BACKGROUND
Percutaneous interventions of bifurcation stenoses represent a technical challenge and pose a high risk of complications.1 Various optimisation techniques such as the proximal optimisation technique (POT) and kissing balloon inflation (KBI) are applied after bifurcation stenting to achieve better post-procedural results.2 However, these methods could still result in incomplete strut apposition to the lateral wall of the side branch (SB).3 The proximal optimisation with KBI technique (POKI) was demonstrated as an alternative to KBI with or without POT, with the potential of shortening the procedure time, and resulting in better final SB ostial stenosis.4 The aim of this analysis is to compare angiographic and clinical outcomes at 12 months between the two groups.
METHODS AND RESULTS
A total of 93 patients with the POKI technique (simultaneous inflation of a balloon in POT fashion with SB balloon) and 295 patients with KBI, with complete 12-month follow-up, were included. Patients with ST-elevation myocardial infarction were excluded. There were no differences in POKI versus KBI groups regarding age (68±9 years versus 66±10 years), sex (67% versus 72% male), hypertension (100% versus 98%), diabetes (38% versus 43%), dyslipidaemia (97% versus 94%), previous myocardial infarction (29% versus 30%), previous percutaneous coronary intervention (48% versus 54%), estimated glomerular filtration rate <60 mL/min/kg (33% versus 31%). Patients in the POKI group had lower left ventricular ejection fraction (50%±7% versus 54%±9%; p=0.030) and higher SYNTAX score (19±7 versus 13±7; p<0.001). The most frequent target vessel in KBI was left anterior descending (66% versus 40% in the POKI group; p=0.027). The procedural time (92±28 min versus 100±38 min; p=0.064), fluoroscopic time (22.8±10.6 min versus 25.8±11.2 min; p=0.083), and total contrast volume (286±85 mL versus 340±121mL; p=0.039) were all lower in POKI versus KBI. The final diameter stenosis in the main branch was not statistically different (15%±8% POKI versus 11%±5% KBI; p=0.067), but significantly lower in the SB (9%±13% POKI versus 13%±23% KBI; p=0.044; Figure 1). The 1-year all-cause mortality was 2.2% for POKI versus 7.8% for KBI (log-rank p=0.089), and cardiovascular mortality was 2.2% for POKI versus 5.7% for KBI (log-rank p=0.221).
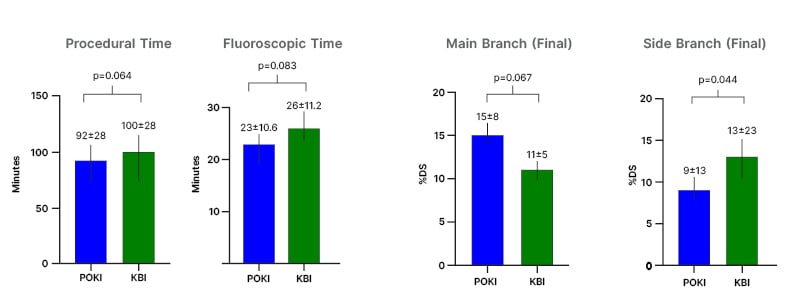
Figure 1: Comparison of angiographic results between patients in the proximal optimisation and kissing inflation technique, and kissing balloon inflation technique groups.
DS: diameter stenosis; KBI: kissing balloon inflation technique; POKI: proximal optimisation and kissing inflation technique.
CONCLUSION
The POKI technique demonstrated similar (even better in the SB) angiographic results in the treatment of coronary bifurcation lesions in comparison with standard KBI, shortening the procedure and fluoroscopic time, and reducing contrast volume. The survival rates at 1 year were numerically lower in POKI patients.







