Abstract
Background: Nurses are vital healthcare team members and are often underutilised in antimicrobial stewardship (AS) activities. Several nursing responsibilities, such as taking allergy history and obtaining cultures, already overlap with AS activities. Nurses can play a crucial role in promoting AS in resource-limited settings. This study was conducted to assess frontline staff nurses’ baseline attitudes and beliefs towards AS, and see if a virtual education campaign consisting of newsletters and tip sheets would affect those attitudes and beliefs.
Methods: An online survey (pre-survey) was conducted of all in-patient nurses employed in the authors’ hospital on their attitudes and beliefs regarding AS. The survey consisted of 24 questions divided into three domains: demographic and practice information, nursing roles, and beliefs and attitudes towards AS programmes (ASP). After obtaining the results of the pre-survey, the authors started distributing monthly newsletters on various AS topics via email and posting them on a resource page. Topics included how to obtain an accurate allergy history, how to use microbiology results to help guide decisions, and stop therapy in cases of colonisation. The authors also distributed the same survey as a follow-up 6-month survey (post-survey) in March 2021 to gauge the impact of their virtual education efforts.
Results: In total, 109 nurses working in the adult in-patient setting of the authors’ institution completed the pre-survey in September 2020, and 64 nurses completed the post-survey in March 2021. Overall, most nurses had a positive attitude towards AS tasks, and over 90% of those who responded in the pre-survey and post-survey agreed with the statement that nurses are antibiotic stewards, thought it was important or very important to obtain appropriate cultures, and understood the relationship between Clostridioides difficile and antibiotics. Most pre-survey respondents listed knowledge gaps in microbiology (47 out of 64 [86%]) and antibiotics (53 out of 64 [84%]) as well as scope of practice concerns (48 out of 64 [75%]) as barriers to nurse participation. The virtual education helped raise the familiarity with the ASP and more nurses in the post-survey said they were familiar with the stewardship programme compared with the pre-survey (48.4% versus 23.2%; p=0.001).
Conclusions: This study showed that most nurses consider themselves antibiotic stewards and want to participate in AS activities; however, barriers to nursing involvement, such as lack of knowledge, scope of practice concerns, and time constraints, persist. Virtual education may be an option to increase nursing awareness and participation on ASPs in resource-limited settings.
Key Points
1. Nurses are vital healthcare team members who can play an important role in establishing or expanding antimicrobial stewardship (AS) programmes (ASP). However, nurses are often underutilised in AS activities. In addition, barriers to nursing involvement, such as lack of knowledge, scope of practice concerns, and time constraints, persist. This is partly because of the paucity of data on nursing attitudes and barriers towards AS, and because of the limited number of educational training programmes regarding AS that are designed specifically for nurses.
2. This study was conducted to assess frontline staff nurses’ baseline attitudes and beliefs towards AS and to see if a virtual education campaign consisting of newsletters and tip sheets would affect those attitudes and beliefs.
3. In this study, over 90% of the nurses surveyed considered themselves to be antibiotic stewards and wanted to participate in AS activities, such as assessing adverse drug reactions and educating patients. The authors also found that virtual education was effective in increasing the familiarity of frontline nurses with the hospital ASP. A virtual education may be an option to increase nursing awareness and participation in ASP, especially in resource-limited settings.
INTRODUCTION
The World Health Organization (WHO) has designated antimicrobial resistance as one of the top 10 public health threats facing the global community, which requires an urgent and multipronged response.1 Surveillance reports from around the world have shown a rise in multidrug-resistant or pandrug-resistant pathogens, and a decline in the number of effective agents to combat them.2 There are multiple drivers of increasing antimicrobial resistance; however, excessive and inappropriate antimicrobial use has been identified in several studies as a major factor behind the proliferation of drug-resistant bacteria.3-5 According to the Centers for Diseases Control and Prevention (CDC), approximately 30% of the antibiotic prescribing in the USA hospitals is inappropriate.6 In response to the growing threat of drug-resistant bacteria and dwindling number of anti-infective agents available in the market to combat these pathogens, the CDC and the Infectious Diseases Society of America (IDSA) have published several guidelines to encourage the implementation of comprehensive antimicrobial stewardship (AS) programmes (ASP) in healthcare settings;7-9 however, lack of monetary resources and inadequate work force make it a challenge to establish a robust ASP, especially outside the in-patient hospital setting.10
Nurses are vital healthcare team members who can play an important role in establishing or expanding ASPs; however, they are often underutilised.11-14 Although ASPs have been around for the past few decades, most programmes are traditionally made up of infectious diseases physicians, pharmacists, infection prevention specialists, microbiologists, and information technology experts. The nurse role in ASPs has typically been limited to infection prevention nurses or hospital epidemiologists, and their role in ASP is not well-defined.11-15 This is surprising considering the number of studies showing the positive role of nurses in pain management, prescription use, surgical prophylaxis, and sepsis management.16-19 Several nursing responsibilities already overlap with AS activities and they could have a significant impact in promoting AS in settings where monetary and labour resources are scarce.12,13,20 Nurses play a vital role in obtaining allergy history, procuring cultures, reviewing microbiology results, and counselling patients.21,22 Several studies demonstrate the positive impact of collaborating with nurses in order to optimise antibiotic use.21-24 Whether it is reducing the number of unnecessary urine and respiratory cultures, which prevents inappropriate prescribing of antibiotics, or reducing the unnecessary testing for Clostridioides difficile, there are several ways in which nurses have shown to complement existing AS activities.25-27 Nursing involvement in AS is now required by regulatory bodies such as The Joint Commission (TJC) to help combat the threat of antimicrobial resistance in the USA.28
Integrating nurses into the fight against antimicrobial resistance is not without its challenges. Several factors, such as workflow, regulatory requirements, education of healthcare workers, and improvements in clinical practice, need to be considered.29 Benefits of a multidisciplinary team-based approach in improving patient outcomes need to be defined clearly in order to increase nursing participation.30-31 Surveys of nursing attitudes towards AS show that nurses, except for advanced nurse practitioners, do not perceive themselves as antibiotic prescribers and hence are not integral to stewardship efforts.32 Also, studies have shown that 35–62% of nurses were unfamiliar with AS and ASPs at their sites. A survey of 159 nurses in a tertiary medical centre showed gaps in education and identified time constraints and concerns over physician pushback as significant barriers to nurse participation in AS activities.33,34 Studies highlighting the role of nurses as antimicrobial stewards show encouraging signs but also demonstrate the need for formal education or training among the nurses in order to be successful.35-42
Although providing educational content thorough virtual reality or virtual cases is not a novel concept in medical or surgical training, the unexpected crisis of the COVID-19 global pandemic has forced several programmes to quickly adapt to virtual teaching methods in the absence of traditional training.43-46 While some of these programmes have shown promising results, the concept of teaching principles of AS via an online, virtual format is relatively new, especially when it comes to nurses, and there is a paucity of data on this subject.47-51
The authors’ study was conducted to evaluate frontline, bedside staff nurses’ baseline attitudes and beliefs towards AS, and to understand if a virtual education campaign consisting of newsletters and tip sheets would positively impact those attitudes and beliefs.
METHODS
Description of the Education Programme
As multidisciplinary rounds expanded in various units in the authors’ 390-bed community hospital, a programme to integrate frontline nurses into AS was made with help from nursing leadership to utilise a valuable resource already at the patient’s bedside and to reduce duplication of efforts. The AS team at the authors’ institution, consisting of infectious diseases pharmacists, physicians, microbiologists, nurse managers, and infection prevention nurses, wanted to educate bedside nurses regarding AS and incorporate some AS best practices in their standard day-to-day workflow. The authors conducted a baseline survey (pre-survey) of in-patient hospital nurses in September 2020. In this study, face-to-face, live presentations, and professional education were originally planned via in-person conferences and continuing nursing education activities; however, the global COVID-19 pandemic forced the authors to conduct their education strictly via a virtual format. After the results were collected, the nurse managers distributed monthly tip sheets and newsletters (created by the AS pharmacists) via email to all the frontline, in-patient nursing staff. The newsletters focused on various AS topics, such as how and when to collect blood and urine cultures, screen for C. difficile, take an accurate allergy history, differentiate between colonisation and true infections, identify sepsis, and use culture results to help guide decisions to de-escalate or stop therapy in cases of colonisation. After the monthly emails were sent, the nurse managers posted various AS topic content on the nursing homepage. The content of the newsletters was re-enforced during CDC Antibiotic Awareness Week in November 2020 and during the various continuing nursing education accredited webinars and virtual professional development educational activities.
Survey
The authors conducted a baseline survey (pre-survey) of in-patient hospital nurses in September 2020 to assess their beliefs and attitudes towards AS. After a review of the literature on nursing roles relating to AS, a questionnaire draft was created by the principal investigator. The draft was then reviewed by members of the research team with expertise on survey research. Finally, the survey was reviewed for content validity by two members of the nurse leadership and professional development team at the authors’ institution. The review established that the wording of the survey would be understood by potential respondents and verified that the survey questions fell within the nursing scope of practice.
The survey was sent to 800 nurses who work in the adult in-patient departments at the authors’ institution. These nurses belonged to 10 different clinical departments covering intensive care units, medical, surgical, preoperative, and oncology floors. The survey was not randomised but sent to all the in-patient nurses who cover adult wards. Participation in the survey was voluntary, confidential, and anonymous. The survey consisted of 24 questions broken down into three broad domains: demographic and practice information, questions on nursing roles in AS, and nursing attitudes and barriers towards AS.
Demographic questions included where the nurses practised, their level of education, and their years of experience. Assessment of the role of nurses in AS included comfort level in participation in various AS activities, such as obtaining cultures properly and understanding the relationship between antibiotics and C. difficile. The concluding section focused on assessing the beliefs and attitudes towards AS.
The survey was distributed to all in-patient nurses via Microsoft Office Forms (Microsoft, Redmond, Washington, USA), which is the format that has been used in the past by the nursing leadership at the authors’ institution. The authors provided the respondents with 2 weeks to complete the survey and sent a weekly and final reminder before it was closed. A subsequent post-survey was sent to the same group of in-patient frontline nurses in March 2021.
The survey results were not matched since the data were deidentified and anonymous. No incentives were provided for the completion of the survey. The hospital’s institutional review board approved the study in August 2020, before the first survey was sent out.
Statistics
Summary statistics for the pre- and post-survey data were calculated as counts and percentages. The demographic factors were compared between the pre- and post-survey to assess whether there was a relationship between the factors and survey groups. Given the small counts in some of the categories of the demographic factors, Fisher’s exact test was utilised for the comparisons. A p value of >0.05 indicates that the participants for the pre- and post-survey were similar based on the demographics. The questions regarding nursing attitudes towards AS tasks and nursing awareness of AS, with responses to the Likert scale of ‘Not important at all’ to ‘Very important’, were compared between the pre- and post-survey using the Wilcoxon rank sum test. Each of the Likert scale questions were coded in the following way for analysis: ‘Not Important at All’=1, ‘Unimportant’=2, ‘Neither’=3, ‘Important’=4, and ‘Very Important’=5. Summary statistics for each question were calculated using median, minimum, and maximum values. The Wilcoxon rank sum test was used to ascertain whether there was a significant difference in participants’ view of the importance of the tasks between the pre- versus post-survey as responses were not paired across both surveys. The significance level was α=0.05. All statistical analyses were conducted using R version 4.1.1 (R Foundation for Statistical Computing, Vienna, Austria).52
RESULTS
In total, 109 nurses responded to the baseline pre-survey, which was distributed in September 2020, and 64 nurses responded for the post-survey, which was conducted in March 2021. The baseline demographics were similar between the pre-and post-survey group regarding education and primary responsibility as a nurse. All specialties, such as the intensive care unit, medical, and surgical nurses, were well-represented, with the majority of survey respondents being frontline staff nurses holding a bachelor’s degree. Overall, most nurses demonstrated a positive attitude towards antimicrobial stewardship tasks. For example, 97.9% of those who responded in the pre-survey thought it was ‘Important’ (Likert scale: 4) or ‘Very Important’ (Likert scale: 5) to obtain appropriate cultures. Other AS tasks, such as assessing adverse drug reactions, educating patients, and understanding the relationship between C. difficile and antibiotics, were also viewed as ‘Important’ (Likert scale: 4) or ‘Very Important’ (Likert scale: 5) by over 90% of the nurses in both the pre- and post-survey (Figure 1). In addition, 93.8% of the nurses surveyed agreed with the statement that nurses are antibiotic stewards (Figure 2). Most pre-survey respondents listed knowledge gaps in microbiology (47 out of 64 [86%]) and antibiotics (53 out of 64 [84%]) as well as scope of practice concerns (48 out of 64 [75%]) as barriers to nurse participation.
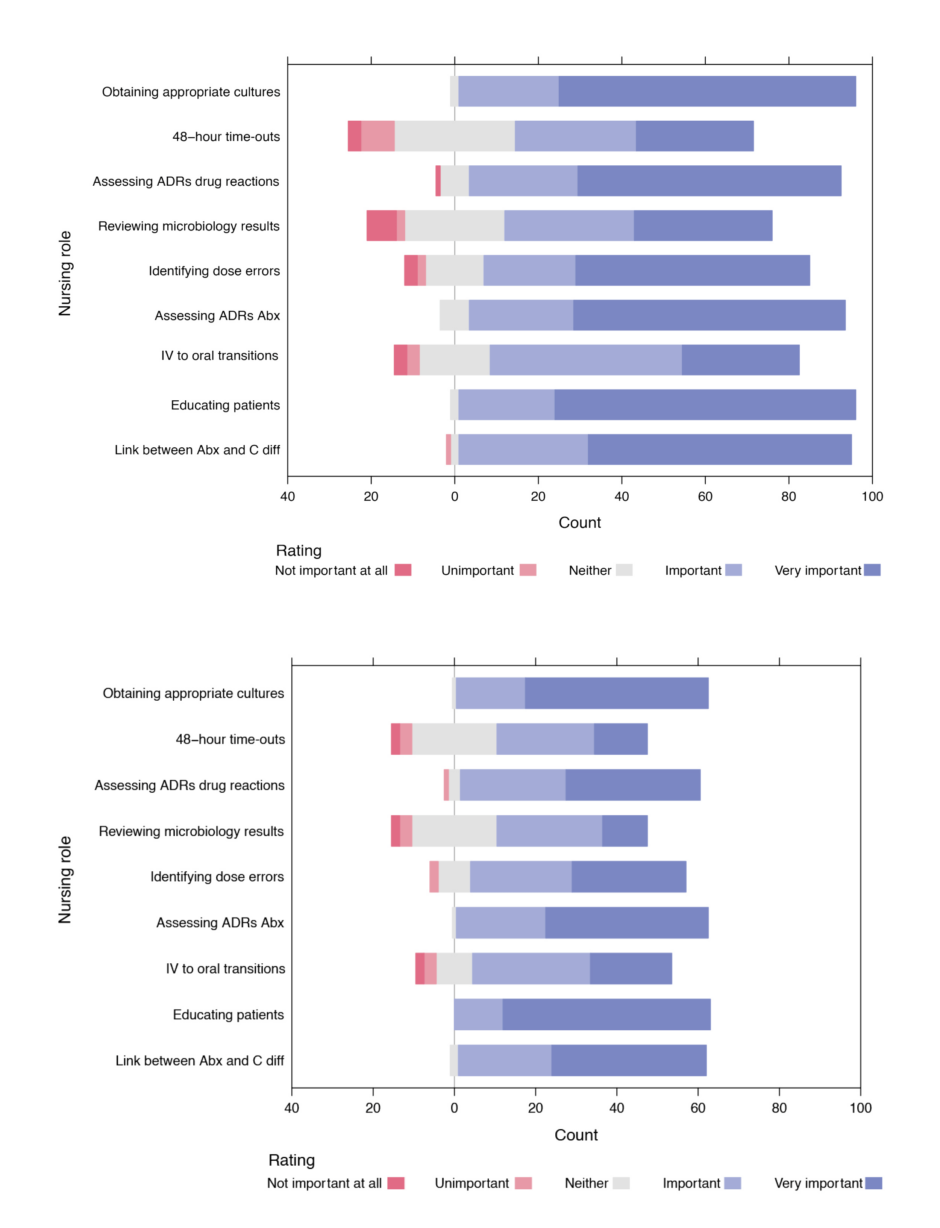
Figure 1: A) Pre-survey nursing attitudes towards antimicrobial stewardship and B) a post-survey nursing attitudes towards antimicrobial stewardship.
Abx: antibiotics; ADRs: adverse drug reactions; C diff: Clostridium difficile; IV: intravenous.
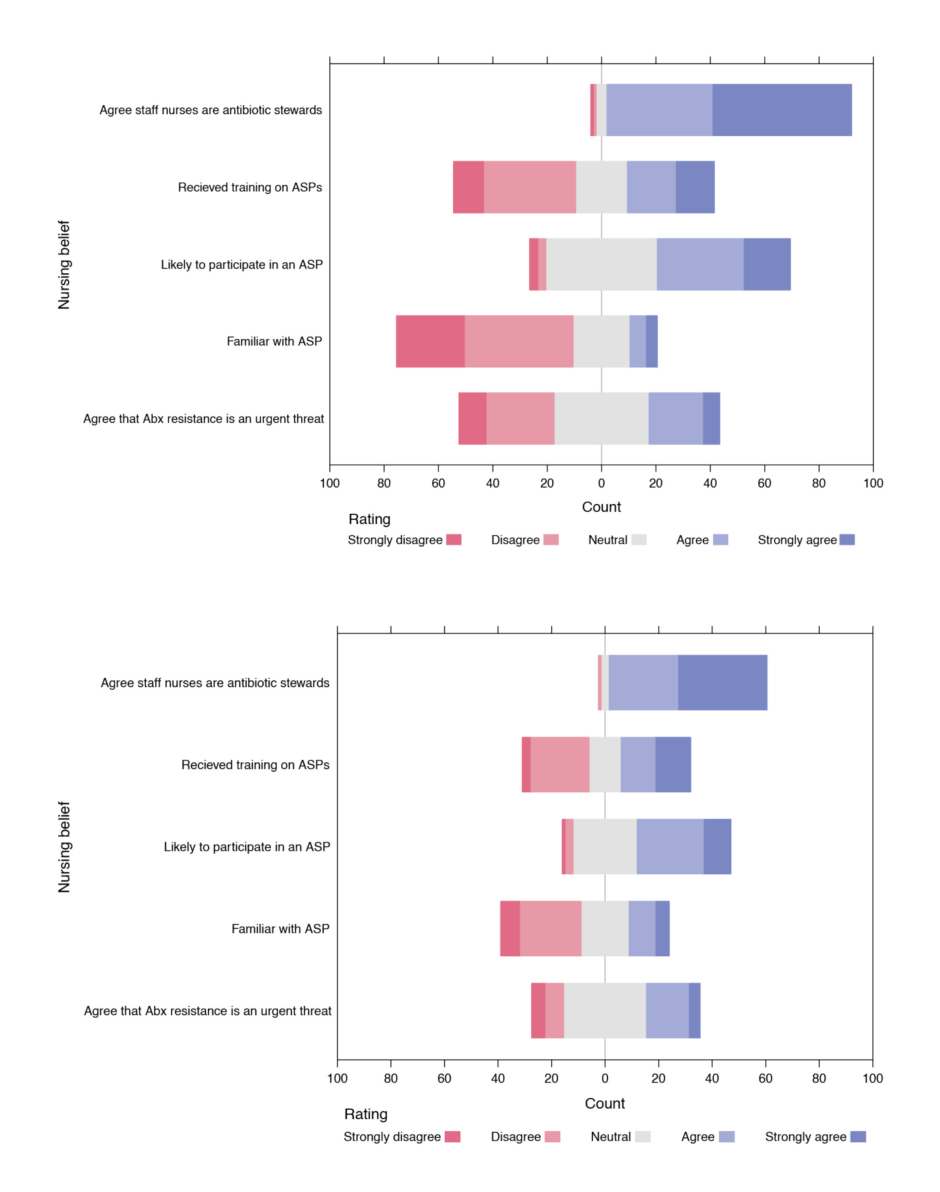
Figure 2: A) Pre-survey nursing awareness of antimicrobial stewardship and B) post-survey nursing awareness of antimicrobial stewardship.
Abx: antibiotics; ASP: antibiotic stewardship programme.
The nontraditional, virtual education was effective in increasing the familiarity of the frontline nurses with the hospital ASP, as significantly more nurses in the post-survey reported that they were familiar with the stewardship programme compared with the pre-survey (31 out of 64 [48.4%] versus 24 out of 109 [23%]; p=0.001). Although not statistically significant, there was also a slight improvement in nursing attitudes towards evaluating a history of adverse drug reactions (median Likert score=5; p=0.17) and learning about the relationship between antibiotics and C. difficile (median Likert score=5; p=0.5) (Table 1). In terms of awareness of AS issues, a majority of nurses (51% in pre-survey versus 55.6 % in the post-survey) were likely to participate in ASP (Figure 2); however, despite education on the rationale and how to apply the recommended tasks to nursing practice, no change was demonstrated in perceived barriers to nurse participation in AS activities.
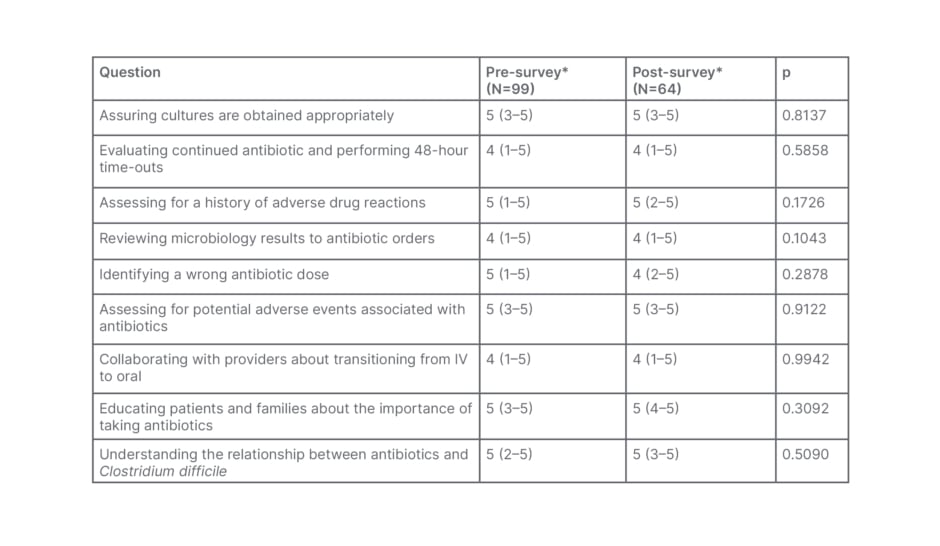
Table 1: Comparison of nursing attitudes towards antimicrobial stewardship tasks between the pre- and post-survey.
*Likert scale responses were coded in the following way: ‘Not Important at All’=1; ‘Unimportant’=2; ‘Neither’=3; ‘Important’=4; and ‘Very Important’=5. Data are presented as median (minimum–maximum).
IV: intravenous.
DISCUSSION
The results of the authors’ survey showed that most nurses were aware of the urgent threat of antimicrobial resistance and want to contribute to a stewardship programme. Nevertheless, lack of education (especially in microbiology and antimicrobial spectrum of activity) and range of practice concerns were perceived as the most common impediments to participation. While not statistically significant, the virtual education campaign showed a positive impact on nurses’ attitudes and beliefs on AS, and may be used as a blueprint moving forward in resource-limited settings.
Data on education for nurses on the topic of AS remains limited. Abbas et al.33 surveyed 159 nurses in an 860-bed tertiary medical centre with an established ASP. They showed that while 62% of the respondents knew about the programme, time constraints, and concerns over physician pushback were identified as significant barriers to nurse participation. Bouchoucha et al.53 surveyed 321 nursing students who were enrolled in an Australian university on their awareness and attitudes regarding the nurse’s role in AS. Their survey found that while 45% of participants were familiar with the terminology of AS, 71% believed they had very little knowledge of the principles of AS. Merrill et al.54 also found comparable results when conducting an online survey of 316 staff nurses from three hospitals. A total of 52% of nurses did not recognise the term AS; however, almost 40% of nurses in the survey suggested that an ASP was moderately or extremely important in their healthcare setting.54
In the UK, efforts are underway to develop national consensus-based competencies to integrate AS education in undergraduate healthcare education. Courtney et al.55,56 identified that only 67% of nursing programmes in the UK incorporate any AS teaching and only a handful (12%) actually go over all the recommended AS principles. A modified Delphi methodology involving two surveys (conducted online), delivered to an international panel of 15 experts, was utilised. These experts in education and AS provided the international consensus on the AS proficiency curriculum appropriate for nursing education.57 The competencies developed will be used to guide future curricula in nursing schools. A total of 95% of the nurses in this study believed they should participate in AS interventions. Results from various previous studies and the authors’ own study make it clear that nurses are aware of the urgent peril of antimicrobial resistance and would like to participate in AS actions but the main barrier is a lack of education.35-42 The format of education is also important.58-60 Interestingly, data shows that nurses learn better by researching
questions themselves or asking their peers rather than formal education.61 Hands-on training, using a collaborative approach, involving nursing leaders, and empowering nurses to be a member of the antimicrobial team, may help improve nurse confidence in AS activities and lead to improved outcomes.62-68
The advantages of a virtual structure are that it is much easier to disseminate and it is a lower-cost option. For example, study materials can be made available in a virtual format (self-study modules, pre-recorded webinars, newsletters, or tip sheets). These can be disseminated with minimal effort to all incoming staff upon hiring and continuing education of nurses. In addition, nurses can receive the same AS training as other healthcare workers, such as physicians and pharmacists, to be effective stewards in their day-to-day practice. Manning et al.50 evaluated the impact of a virtual case-based simulation experience on nursing students and found improvement in knowledge domains regarding antibiotic use and resistance.
According to the USA healthcare workforce statistics, nurses practise in every healthcare setting, including nursing homes, clinics, dialysis centres, and long-term care facilities.14 Therefore, empowering nurses to fight antimicrobial resistance will likely have a significant impact on reducing the inappropriate overutilisation of antibiotics and lessen the burden of antimicrobial resistance.
Limitations
This was a single-centre study conducted during a global pandemic. During this time, there was significant turnover in staff, and several staff nurses were cross-covering several units during the study period. Furthermore, since the survey was anonymous, the authors could not match data to look at the impact of education on an individual level or collect any feedback related to education.
CONCLUSION
In the authors’ study, more than 90% of nurses agreed with the statement that staff nurses are antibiotic stewards, and more than 50% said they are likely to participate in some activities pertaining to AS; however, many barriers to nursing involvement, such as lack of education, range of practice concerns, and time constraints, persist. When real-time, face-to-face instruction is not feasible, as was the case in the COVID-19 era, virtual education via email and newsletters may be used instead of conventional methods to advance participation of nurses in AS projects in a resource limited setting.








