BACKGROUND AND AIMS
Infrapopliteal lesions in patients with peripheral artery disease are becoming more common due to the global increase of risk factors such as diabetes, renal, and metabolic disease.1 Angioplasty has recently been shown to be superior to surgery for treating arterial disease below the knee.2 However, these patients commonly present multilevel disease, small calibre, and long lesions with high calcium burden, making endovascular interventions for the infrapopliteal region extremely challenging.1 A wide spectrum of revascularisation strategies and technologies have been developed to address the therapeutic needs in the infrapopliteal space of this region, including support catheters, retrograde access, specialised balloons, and atherectomy for calcified vessels.1, 3-5 The use of stents in this region is currently under investigation. The recent LIFE-BTK study showed better efficacy for adverse limb outcomes with reabsorbable scaffolds placement compared to angioplasty.6 However, the trial included a highly selected population, and the use of stents in infrapopliteal lessions is still uncommon (and not widely available) in world-wide ‘real’ clinical practice.
The aim of this current study is to describe the lesion characteristics, and procedural and technical aspects of infrapopliteal endovascular procedures in Latin America.
MATERIALS AND METHODS
The cohort included patients derived from the Latin American Society of Interventional Cardiology (SOLACI) peripheral registry. SOLACI peripheral is a prospective, multi-centre, observational, and hospital-based registry of patients with lower-limb peripheral arterial disease, who were treated with endovascular interventions across 10 Latin American countries.7 A total of 1,120 procedures were included in the SOLACI peripheral registry between January 2017–May 2023. The current analysis focuses on infrapopliteal interventions, performed as part of a single or multilevel revascularisation strategies (N=554 procedures).
RESULTS
Overall, there was a high prevalence of cardiovascular risk factors and concomitant comorbidities, including hypertension (82.5%), dyslipidaemia (63.4%), diabetes (79.4%), myocardial infarction (15.7%), and stroke (9.0%). Most patients had chronic limb-threatening ischaemia (CLTI; 81.9%), while 17.7% presented with advanced intermittent claudication. From the entire cohort, 27 lesions had a previous endovascular treatment. More than one territory was treated in 250 procedures (45.1%). The target infrapopliteal lesions had a length of 144±88.4 mm and a diameter of 2.82±0.7 mm. Moderate calcification was present in 51.3% and 28.2% presented severe calcification. Atherectomy was used in 1.3%. Stenting was used in 8.5% (47 interventions), of which 22 (3.9%) were performed as rescue stenting or bail-out. Lesions treated with stents were wider (mean diameter 3.20±0.70 mm versus 2.79±0.70 mm) and shorter (mean length 111±101 mm versus 147.0±86.6 mm) compared to lesions treated with balloon angioplasty alone. Most of the procedures using stents required a single device, and only 10 patients required two or more stents. Coronary drug eluting stents were the most commonly used (74.4%). Successful revascularisation was achieved in 533 procedures (96.2%), with 19.1% of the procedures using indirect revascularization. The most frequent intraprocedural complication was thrombosis; 4.3% among patients with stents and 1.8% in patients without stents. Other main complications included embolism (1.3%), and access site haematoma (1.1%). Major adverse events during hospitalisation included death (1.8%), cardiovascular death (0.9%), myocardial infarction (0.5%), and stroke (0.2%).
CONCLUSION
This study illustrates the real-world Latin-American experience, and demonstrates the complexity of infrapopliteal procedures (high-risk factors, comorbidities burden, and complex lesions). Even though some procedures required specialised strategies (e.g., indirect revascularisation, retrograde access), there was a high rate of successful revascularisation with low use of additional dedicated devices such as atherectomy or stents. These strategies can help to reduce costs, amputations, and complications.
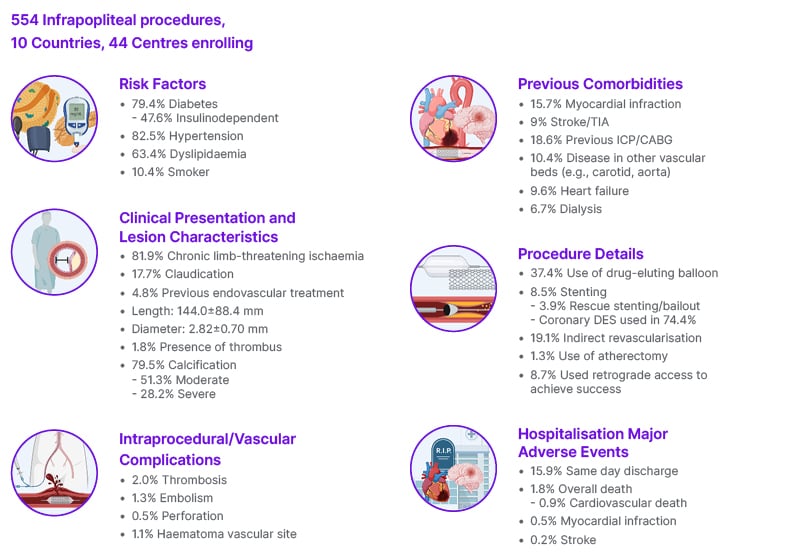
Figure 1: Lesion and Procedural Features of Infrapopliteal Endovascular Procedures from SOLACI Peripheral.
CABG: coronary artery bypass surgery; DES: drug-eluting stents; ICP: intracardiac microaxial pump; SOLACI: Latin American Society of Interventional Cardiology; TIA: transient ischaemic attack.







