BACKGROUND
Behind the technical difficulties involved in the percutaneous recanalisation of coronary chronic total occlusions (CTO), a complex scenario of physiopathological mechanisms are responsible for various modifications that affect the vessel. In fact, after successful CTO revascularisation, the segment distal to the CTO undergoes physiological changes, with documented increases in vessel diameters when control angiography is performed at follow-up. The aim of this investigation was to identify the clinical and angiographic predictors of this phenomenon.
METHODS
The PRISON III1 and IV2 trials, which enrolled patients with successfully recanalised CTO treated with drug-eluting stent implantation, were used as the data source for this study. Quantitative coronary analysis (QCA) was performed immediately after the baseline procedure and at 8–9 months follow-up, to specifically address the characteristics of the segment distal to the CTO lesion. Measures included mean lumen diameter (MeanLD), minimal lumen diameter (MLD), reference vessel diameter, and minimal and mean lumen gain (MeanLG). The primary endpoint of this analysis was to identify basal angiographic features and clinical characteristics associated with higher increase in MeanLD and MLD.
RESULTS
A total of 425 patients were suitable for QCA at baseline and follow-up procedures. Mean length of the distal segment analysed was approximately 40 mm. Baseline QCA disclosed a MeanLD of 1.97±0.49 mm and a MLD of 1.33±0.53 mm. Binary stenosis was detected in 167 (39.3%) patients. Follow-up QCA showed an increase in all measures (MeanLG 0.42±0.35 mm and minimal lumen gain of 0.54±0.45 mm). A lumen gain >0.1 mm was observed in 351 (82.6%) patients. Moreover, 151 out of 167 (90.4%) patients with binary stenosis at baseline showed regression of the lesion at follow-up. Association between baseline variables and a significant MeanLG was investigated by means of univariate and multivariate analysis. At univariate analysis, age, smoking, the use of diuretics, the presence of collaterals channels, and basal MLD were predictors of significant MeanLG at angiographic follow-up. Once entered in the multivariate algorithm, however, only the use of diuretics (odds ratio [OR]: 2.62, 95% confidence interval [CI]: 1.12–6.15; p=0.02), baseline MLD (OR: 0.22, 95% CI: 0.12–0.39; p=<0.001), and presence of collaterals and channels (OR: 2.75, 95% CI: 1.35–5.61; p=0.005) were confirmed predictors of significant MeanLG (Figure 1).
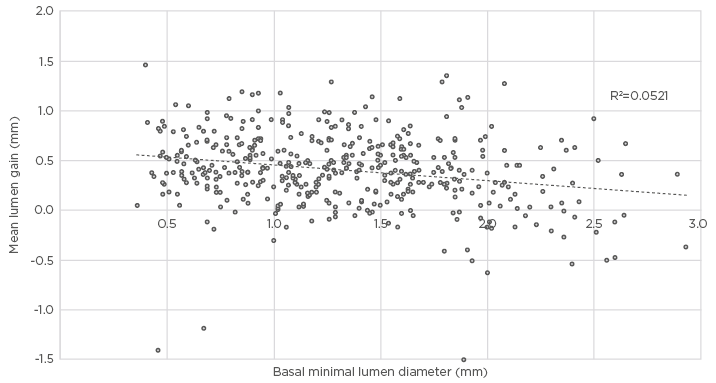
Figure 1: Correlation between basal minimal lumen diameter and mean lumen gain as observed at follow-up procedure.
CONCLUSION
Our results confirm that the segment downstream of the CTO lesions undergoes relevant increases in diameter in most cases if follow-up angiography is performed. Major predictors of late lumen increase are the use of diuretics, the presence of collateral channels, and the basal MLD in the same segment after the baseline procedure.








