BACKGROUND
In countries without universal vaccination for chickenpox in childhood, a very high seroprevalence for varicella zoster virus (VZV) IgG in adults is often assumed.Consequently, some suggest vaccinating at-risk adults against herpes zoster, even if they lack a documented history of chickenpox, under the assumption of immunity.1,2 However, this presumption may not accurately reflect today’s epidemiological landscape.3,4 Neglecting the risk of primary infection post-childhood could lead to severe outcomes in vulnerable adults,5 pregnant patients,6 and increase the likelihood of exposure for caregivers, potentially resulting in secondary transmission.7
METHODS
A retrospective study was conducted on VZV serology among individuals aged 11 years and above, from February 2014–March 2024, who were unvaccinated and lacked known chickenpox history, within a Portuguese hospital.
RESULTS
Analysis of 613 patients (68% women; median age: 39 years) with high VZV infection risk due to comorbidities or immunosuppression revealed an 83.6% VZV IgG positivity rate, increasing with age (Figure 1). Among working-age individuals aged 21–60 years, 12% were seronegative for VZV, and 19.2% of women aged 16–40 years showed no immunity.
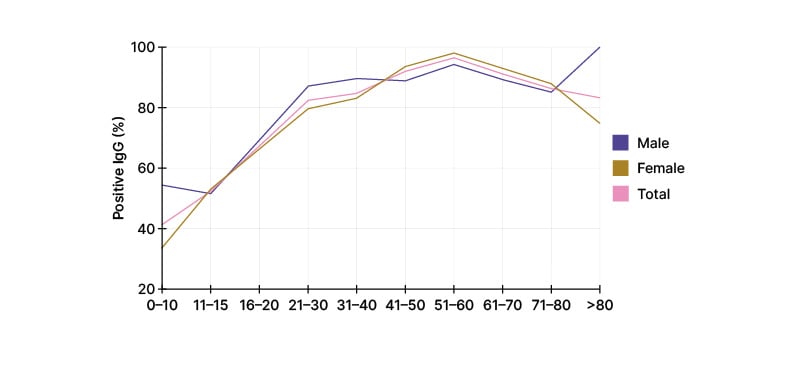
Figure 1: Varicella zoster virus IgG seroprevalence by gender and age group.
CONCLUSION
Although common, the presence of antibodies against VZV is not universal after childhood in unvaccinated populations. Vaccination for herpes zoster is not indicated for the prevention of primary infection, so assuming immunity may fail to prevent it in a population at risk.
Prevention of chickenpox relies on specific vaccination, or the use of immunoglobulin when the former is contraindicated, which implies recognition of this susceptibility. Serology remains a useful tool, especially for at-risk individuals and caregivers.







