Abstract
Self-management programmes for epilepsy have been developed and studied for several decades but have proven difficult to implement and sustain in clinical practice settings. The most advanced work on the concept of self-management has occurred in academic centres with a focus on the theoretical underpinnings of patient and caregiver learning and social support, and the validation of outcome metrics. Although limited by trial design and real-world implementation, many programmes for epilepsy self-management have been successfully demonstrated to provide some benefits. Very few of these programmes however have been successfully sustained and scaled beyond the academic world. Known barriers include logistics and staff resource limitation, patient/caregiver travel, lack of an incentive structure, and limited healthcare promotion. New digital methods of presenting self-management educational content and services may address many of these barriers, even if the experience is less controlled. These online and mobile services permit ‘on-demand’ availability of content that can be tailored to individual needs. However, the epilepsy community must continue to actively promote and sponsor the concept of self-management as a whole.
INTRODUCTION
Epilepsy is a chronic neurological condition defined by a predisposition to recurrent seizures that are not provoked by some environmental or reversible trigger. Approximately 1% of the USA population has been diagnosed with epilepsy and an even greater percentage of the world’s population suffers from seizures.1 Fortunately, many anti-epileptic medications are available and are very effective for the treatment of seizures. In fact, ~65% of patients with a diagnosis of epilepsy can achieve seizure-freedom with singular but daily medication.2 Although the remaining patients often deal with resistant seizures, relief can be provided to many using approaches such as: advanced medication combinations, surgical approaches, and innovative devices.
In addition to standard therapeutic options, patients are also urged to engage in epilepsy self-management. The concept of self-management for epilepsy has existed for decades, supported primarily by a theory of robust patient education for increasing disease knowledge and improving decision-making.3,4 Multiple formal self-management programmes have been developed and academically tested for epilepsy patients, and in its 2012 report, the Institute of Occupational Medicine (IOM) highlights the importance of self-management research on behavioural interventions on health outcomes and quality of life for people with epilepsy. The IOM report also recommends improved and expanded educational opportunities for people with epilepsy.5 Despite this emphasis, self-management programmes have not found traction in clinical use. A recent Cochrane review found it challenging to demonstrate a high volume of evidence supporting self-management strategies;6 it has been challenging for investigators to demonstrate substantive and quantitative outcomes from these programmes in comparison to traditional clinical trials. Additionally, most of these programmes are relatively labour and time-intensive, requiring substantial investment from the clinical centres choosing to support them.
Nonetheless, healthcare providers should become familiar with and consider the potential value of self-management programmes for epilepsy. As the field evolves and more evidence is generated, these approaches will become more readily available and thus, practitioners should be knowledgeable about the concept of disease self-management. This article will provide an overview of traditional and digital self-management interventions, with a focus on the evidence base supporting the use of these programmes, the current barriers preventing adoption, and new digital approaches and solutions that may lower the barriers to implementation.
CONCEPT OF SELF-MANAGEMENT
Health-related self-management is largely rooted in patient education, awareness, and engagement. For epilepsy patients, a lack of patient education about their condition is a widespread problem.7,8 One of the most common reasons for ‘breakthrough’ seizures is simple medication non-adherence.9,10 Unlike some other chronic medical conditions, for which missing several doses of medications may have little or no effect, even a single missed dose for an epilepsy patient can result in a seizure. For well-controlled patients, this event can be a disabling setback. Additionally, a basic understanding of lifestyle decisions, the importance of adequate sleep, and first aid approaches is often lacking in epilepsy patients and their family members, friends, and caregivers. This is partially due to an over-reliance on the ‘pill’ as a prescription and a lack of incentivisation for basic patient education and longitudinal chronic disease support.
The concepts of patient education and self-management have been studied in academic circles for several decades, but have failed to penetrate the routine practice of medical clinics. This may be because patients have not been prioritised as active and engaged participants in their own healthcare. Multiple research streams have now begun to build on the concept of critical social theory, seeking to educate through patient empowerment, often with an emphasis on social connections and learning through context.11 In recent years, there appears to have been a renewed emphasis and attention on the possibilities of patient self-management, with multiple studies12-16 and even a new, validated instrument.17 This trend may be a reflection of a natural increase in patient activation through better information-gathering on the internet and a flourishing of online communities. There may also be recognition of the limitations of traditional treatment algorithms and the opportunity presented by alternative financial models within the USA healthcare system in particular.
Epilepsy self-management is formally defined as: ‘The sum total of steps taken and processes used by a person to control seizures and manage the effects of a seizure disorder’18 and this has been found to be important for the related concept of self-efficacy.19 Self-efficacy has been defined as: ‘The beliefs in one’s capabilities to organise and execute the courses of action required to produce given attainments.’19 Patients who successfully improve their self-efficacy have been demonstrated to successfully complete self-care tasks, such as taking medications and engaging in other healthy behaviours.19 Thus, although related, these two concepts reflect slightly different patient traits that are important for improving health; while self-efficacy represents a patient’s belief or confidence in making favourable health decisions, self-management reflects the actual steps or behaviours that are adopted. Appropriately, standardised and validated metrics for both these concepts exist and have been used in the existing literature on epilepsy management programmes.20
The majority of the historical self-management programmes for epilepsy have focussed on in-person educational sessions and peer support groups (Table 1).12-14,20-22 Most of these programmes focus on specific educational sessions (either in person or digital), but a number of other services exist that may augment the ability of a patient with epilepsy to perform better self-care. These include a growing number of digital and mobile applications for tracking condition-specific data points, such as seizures, side effects, and medication adherence. Streamlining data capture (either through passive techniques or via brief notification requests) and presenting this back to the patient as feedback is increasingly popular. Additionally, the importance of peer support and online communities is well recognised, and these continue to grow. Peer networks are finding their way to mobile platforms, with an increasing amount of ‘matching’ sophistication.
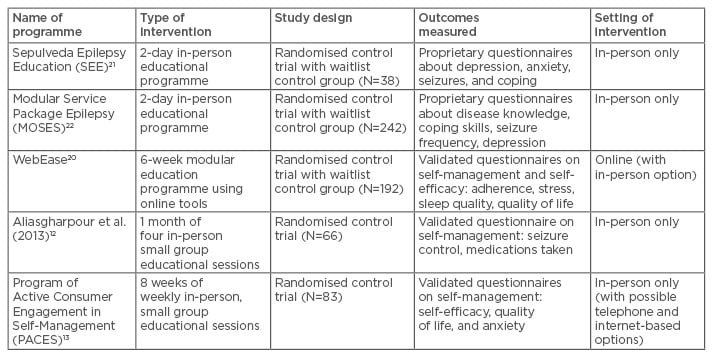
Table 1: Self-management programmes with an educational focus and randomised study design.
EVIDENCE BASE SUPPORTING SELF MANAGEMENT
Many epilepsy self-management programmes have been developed and tested over the past several decades. A recent Cochrane review identified 16 separate interventions focussed on alternative care delivery and self-management strategies for epilepsy patients.6 Of these 16 programmes, the authors determined that four clinical trials were of sufficient quality to be assessed specifically for their focus on self-management (Table 1).12,20-22 Of these, three utilised in-person multi-day educational programming;12,21,22 the work by DiIorio et al.20 utilised the WebEase platform consisting of digital educational modules. The authors of the review concluded that only programmes including a specialised epilepsy nurse and dedicated self-management education showed evidence of benefit. Although the quality of evidence in this area remains quite limited, it is suggested that “…innovative service models could improve identified problems in epilepsy care by improving the knowledge and awareness of epilepsy amongst clinicians and patients…”6 Based on the small numbers of high-quality studies in the review, the Cochrane authors could not “…advocate any single model of service provision.” The review however did provide growing evidence of the importance of dedicated self-management education strategies and highlighted the need for more comprehensive research studies in this area to create a compelling body of supportive evidence.
One of the programmes included in the Cochrane review is the MOSES (Modular Service Package Epilepsy) educational platform, which was tested in a randomised trial in Europe.22 This programme was interactive and tailored, consisting of nine specific modules that highlight different elements of epilepsy care. In the study, the modules were offered as a part of a 2-day course, with 22 epilepsy centres participating in recruitment. The study outcome measures included both epilepsy-specific and generic questionnaires, assessing quality of life, self-esteem, mood, restrictions in daily life, stigma, epilepsy knowledge, and self-reported seizure frequency.22 A total of 242 patients participated in the trial which used a waitlist controlled approach, and questionnaire responses were assessed before the course and after 6 months. The results demonstrated significant improvement in some metrics, such as epilepsy knowledge and coping with epilepsy. Additionally, participants self-reported improved seizure control and more overall satisfaction with their treatment (tolerability). The authors concluded that this study provides clear evidence of a need for improved epilepsy patient education.22
In the 1990s, DiIorio et al.20 developed and validated quantitative questionnaires for assessing both epilepsy self-management and self-efficacy. This created an academic mechanism for demonstrating the value of different programmes focussed on improving self-management. One of the more prominent internet-based self-management programmes is the WebEase effort, developed by DiIorio et al.20 This programme is a primarily internet-based programme, consisting of three learning modules focussing on medication management, emotional stress management, and sleep management. The original programme has its underpinnings in several theoretical learning constructs, including social cognitive theory.11 The WebEase programme is relatively unique in that it is primarily internet-based, and is largely patient-driven. The academic study employed a randomised approach, with half of the study population falling into a waitlist control group for comparative purposes. All participants spent 6 weeks in the trial, spending 2 weeks on each of the three educational modules. Participants were encouraged with email reminders at the beginning and throughout the entirety of the study, and completers were compensated with a gift card. The final study results demonstrated that patients in the treatment group reported higher levels of medication adherence than those in the waitlist control group. Furthermore, patients who completed at least some of the modules achieved higher levels of self-efficacy at the end of the study period.20 Later commentary from the same research group confirmed that social support was a critical component of self-management behaviours in the WebEase study population, although this support was not linked to the online aspect of the programme.23
Since 2007, the WebEase platform and other self-management interventions have been supported in the USA through the Managing Epilepsy Well (MEW) Network which is co-ordinated by the Centers for Disease Control and Prevention (CDC) Epilepsy Program.24 The purpose of this venture is to provide an evidence-based portfolio of digital tools for patients, families, and caregivers to increase awareness and improve self-management opportunities. In a series of formative studies prior to the establishment of the MEW Network, researchers highlighted data suggesting that patient input and needs assessments should be included in any new self-management strategy. Interestingly, although the potential for digital tools was noted, some patients also reported a preference for in-person tools and services. This observation highlights the fact that a variety of interventions will be necessary to adequately target different patient categories. However, in terms of scalability and dissemination, the digital platforms remain highly promising solutions.
Completed after the recent Cochrane review, another self-management programme worth mentioning is the Program of Active Consumer Engagement in Self-Management (PACES) in Epilepsy. This effort builds on prior self-management programmes, which were largely developed by expert opinion, by using patient needs assessments to build the educational content. This platform was studied in an intensive randomised controlled trial, involving weekly in-person meetings over an 8-week period. The study demonstrated robust improvements in validated measures of epilepsy self-management, epilepsy self-efficacy, and quality of life.13 Additionally, the work showed evidence of a durable effect at 6 months for self-management and reported a relatively low rate of attrition in comparison with other intensive educational programmes.
Finally, international medical bodies, including the World Health Organization (WHO) and the IOM, have recently recognised the importance and potential for epilepsy self-management by issuing formal recommendations. In its 2012 report, the IOM prioritised research on behavioural interventions on health outcomes and quality of life for people with epilepsy, and formally recommended improved and expanded educational opportunities for people with epilepsy.5 In 2015, the World Health Assembly (WHA) formally adopted a sweeping international resolution to better address the global impact of epilepsy. One of the formal recommendations included a reference to self-management programmes directly endorsing: “…empowering people with epilepsy and their carers for greater use of specified self and home care programmes…”25
BARRIERS TO IMPLEMENTATION
Despite the wealth of academic evidence supporting epilepsy self-management programmes, these services have unfortunately failed to gain a foothold in most clinical programmes in the USA and worldwide. The projects in active use are either supported through research funding operations or through philanthropic efforts, preventing widespread implementation. Furthermore, the logistical planning, staffing requirements, and patient travel often present a significant barrier for ongoing success.26 In our own anecdotal experiences, in-person support group attendance tends to be highest at the beginning of a programme, then suffers significant attrition with time.
Additionally, the lack of an incentive structure supporting these self-management programmes is another barrier, particularly in the USA. The historical reimbursement system, now perpetuated through systemic inertia, provides few financial drivers to improve epilepsy self-management. Although medication and some procedural interventions should remain the mainstay for active epilepsy treatments, an ideal payment system would support a comprehensive treatment approach, including self-management services. For instance, in conjunction with a new medication prescription, patients should be provided with access to better education and tools for tracking early side effects and improving pill adherence. New alternative payment models are beginning to explore these approaches however widespread implementation remains a challenge.
Under different healthcare models in Europe, more success has been achieved with self-management programmes for other chronic diseases such as diabetes27,28 and asthma.29 Despite facing similar barriers related to resource and logistical support, particularly in some lesser-developed countries, some European nations have initiated and sustained momentum for formal chronic disease self-management programmes. These success stories have largely depended upon official policy statements prioritising patient education services, such as the National Service Framework (NSF) which has been issued in the UK since 2002.27 Consensus-based guidelines are an important first step towards driving research interest towards self-management programmes including outcomes focussed on clinically meaningful metrics and economic impact. From an epilepsy perspective, the WHO and IOM reports are particularly relevant, although these resolutions have only been recently issued.5,25
More specifically, Rogers et al.28 noted that while “European countries are increasingly adopting systems of self-care support for long-term conditions…” there remains significant barriers and disparities due to a variety of country-specific practices. The authors additionally concluded that the “…infrastructure and culture for supporting behavioural change and living well with a long term condition is driven to a significant extent by political decision-makers, the socio-economic and policy [of the] environment and the ethos and delivery of chronic illness management in health care systems.”28 They identified three main areas for targeted outreach: social environmental influences, the reluctance of policy makers to regulate, and a gap in biomedical research focussed on self-management strategies. Focussing on the policy-related barrier, the authors noted that vested interests of other stakeholders within the healthcare ecosystem can impede progress in this arena.28 In Europe, formal guidelines for some chronic diseases, such as diabetes, have succeeded in furthering the pressure to adopt self-management programmes but the inertial force continues to slow the pace of adoption.27,28
In recognition of the need to directly address historical disincentives to implementation, the USA-based Chronic Disease Self-Management Program (CDSMP) has recently been evaluated for its impact on healthcare costs and utilisation.30,31 The CDSMP is a generic self-management education programme utilising a small focus group structure to engage patients and improve their health behaviours. In 2013, a study of the impact of the CDSMP on healthcare savings demonstrated a reduction in both emergency room visits and hospitalisations.30 This was followed in 2015 by the release of a savings ‘estimator tool’ that could be used to determine the overall cost savings that the CDSMP could provide for patients with certain chronic diseases.31 Moving beyond assessments of education and engagement improvements, these types of studies are important to add to the body of evidence justifying an investment in self-management strategies. However, it must be noted that none of these programmes have specifically investigated the impact on epilepsy patients.
Even when the implementation effort is seemingly straightforward, most clinics do not invest heavily in patient education or self-management. This is usually not due to a lack of interest from healthcare providers, many of whom would welcome more resources and time to conduct comprehensive patient and caregiver education. However, even in healthcare systems where economic considerations do not disincentivise these types of programmes, the required intensity of commitment from both the healthcare team and patients often limits long-term participation. However, in a constantly evolving digital age, new approaches to patient education and engagement should be actively sought out and promoted by epilepsy clinics. Methods of simple promotion, such as pamphlets or business cards with website addresses, should be attempted.
NEW DIGITAL APPROACHES TO SELF-MANAGEMENT
The digital and mobile health movement offers an opportunity to dramatically impact the barriers affecting self-management programmes. By offering traditional self-management resources through digital ‘on-demand’ means, the challenges of logistics, travel, and staff resource support are substantially lessened.20 Patients can access resources and engage asynchronously (and anonymously if desired) at their own time and convenience; this offers the promise of expanding access to many patients who previously would have been marginalised. Although some research suggests that patients with epilepsy may use internet-based health tools less than their non-epilepsy counterparts,32,33 the absolute magnitude of usage is still significant (>50%). Furthermore, our own research demonstrates that historically resistant patient populations may be growing more comfortable with technological interventions34 and that real-world online platforms can provide similar self-management benefits to the formal education programmes described earlier.15,35 However, it is important to recognise that online and mobile self-management programmes (particularly those that are patient-driven) are more difficult to study in a controlled trial due to a lack of a consistent setting and a fluid patient experience.
In addition to educational programmes, a medley of mobile diaries and wearable devices are emerging and could eventually further empower patients with data to better manage their epilepsy. Electronic seizure diaries with optimised mobile interfaces are enabling better tracking of seizure details, side effects, and medication adherence.36,37 Furthermore, new wearable technologies can capture a variety of biometric data points that may more accurately quantify seizure burden and severity.38 Although these devices are still investigational, rapid progress is being made and it is likely that some of these approaches will become clinically meaningful in the coming years. More compellingly, these mobile diaries and devices will serve as adjunctive tools for producing meaningful clinical information that may be integrated into the existing online self-management platforms.
CONCLUSIONS
With an ever-increasing amount of evidence supporting the use of self-management programmes for epilepsy, the clinical community should embrace this concept and begin directly addressing the current barriers to implementation. Many academically supported self-management programmes now exist, with various focusses for tailoring to individual patient needs. Although some may critique the magnitude of ‘real-world’ impact of these solutions, many patients are desperately seeking these types of resources and support. Furthermore, the risks associated with these programmes are low, and in the case of self-guided, digital solutions, the logistical support and cost are also low. Thus, with a concerted effort across the clinical epilepsy community, self-management for epilepsy can become a new standard of care for all.








