BACKGROUND
UK Escherichia coli (E. coli) sepsis rates have been rising for the last 20 years, however the reason behind the consistent year on year increase is an enigma. Good information on the rates of increase are available from the Public Health England, Wales, and Scotland agencies. E. coli bacteraemia (blood infection) rates have been closely monitored since mandatory surveillance was initiated for acute NHS trusts in 2011. For example, rates have risen by 49% in Wales (60.3–89.8 per 100,000 population from 2010–2017),1 71% in England (45.0–77.7 per 100,000, 2009–2018),2,3 and 31% in Scotland (66.6–87.3 per 100,000, 2009–2018).4 However, the reason behind this increase is, to date, unknown. The sepsis rate also varies greatly between NHS geographic regions and considerably between London (64/100,000) and South Wales (85/100,000). The authors hypothesised that the different rates could be due to differing prevalence of pathogenic E. coli types in the different UK NHS regions.
METHODS
The authors investigated the common E. coli strains in the community at several UK locations by sampling sewage on entry to waste water treatment plants at multiple sites: Longreach (about 20 km east of London on the Thames), Marlow (Buckinghamshire), Reading (Berkshire), Bristol (Avon), Ponthir (South Wales), and Cardiff (South Wales) sewage works from 19.9.2019–26.9.2019. These samples were diluted and streaked on chromogenic UTI agar (no antibiotics) and approximately 100 E. coli isolates were chosen from each location. Species was confirmed by matrix-assisted laser desorption/ionisation-time-of-flight mass spectrometry and susceptibility determined by disc diffusion (European Committee on Antimicrobial Susceptibility Testing [EUCAST] methodology). The phylotype was determined by multiplex PCR (Clermont method). Each pathogenic B2 isolate was further tested for known common sepsis sequence types (ST): ST131, ST73, ST95, and ST69 by multiplex PCR (Doumith method).
RESULTS
The prevalence of pathogenic B2 phylotype E. coli was considerably higher in South Wales than in England (32.5% versus 17.8%), reflecting the differing sepsis rates between the two countries. B2 phylogenetic prevalence at each location was 33.0% (Ponthir), 32.0% (Cardiff), 24.0% (Bristol), 12.0% (Reading), 17.0% (Marlow), and 18.0% (Longreach). Prevalence was lowest in the London region (15.6%), an average of the sites that were all within 40 miles of central London, i.e., Reading, Marlow, and Longreach. The multiplex PCR for detecting known sepsis-causing pathogenic E. coli ST95, ST131, ST73, and ST69 detected one or more of these ST at all locations (Table 1).
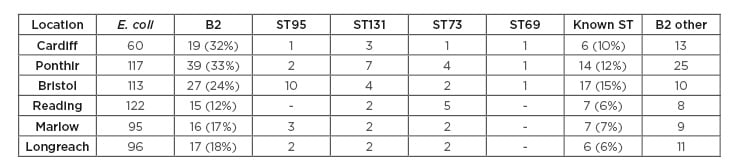
Table 1: Sepsis-causing pathogenic Escherichia coli strain distribution across different geographical sites.
coli: Escherichia coli; ST: sequence type.
The prevalence of these specific ST was also higher in Wales than in England (11% versus 8.5%). The highest rate of specific sepsis E. coli ST was found in Bristol mostly due to a very high prevalence of ST95 (8.8%) in the community. However, overall Bristol had less of a diversity of sepsis causing ST as compared to the Welsh sites, with several additional sepsis-causing types commonly found in Wales.
CONCLUSION
This study demonstrates that: 1) human carriage of pathogenic B2 E. coli phylotypes is very high in the UK, especially in Wales; 2) specific ST within the B2 phylotype, known to be the cause of E. coli sepsis in hospitals across the nation, are commonly carried in the human gut; and 3) carriage rate is related to sepsis rate. Taken together, this information suggests a rational explanation of the rising sepsis rates in the UK, i.e., they are directly related to increasing carriage rates of virulent E. coli strains in the community.








