INTRODUCTION
Human T-lymphotropic virus type 1 (HTLV-1) is a retrovirus associated with significant immunological dysregulation and oncogenesis.1 It is highly endemic in South America, notably in Brazil, Peru, and Colombia, affecting primarily individuals of indigenous and African descent.2 In children, HTLV-1 often presents with dermatologic manifestations, respiratory diseases, opportunistic co-infections, and autoimmune disorders.3 The virus primarily targets CD4+ T lymphocytes but can also infect CD8+ T cells, B cells, and other immune cell types.4 Transmission occurs mainly through prolonged breastfeeding, sexual contact, blood transfusions, and needle sharing.5 This study aims to describe the immunological profile of pediatric patients diagnosed with HTLV-1 in Cali, Colombia, focusing on cellular and humoral responses.
METHODS
This observational, descriptive, and retrospective cross-sectional study was conducted at a pediatric referral center from January 2017–March 2021. Nineteen pediatric patients with confirmed HTLV-1 infection were included. The median age at diagnosis was 94 months, with school-age children representing the largest group (52.6%). The analysis involved lymphocyte subpopulations (CD4+, CD8+, CD19+, CD3+) and serum immunoglobulin levels (IgA, IgG, IgM, IgE), interpreted according to age-specific reference values. Data were collected from medical records and analyzed using IBM® SPSS® Statistics 22 (Armonk, New York).
RESULTS
Of the 19 patients, 57.9% were male, and 84.2% were affiliated with the subsidized health insurance system. Malnutrition was observed in 52.6% of the cases, suggesting a potential risk factor for immune dysfunction. No cases of HIV co-infection were found. Cellular immunity analysis in six patients revealed that 50% had elevated B lymphocytes (CD19), while CD4+ and CD8+ T cell counts were within normal ranges for most patients. Regarding humoral immunity, 16 patients were evaluated, with elevated IgA, IgG, and IgE levels in over half of the patients, while IgM was normal in 81.3% of cases (Table 1). The increase in immunoglobulin levels, particularly IgE and IgA, was associated with elevated CD19+ B lymphocytes, suggesting a link between B cell activation and polyclonal hypergammaglobulinemia.
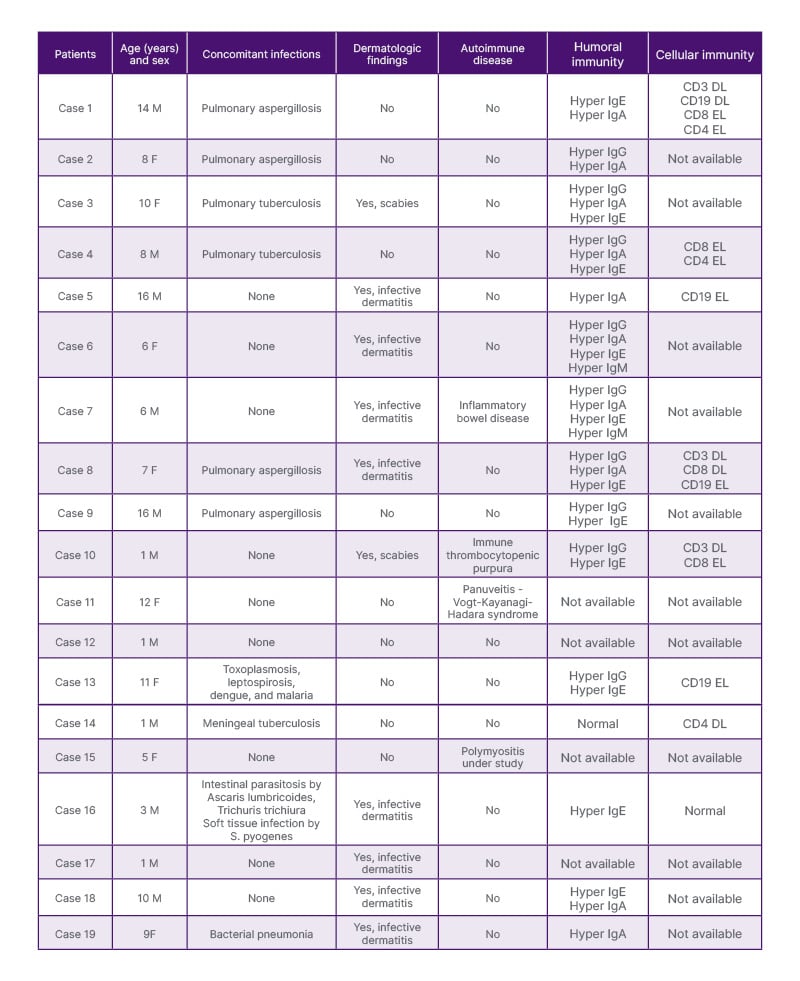
Table 1: Clinical characteristics and immunological profile of patients with HTLV-1 in the present study.
F: female; M: male.
DISCUSSION
The findings indicate that immunosuppression in pediatric HTLV-1 patients is not related to reduced lymphocyte subpopulations but may be mediated by cytokine dysregulation and viral regulatory proteins that interfere with immune signaling.4 This immune dysregulation contributes to increased susceptibility to opportunistic infections such as Strongyloides stercoralis, Aspergillus fumigatus, and Mycobacterium tuberculosis.6 Pulmonary infections, including tuberculosis and aspergillosis, along with dermatological conditions like infective dermatitis, were common opportunistic manifestations.7 The male predominance observed contrasts with studies reporting a higher prevalence in females.8 Consistent with prior research, this study identified polyclonal hypergammaglobulinemia rather than lymphopenia, reflecting an aberrant but functional immune response.9 Additionally, the elevated immunoglobulin levels and B lymphocytes suggest a possible link to immune system overstimulation rather than depletion.10
CONCLUSION
Pediatric patients with HTLV-1 infection exhibit elevated B lymphocytes and immunoglobulin levels, indicating immune dysregulation driven by cytokine alterations rather than lymphocyte depletion.2 Enhanced monitoring for opportunistic infections and regular immunological assessments are recommended to improve outcomes. Future studies should focus on understanding immune activation mechanisms and developing therapeutic interventions that address pediatric HTLV-1 infection.5







