BACKGROUND AND AIMS
During the COVID-19 pandemic, non-pharmaceutical interventions suppressed the circulation of many respiratory viruses, including respiratory syncytial virus (RSV).1,2 Thus, the expected winter season of 2020/21 did not appear in Denmark. However, as restrictions were lifted during spring 2021, an unusually large RSV epidemic occurred in the summer/autumn of 2021. The aim of this study was to compare the RSV summer/autumn epidemic with previous winter seasons using national Danish registries.
MATERIALS AND METHODS
A retrospective, register-based study was conducted to analyse the occurrence of RSV in the Danish population in three typical pre-COVID-19 RSV seasons (2017/18, 2018/19, and 2019/20) in comparison to the unusual RSV epidemic during the summer/autumn of 2021. Laboratory-confirmed RSV cases were identified using the Danish Microbiology Database (MiBa).3 Cases were linked to the National Patient Register4 to identify RSV-related admissions and patients receiving intensive care treatment (ICT) during an RSV-related admission. Seasonal incidence rates (IR) per 1,000 person-years of RSV cases, RSV-related admissions, and ICT were calculated with 95% confidence interval (CI) for each season, stratified by age group. The seasonal IRs were compared by calculating IR ratios (IRR) with 95% CI using the 2017/18 season as reference. Finally, to explore if a more severe type of RSV was circulating in the summer/autumn, the relative risk (RR) of a case being admitted to hospital and an admitted case receiving ICT was calculated with 95% CI using the 2017/18 season as reference.
RESULTS
For the summer/autumn epidemic, IRs of RSV cases exceeded previous winter seasons for all age groups. Compared with the winter season of 2017/18, the highest IRRs of cases in the summer/autumn epidemic were detected among children aged 2–3 years and 4–5 years, with IRRs of 5.5 (95% CI: 4.9–6.2) and 4.2 (95% CI: 3.3–5.4), respectively (Figure 1). For hospital admissions, IRs were significantly higher in the summer/autumn epidemic than in the 2017/18 season, except for the age groups of 6–14 years and ≥65 years. The highest IRRs were detected in children aged 2–3 years and 4–5 years, with 3.7 (95% CI: 3.0–4.6) and 4.3 (95% CI: 2.6–7.1), respectively.
The risk of a case being admitted in the summer/autumn epidemic compared with the winter season of 2017/18 was significantly lower in most age groups. This was especially the case for children ≤5 years, where RRs ranged between 0.6 (95% CI: 0.4–0.6) and 0.9 (95% CI: 0.8–0.9), suggesting that the cases detected in the summer/autumn epidemic were milder than in previous seasons.
The risk of an admitted case receiving ICT was only significantly higher in the summer/autumn epidemic than in the 2017/18 season for children aged 3–5 months and children aged 2–3 years with RRs of 1.5 (95% CI: 1.1–2.1) and 2.3 (95% CI: 1.1–4.8), respectively.
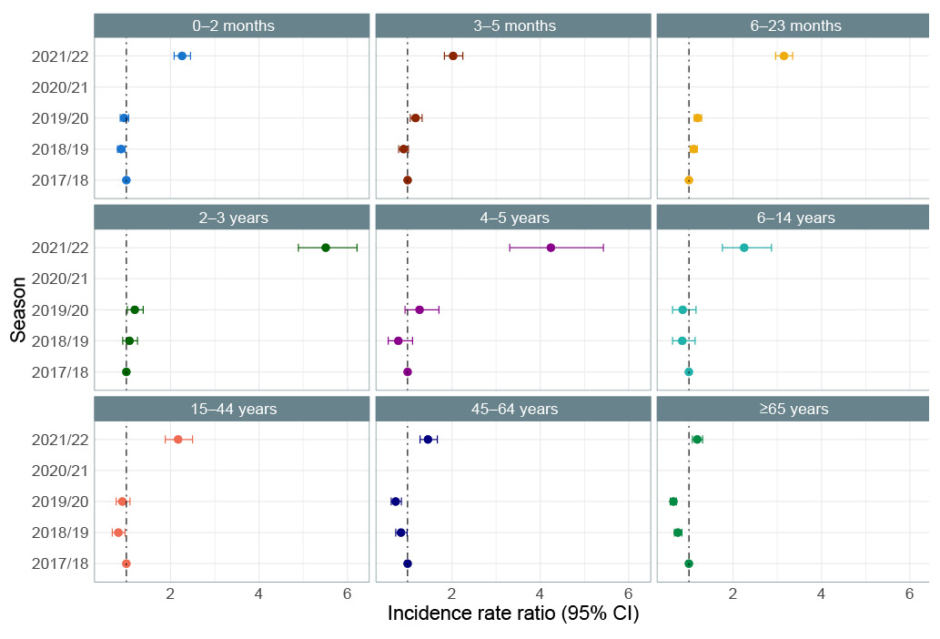
Figure 1: Incidence rate ratio of respiratory syncytial virus cases by season and age group using the 2017/18 season as the reference season.
CI: confidence interval.
CONCLUSION
The summer/autumn RSV epidemic of 2021 was considerably larger than previous RSV winter seasons in terms of both confirmed cases and hospital admissions. A shift in age groups affected by RSV was observed, most prominently in children who are 2–5 years old. The authors speculate that this age shift may be explained by an immunity debt due to suppression of RSV in the winter of 2021. Further, there were no indications that the specific RSV type circulating in the summer/autumn epidemic of 2021 per se caused more severe disease as the risk of a case being admitted was lower and the risk of an admitted case receiving ICT was similar when compared to previous winter seasons.








