Interview Summary
Coronary interventions, and specifically the number of percutaneous coronary intervention (PCI) procedures, are increasing, together with their complexity. Contrast media administration during those procedures assists in visualising vessels anatomy, but also increases the risk of contrast-induced nephropathy (CIN), which remains one of the most common complications, and has been associated with poor clinical outcomes.
Dynamic Coronary Roadmap (DCR) is a technology that creates a dynamic, motion-compensated, real-time view of the coronary anatomy overlaid on a 2D fluoroscopic image, creating a coloured map that adjusts automatically, and providing continuous visual feedback on the positioning of wires and catheters.
The technology, which is already being used in clinical practice, has posed the promise of not only assisting in navigating wires and catheters, but also reducing the use of contrast during PCI.
DCR4Contrast was a randomised clinical trial conducted in the USA, Europe, and Israel that enrolled more than 356 patients. The primary endpoint for the study was the reduction in contrast administered with the use of DCR, compared with the control group. The secondary endpoint was the potential reduction in the number of cineangiography runs.
In the trial, DCR reduced the total contrast volume per PCI procedure by an average of 28.8%, and reduced the number of contrast-enhanced cineangiography runs per procedure by 26.3%.
It was also demonstrated that the more complex the PCI procedure, the larger the reduction in contrast with DCR.
Here, interventional cardiology experts discussed the need for contrast reduction, and the evidence for DCR.
INTRODUCTION
PCI is a minimally invasive, non-surgical procedure that aims to relieve the narrowing or occlusion of a coronary artery through the insertion and inflation of a balloon catheter or a stent.1
Approximately 30% of PCIs are considered complex.2 The use of PCI in complex disease is increasing due to the introduction of drug-eluting stents and improvements in implantation techniques and medical therapy.2 Part of this complexity is related to age, as well as medical comorbidities, such as obesity, Type 2 diabetes, hypertension, and hyperlipidaemia.2-4
PCI requires the use of iodinated contrast to define the coronary anatomy and to guide the navigation of dedicated equipment, such as guidewires, balloons, and stents. It has been demonstrated that contrast volume is directly associated with the risk of CIN, which remains one of the most common and serious complications of procedures involving contrast administration. CIN has been associated with poorer clinical outcomes, including mortality, as well as longer hospital stays, higher readmission rates, and a greater economic burden.5
Since CIN can significantly impact prognosis, clinicians are seeking ways to minimise the contrast volumes used during PCI, thereby increasing procedural safety. To support these aims, Philips (Amsterdam, the Netherlands) has developed DCR, a PCI navigation support tool.
WHAT IS THE DYNAMIC CORONARY ROADMAP?
DCR creates a dynamic, motion-compensated, real-time view of the coronary arteries. The system overlays a highlighted coronary angiogram on a 2D fluoroscopic image, creating a coloured map that adjusts automatically, and providing continuous and specific visual feedback on the positioning of wires and catheters (Figure 1).
This coloured roadmap compensates for heart and respiratory motions, and is generated from previously acquired coronary angiograms during the procedure.
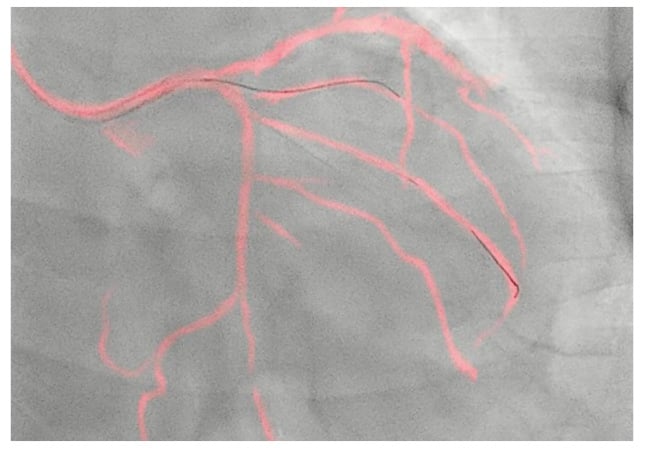
Figure 1: Dynamic Coronary Roadmap as displayed on the live X-ray system screen.
HOW THE DYNAMIC CORONARY ROADMAP HELPS TO ANSWER KEY CHALLENGES IN PERCUTANEOUS CORONARY INTERVENTION PROCEDURES
Although coronary catheterisation has become a common procedure for the diagnosis and treatment of patients with coronary artery disease, imaging the vessels and navigating to the area of interest (through the coronary tree) while advancing guidewires and specific devices (e.g., for intracoronary imaging, physiology, or vessel preparation), may still pose challenges to the operating interventional cardiologist.
These challenges can be addressed by injecting additional contrast media (small ‘puffs’ of contrast), to better visualise the vessels; however, this raises the risk of CIN. There is a need to solve the tension between increasing the probability of procedural success and maintaining patient safety, said Ajay Kirtane, Chief Academic Officer at Columbia Interventional Cardiovascular Care, Columbia University Irving Medical Center (CUIMC), New York City, New York, USA, and Director of the Cardiac Catheterization Laboratory, New York-Presbyterian (NYP)/CUIMC, New York City, New York, USA.
The randomised DCR4Contrast trial was conducted to determine whether DCR could assist physicians in relieving this tension.6
DCR4Contrast TRIAL
The framework for the study, as described by principal investigator Javier Escaned, Head of the Interventional Cardiology Section at Hospital Clínico San Carlos, Madrid, Spain, was reducing contrast use during PCI, also referred to as ultra-low contrast PCI. Escaned noted that ultra-low contrast PCI is highly important in patients who are particularly sensitive to iodine contrast, as they may develop CIN.6
The study was a randomised clinical trial that allocated patients to two arms: PCI performed in the conventional way (guided by angiography) or PCI guided by DCR.
The study was conducted in more than 356 patients in the USA, Europe, and Israel. The primary endpoint was the reduction in contrast administered with the use of DCR compared with the control group. The secondary endpoint was the potential reduction in the number of cineangiography runs, which expose patients and staff to X-ray radiation.6
Trial Results and Their Impact
The trial demonstrated that DCR reduced the total iodine contrast volume per PCI procedure by 26.2 mL (p<0.001), or an average of 28.8% (95% confidence interval: 18.9–38.2%), as presented by Escaned, in a late-breaking trial session at EuroPCR 2023 (Figure 2).7 For the secondary endpoint, DCR reduced the number of contrast-enhanced cineangiograms per PCI procedure by an average of three runs, based on a procedure with an average of 11 runs, which corresponds to a 26.3% reduction (95% confidence interval: 16.8–35.1%; Figure 2).
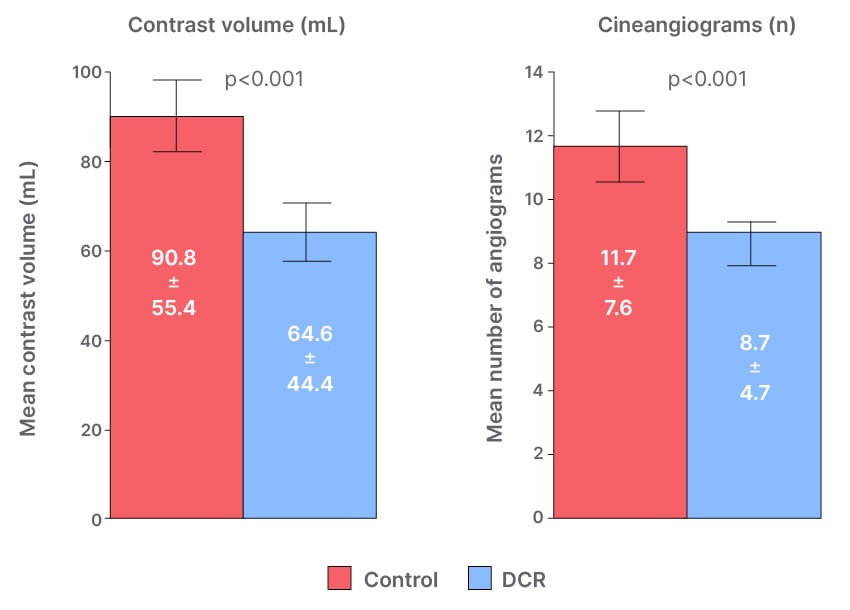
Figure 2: Primary and secondary endpoints of the DCR4Contrast trial.7
DCR: Dynamic Coronary Roadmap.
The complexity of PCI was obtained by calculating the SYNTAX Score for each treated vessel. The trial showed that the more complex the PCI was, the larger the contrast reduction with DCR (Figure 3).6,7 Escaned noted that complex PCI procedures generally require greater use of contrast, and said that the results of the trial indicated that patients with complex lesions would potentially benefit the most from the use of DCR during PCI.6
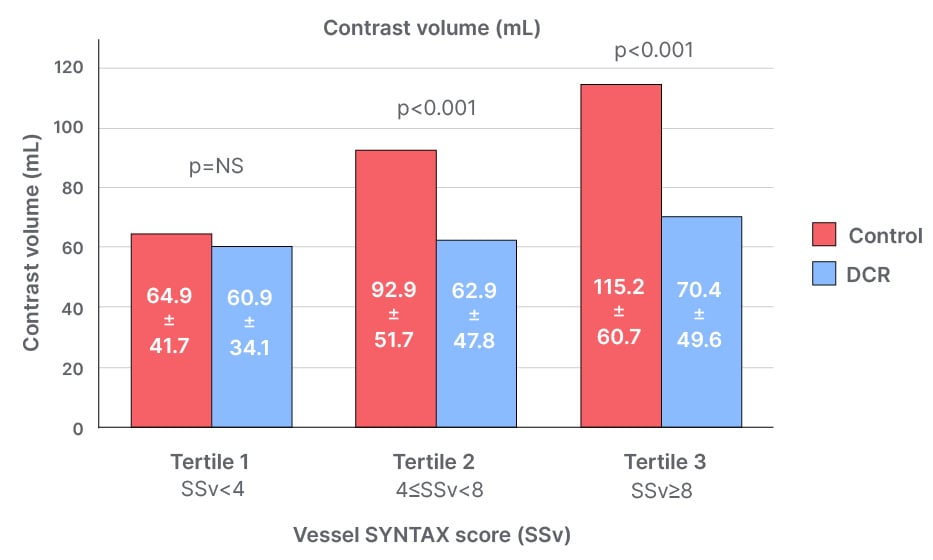
Figure 3: Contrast volume used according to tertiles of SYNTAX Score.7
DCR: Dynamic Coronary Roadmap; NS: not significant; SSv: vessel SYNTAX Score.
“Enabling physicians to decrease contrast administration during procedures with tools like DCR could make a significant contribution to both the safety and quality of PCI. This is important at a time when PCI is increasingly used in patients with a complex clinical or anatomical profile,” said Escaned.
“These results are very exciting,” commented John Messenger, Clinical Director, Heart and Vascular Center, University of Colorado Hospital, Denver, USA, who presented a secondary analysis of the DCR4Contrast trial at the Society for Cardiovascular Angiography & Interventions (SCAI) 2023 Scientific Sessions in Phoenix, Arizona, USA.8 “They confirm that this technology can be applied to all PCIs, and has the potential to increase overall PCI safety by mitigating one of the few preventable contributors (iodinated contrast media use) to contrast-induced acute kidney injury following PCI.”
“From the initial recruitment, it was clear that the system improves the safety and efficacy of coronary angioplasty, reducing radiation and the use of contrast,” said Haim Danenberg, Director of Interventional Cardiology, Wolfson Medical Center, Holon, Israel.
In a secondary analysis of the DCR4Contrast trial, the overall quality of the roadmap displayed by DCR was rated by investigators as good/very good in 79% of the cases.8
IMPACT ON DAILY PRACTICE
Aaron Strobel, Interventional Cardiologist at Baptist Health Heart Institute and Arkansas Cardiology Clinic, both in Little Rock, Arkansas, USA, said: “DCR is a great asset to add to the interventional toolkit; [it is] an easy-to-use tool, which reduces the contrast exposure to patients. It is very useful in patients with low glomerular filtration rate, or patients with branch vessel disease. I use it very frequently to assist in decreasing contrast use.”
Danenberg agreed: “It became routine in almost every coronary angioplasty I perform. Very simple to use with clear benefit and no downside.”
CONCLUSION
Escaned concluded: “Hopefully this will be one additional tool in guiding our PCI procedures, not only on angiography, but also together with relying more on intracoronary imaging, intracoronary physiology, even coronary images that have been obtained from CT angiography, and from previous angiograms.6 All to support and assist in maintaining patient safety, while maximising procedural outcomes.”







