BACKGROUND AND AIMS
There are currently two guideline-recommended diagnostic criteria in use to define a periprocedural myocardial infarction (PPMI) following coronary artery bypass grafting (CABG): the 4th Universal Definition of Myocardial Infarction (UDMI) and the Society of Cardiovascular Angiography and Interventions (SCAI).1,2 Understanding the merits of these definitions has become essential when interpreting the results of trials evaluating the outcomes of CABG. Despite the availability of modern biomarkers, there are as yet no studies comparing the frequency and outcomes of PPMI across these two definitions using high-sensitivity troponin (hs-cTn) assays. These criteria specifically state that a patient must have had CABG in order for a diagnosis of PPMI to be made but this leaves uncertainty as to the diagnosis in patients undergoing non-CABG cardiac surgery. The aim of this study was to describe the frequency, associations, and outcomes of PPMI when applying the SCAI and UDMI definitions using a hs-cTn assay to those patients undergoing CABG and those undergoing other cardiac surgery.
MATERIALS AND METHODS
All patients admitted to cardiothoracic critical care following open cardiac surgery over a 6-month time frame were included, except for those who had a clinically diagnosed Type 1 myocardial infarction. Testing for hs-cTnI was performed on admission and every day for 48 hours, regardless of whether the supervising team felt there was a clinical indication for testing. The results were nested and not revealed to patients or clinicians unless they were requested as part of routine care. After the two PPMI definitions were applied to patients who had undergone CABG, they were also then applied to patients who did not undergo CABG.
RESULTS
The study included 245 patients with at least one CABG, of whom 20.4% met criteria for UDMI PPMI and 87.6% for SCAI PPMI (Figure 1). There was no association between PPMI and length of stay or death in critical care regardless of the definition used. There were 243 patients included who did not have CABG in the study, of whom 11.1% met the criteria for UDMI PPMI and 85.2% for SCAI criteria. Again, there was no association between PPMI (regardless of definition) and length of stay or death in critical care.
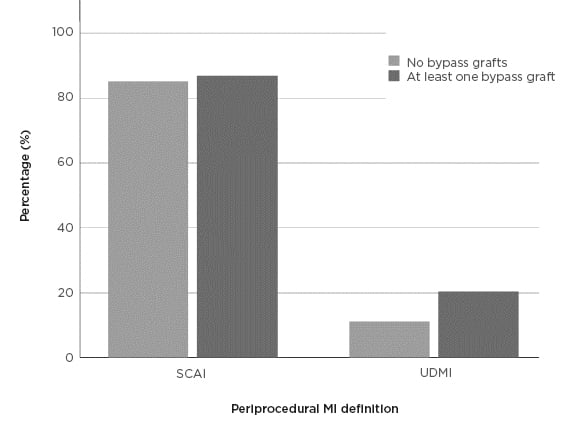
Figure 1: The frequency of periprocedural myocardial infarction depending on the definition used and whether the patient had coronary artery bypass grafts or not.
MI: myocardial infarction; SCAI: Society of Cardiovascular Angiography and Interventions; UDMI: 4th Universal Definition of Myocardial Infarction.
CONCLUSION
The high frequency of PPMI using the SCAI criteria raises concerns about the validity of this definition in the era of hs-cTn assays. Longer term data are required to assess the relevance of a diagnosis of PPMI made using hs-cTn assays. The data suggest that separate PPMI criteria should be considered for patients that do not undergo CABG in future iterations of guidelines.








