AIMS
Due to the difficulty of accessing small diameter vessels, modern transcatheter technologies remain problematic in the treatment of ischaemic stroke resulting from intracerebral atherosclerotic lesions. This research is dedicated to the possible treatment of patients with ischaemic stroke by means of transcutaneous transcatheter endovascular surgery.
METHODS AND RESULTS
The research involved 798 patients aged 29–81 years (mean age 73 years), predominantly with intracerebral atherosclerosis, after ischaemic stroke: males 591 (74.06%), females 207 (25.94%). The evaluation of the clinical dementia rating, mini-mental state examination, and the Barthel index (BI) were conducted using the following methods; computed tomography, magnetic resonance imaging, magnetic resonance angiography, scintigraphy, rheoencephalography, and cerebral multigated acquisition scan:
- macrofocal strokes were detected in 134 (16.79%) patients
- midfocal strokes were detected in 390 (48.87) patients
- microfocal strokes were found in 274 (34.34%) patients
Transcatheter interventions were conducted in 487 (61.03%) patients in a test group. To perform transcatheter revascularisation of the main intracerebral arteries, high-energy pulsed lasers were used for revascularisation of distal intracerebral branches (continuous low-energy lasers [Patent US 7490612]). By transfemoral access and with the use of multiple conductive catheters, a flexible fibre-optic laser instrument with a diameter of 50–200 mm was guided through the carotid artery to the territory of the intracerebral atherosclerotic lesions, which was then followed by laser irradiation. While the laser apparatus was at work, the fibre-optic instrument was washed with physiologic saline thereby eliminating the blood and creating a transparent environment for laser irradiation. Conservative treatments including desagregate, anticoagulant, vasodilatory, antioxidant, and nootropic therapy were conducted in 311 (38.97%) patients in a control group.
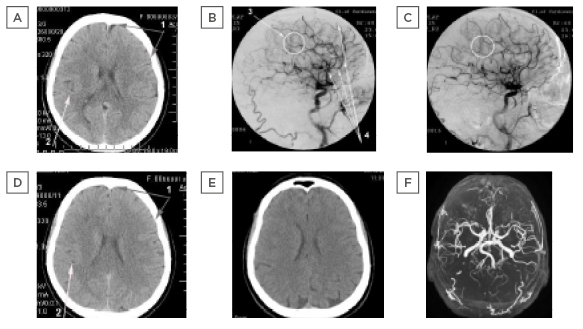
Figure 1: Patient H., 60 years old, female, suffered a small ischaemic stroke in the right hemisphere resulting in partial left-sided hemiparesis.
A) Computed tomography of the brain before intervention: 1) Moderate expansion of the
subarachnoid space; 2) moderate heterogeneous post-ischaemic cyst in the right middle cerebral
artery region.
B) Right-sided carotid multigated acquisition scan before intervention: 3) occlusion of distal branches
of the right middle cerebral artery; 4) multiple stenosis of intra-cranial branches.
C) Right-sided carotid multigated acquisition scan after intervention: Restoration of the lumen and permeability of distal branches of the right middle cerebral artery; improvement of collateral
blood flow.
D) Computed tomography of the brain 12 months after intervention: 1) Subarachnoid space restoration; 2) reduction in the size of the post-ischaemic cyst with signs of cerebral tissue structure recovery.
E) Computed tomography of the brain 6 years after intervention: No signs of residual effects of the
post-ischaemic cyst, the structure of the right hemisphere cerebral tissue is restored.
F) Magnetic resonance angiograph of the brain 6 years after intervention: The permeability and
lumen of the distal branches of the right internal carotid artery are completely preserved, there is
further progression of collateral revascularisation.
Test Group
After the intervention, a good immediate outcome was achieved in 477 (97.95%) test group patients due to the restoration of patency and lumen of the affected vessels, as well as to the collateral circulation revascularisation. Twelve months after the treatment, the results depended on the size of the ischaemic lesion and the timing of the intervention.
- Good clinical outcome (complete recovery of mental and motor functions; BI: 90–100) was obtained in 175 (35.93%) patients
- Satisfactory clinical outcome (incomplete recovery of mental and motor functions; BI: 75–85) was obtained in 228 (46.82%) patients
- Relatively satisfactory clinical outcome (partial restoration of mental and motor functions; BI: 60–70) was obtained in 84 (17.25%) patients
- Relatively positive clinical outcome (absence of negative dynamics with insignificant reduction of mental and motor functions; BI: <60) was not obtained in any case
Control Group
The following results were obtained from the control group:
- good clinical outcome was not obtained in any case
- satisfactory clinical outcome was obtained in 46 (14.79%) patients
- relatively satisfactory clinical outcome was obtained in 96 (30.88%) patients
- relatively positive clinical outcome was obtained in 169 (54.34%) patients
CONCLUSION
Evaluating the data obtained it can be concluded that the method of transluminal laser revascularisation of cerebral blood vessels is effective in treating intracerebral atherosclerotic lesions. Transcatheter laser revascularisation in the treatment of ischaemic stroke with intracerebral atherosclerotic lesions is more effective than therapies. Restoration of intracerebral blood flow can significantly reduce the level of mental, cognitive, and motor disorders and return patients to their active daily life.








