BACKGROUND
For more than 20 years, there has been considerable progress in the treatment of coronary bifurcation lesions.1-4 The one-stent technique with proximal optimisation is fundamental in our current philosophy of coronary bifurcation intervention.4 According to the latest European Bifurcation Club (EBC) statements, side branch pre-dilatation (SBPD) is generally not recommended.2-4 SBPD during coronary bifurcation interventions is a technique that is generally not recommended by the latest guidelines and consensus statements. However, the data about the clinical outcomes after SBPD from dedicated studies are surprisingly few. The objective of the current study was to explore the effects of SBPD on all-cause and cardiovascular mortality at long-term follow-up.
METHODS
All patients with coronary bifurcation lesions treated with percutaneous coronary intervention (PCI) between 2012–2022 were included in the prospective registry. Patients were divided into two groups, depending on performance of SBPD: SBPD performed (SBPD[+]) and SBPD not performed (SBPD[-]). For the current analysis, only patients with stable or unstable angina were included, with follow-up of at least 2 years. Patients with ST elevation myocardial infarction and left main stenosis were excluded. Propensity score matching was performed to equalise the effects of the following characteristics: age, sex, diabetes, smoking, hypertension, dyslipidaemia, renal failure, cancer, chronic obstructive pulmonary disease (COPD), atrial fibrillation, left ventricular ejection fraction, and SYNTAX score. A multivariate analysis of all-cause and cardiac mortality was performed, with SBPD as an independent variable.
RESULTS
A total of 832 patients from the registry covered the criteria for the current analysis. After propensity score matching, 324 matched couples remained, and 648 patients were analysed. The demographic characteristics of SBPD(+) and SBPD(-) were well balanced, with no significant differences between groups. Mean age was 68±10 years, 71% were males, 40% were smokers, 47% had diabetes, 26% had a previous myocardial infarction, 53% a previous PCI, 4% coronary artery bypass surgery, 12% peripheral arterial disease, 13% COPD, 32% renal failure, 23% atrial fibrillation, and left ventricle ejection fraction was of 55±10%. Patients with SBPD(+) had more chronic total occlusions (17% versus 9%; p=0.003), longer lesions (42±21 mm versus 36±20 mm; p<0.001), and more severe side branch stenoses (68%±25% versus 41%±31%; p<0.001). Among true bifurcation stenoses (Medina xx1: 63%; 410/648), 88% were predilated. At follow-up to 100 months (median 58 [interquartile range: 37–78]), 205/648 (32%) died. Mortality among the SBPD(+) group was significantly higher (all-cause for SBP[+] versus SBP [-]: 33% [107/324] versus 30.2% [98/324], respectively; p=0.045; cardiac: 25.3% [82/324] versus 21.6% [70/324], respectively; p=0.028) (Figure 1).
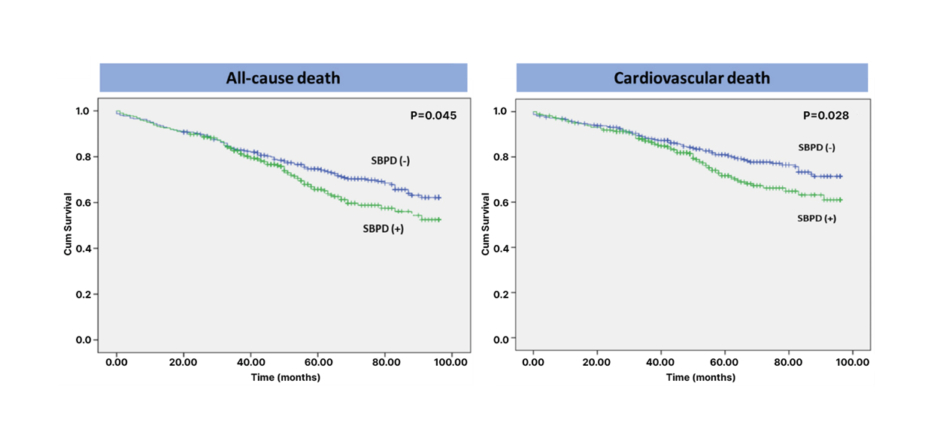
Figure 1: Kaplan–Meier survival curves for all-cause mortality and cardiac mortality in groups with and without side-branch pre-dilatation.
Cum: cumulative; SBPD(-): side-branch pre-dilatation not-performed; SBPD(+): side-branch pre-dilatation performed.
On Cox survival analysis, SBPD(+) was an independent predictor of all-cause mortality (odds ratio: 1.354; confidence interval: 1.003–1.828; p=0.048; with age, mitral regurgitation, left ventricle hypertrophy, pre-PCI troponin, haemoglobin, COPD) and cardiac mortality (odds ratio: 1.512; confidence interval: 1.070–2.136; p=0.019; with age, diabetes, left ventricle hypertrophy, pre-PCI troponin, COPD).
CONCLUSION
SBPD treatment of coronary bifurcation stenoses results in worse patient survival at up to 8 years following the procedure. It gives better angiographic results, but this did not translate into better clinical outcomes.








