Abstract
In 2015, the world recorded its highest numbers of international migrants and forced displacement since World War II. With this historic rise in migrants, refugees, and displaced persons around the world, there is a huge risk of chronic illness burden on healthcare systems. Thus, healthcare systems may need to incorporate innovative digital healthcare solutions into their processes and procedures. The purpose of this article is to present the argument that for effective prevention and management of chronic illnesses in ever-increasing migrant societies to be achieved, mobile digital healthcare technologies must be realistically smart and strategically adopted. Beginning with an overview of the current global migration trend, this article considers the implications of this trend for chronic illnesses and the potential for mobile health technologies to support achievement of healthcare outcomes. It highlights three core reasons why digital innovations may be limited as tools for helping to address the global chronic illness challenge and identifies important directions for mobile health technology developers, healthcare professionals, researchers, government and funding agencies, and public health ministries, with a focus on the strategic development and adoption of ‘realistically smart’ phones. The article concludes with recommendations for research and public health education.
INTRODUCTION
All around the world, the high prevalence of chronic illnesses is rapidly shifting the healthcare landscape towards preventive lifestyle behaviours and population health management. Thus, now more than ever, health systems are incorporating into their processes and procedures digital technology healthcare solutions. These are innovative information and computer technologies aimed at achieving one or more health-related goals.1,2 Common among these goals are: improving access to healthcare information, enhancing the patient experience of healthcare services, improving clinical outcomes, promoting health behaviours and population health, reducing inefficiencies while increasing care quality, and reducing the cost of healthcare.3 In line with this broad spectrum of goals, digital health technologies involve a wide range of solutions. These include telehealth and telemedicine, mobile health (mHealth), and health information technologies.3 Some of these solutions (e.g. mobile medical apps) may target specific consumers such as patients and caregivers. Others (e.g. telehealth) may aim at enhancing remote communication, monitoring, and feedback between patients and healthcare professionals (HCPs). Yet still others (e.g. electronic health records) may target information gathering for health administrators, payers, digital health designers, and other stakeholders in the health industry.
Indeed, over the years many healthcare providers and organisations have given increasing consideration to digital healthcare technologies as tools that hold promise for increasing healthcare outcomes while reducing costs.2,4-6 Particularly in the area of chronic illnesses, mobile digital devices and software applications (apps) are being explored as ways of achieving both behavioural and clinical outcomes.7,8 Nonetheless, healthcare systems continue to battle important issues (e.g. inequitable access to healthcare) fundamental to the majority of chronic illnesses that most burden these systems.9 With the current historic rise in migrants, refugees, and displaced persons around the world, there is an even greater risk of chronic illness burden on healthcare systems.9
The purpose of this article is to present an argument to the effect that for effective prevention and management of chronic illnesses in the ever-increasing migrant societies to be achieved, mobile digital healthcare technologies must be realistically smart and strategically adopted. It begins with an overview of the current migration trend around the world. How this trend may contribute to the global burden of chronic non-communicable illnesses, such as diabetes, hypertension, cardiovascular disease, cancers, and mental disorders is then outlined. Evidence of risk factors and prevalence of chronic illnesses in migrants is also highlighted. Next, the paper reviews the role and effectiveness of mHealth technologies in promoting outcomes in chronic illness. This is followed by an outline of three core reasons for which existing mHealth technologies may be limited in effectively tackling any probable chronic illness epidemic9 as a result of the increasing migration. Finally, important directions for mHealth technology developers, HCPs, researchers, government and funding agencies, and public health organisations are identified, with a focus on the strategic development and adoption of ‘realistically smart’ phones (RSPs). The paper ends with recommendations for research and public health education efforts.
GLOBAL MIGRATION TRENDS
In 2015, the world recorded its highest ever number of international migrants; 244 million people worldwide moved from their countries of origin to other countries.10,11 Compared with the 232 million migrants in 2013, 12 million more people migrated in 2015.10 By the end of the same year, >1.2 million people, largely from Syria, Afghanistan, and Iraq, had sought asylum within the European Union (EU), reflecting >50% the number recorded in 2014 (563,000). Indeed, this is the highest level of forced displacement recorded worldwide since World War II.10 Unfortunately, while these figures are appalling, they are predicted to further rise in the coming years, as the United Nations (UN) and other world organisations struggle to achieve lasting solutions to the conflicts and persecutions in the Middle East, South Asia, and also parts of Africa such as Nigeria.12 Within countries, internal migration is also reported to be on the rise.10 This historic migration trend suggests that many societies are getting increasingly pluralistic and complex. First, there is the presence of various ethnocultural groups in receiving countries and internal regions. Secondly, there is increasing diversity in language, health, educational, religious, and socioeconomic needs of the various ethnocultural groups. Thirdly, and as a matter of urgency, host countries may need to develop and/or amend policies to cater for the health and socioeconomic needs of migrants and for the diversity in needs.
MIGRATION AND CHRONIC ILLNESSES
Whether internal or external, migration generally brings with it an increased potential for infectious disease spread.9 Yet, with the massive influx of migrants in developed and developing countries, healthcare systems may record higher incidence and prevalence of long-term non-communicable illnesses.13 Firstly, the steep rise in populations may greatly reduce the capacity of available healthcare resources and services9 to identify at risk persons, provide timely preventive interventions, and efficiently manage known chronic illness cases for both migrants and residents. Secondly, the surge in language barriers may limit access to healthcare and health-related socioeconomic resources (e.g. housing, employment, and education), particularly for migrants.14-18 These two fundamental issues facing contemporary healthcare systems may lead to the onset and progression of chronic illnesses in diverse ways. These include increasing waiting times for accessing health screening services, increasing stress from limited access to pertinent socioeconomic resources, and promoting health risk behaviours including smoking, unhealthy eating habits, sedentary behaviours, and alcohol and substance abuse. In addition, they may lead to suboptimum adherence through poor patient–HCP communication and poor understanding of treatment prescriptions. In chronic illnesses, non-adherence to medications and lifestyle recommendations is a major determinant of illness progression.19,20 Furthermore, language barriers may reduce access to food labels, which are important for making informed decisions about foods. Inability to do so could have a negative impact on diet quality and hence health. Figure 1 illustrates a theorised model of the relationships between the influx of migrants and prevalence of chronic illnesses.
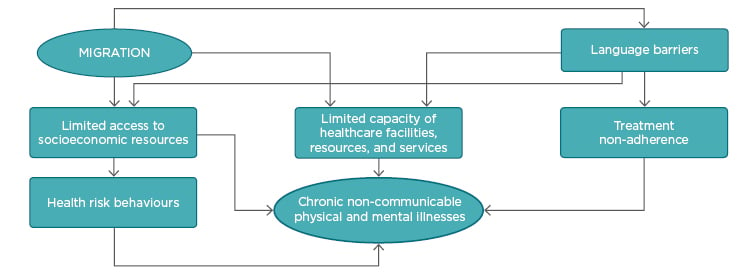
Figure 1: Hypothesised relationships between migration influx and chronic illnesses.
RISK FACTORS AND PREVALENCE OF CHRONIC ILLNESSES AMONG MIGRANTS
Compared with non-migrants, a number of studies have found a high prevalence of chronic non-communicable illnesses and related risk factors among migrants.13 These factors include communication difficulties (due to language differences), poor employment, and poor social status.21-23 Post-migration stress has also been identified as one of the most consistent factors associated with depression, post-traumatic stress disorder, and generalised anxiety disorder.22 Among resettling migrant women, studies suggest an increased risk of experiencing somatisation and low birth-weight infants.24 Immigrant women have also been found to be at increased risk of social vulnerability15 and at more than twice the risk of Canadian-born women for postpartum depression.21 Often, women migrate during their childbearing years and may lack knowledge about the rights and services available to them.15,21,25 Among migrant men, a study of Gulf migrants (including emigrants from Kerala, India, to the Gulf countries) and non-migrants in India found that a majority of health risk factors for non-communicable illnesses were significantly higher in migrants.26,27 With the exception of alcohol use, the prevalence of tobacco use, physical inactivity, poor diet habits, chronic illness history, less sleep, and longer work hours were significantly higher in migrants than non-migrants.26 Accordingly, hypertension and abdominal obesity were significantly more prevalent among migrants than non-migrants.26,27 A similar study found that participants with a history of migration (largely from Kerala to the Gulf countries) had a higher prevalence of diabetes, hypertension, and cardiac problems.28
Chronic illnesses currently constitute the most prevalent and costly of all health problems in both developed and developing countries,4,13,29 with morbidity and mortality from chronic illnesses exceeding that from infectious diseases.29 Coupled with the generally strained healthcare facilities and resources worldwide, it is of utmost importance that smart yet realistic mHealth innovations are adopted to help address the core health needs of contemporary pluralistic societies. Specifically, the need for: i) innovative language-bridging solutions; ii) increased access to preventive healthcare information and services irrespective of socioeconomic status; iii) wider promotion of healthy lifestyles and behaviour change techniques; iv) enhanced self-monitoring and self-management behaviours; and v) increased access to essential health-related socioeconomic resources (housing, education, employment, support networks). This task may seem enormous and costly, yet countries that have embraced pluralism and fostered integration of migrants via effective policies and programmes, referred to as multicultural countries, tend to report higher health as well as economic status.30
THE ROLE AND SUCCESS OF MOBILE DIGITAL INTERVENTIONS IN HEALTHCARE
Over the last two decades, well over 100,000 health and medical apps have been designed for use on mobile smartphones, tablet computers, laptops, and wearable devices.31 Presently, consumers can use mHealth technologies to access a wide range of clinical and public health services.32 For instance, smartphones together with wearable wireless sensors can be used to measure, monitor, and manage vital body signs (e.g. blood glucose levels), which are critical in chronic illness management.8,32-34 With the increasing movement of populations to developed and developing countries, where resources are typically fewer and concentrated in urban areas, mHealth devices and apps may offer opportune avenues for meeting the critical health needs of modern societies.7,34,35 Their capacity for continuous interactive wireless communication means that health interventions can be accessed independent of geographic location.34,35 Intervention content can also be delivered and updated consistently across users.35 These devices allow users to privately and anonymously access personalised interventions at their own convenience and pace.34,35 As interventions are accessed independent of expensive therapy consultations, mHealth innovations are potentially cost effective.34 Furthermore, they have the potential to revolutionise healthcare research, data analysis, and service delivery via real-time data collection.35
Empirically, a recent systematic review of 30 randomised controlled trials (RCTs) found that telemonitoring interventions significantly reduced the odds of mortality and hospitalisation among people with heart failure, compared to standard post-discharge care.36 Telemonitoring interventions may include HCPs monitoring symptoms through live telephone calls with patients. Patients may also enter data on signs and symptoms into an electronic communication device (e.g. smartphone) to be downloaded and viewed later by HCPs.37 Among a cohort of 17,025 veteran patients, a home telehealth programme was found to reduce the number of bed days of care by 25% and the number of hospital days by 19%. The average cost per patient ($1,600.00 per annum) was reported to be substantially lower than nursing home care.38 A recent comparison of patients on the programme to a matched control group indicated further reductions in hospitalisations, healthcare costs, and mortality rates for programme participants.39 In men who have sex with men, a tailored and interactive text-messaging intervention (a set of messages addressing nine topic areas) significantly improved medication adherence, human immunodeficiency virus (HIV) knowledge, and social support post-intervention, whereas there were significant reductions in viral load and the number of sex partners.40 Findings of a systematic review of the effectiveness of communication technologies among adolescents with diabetes showed that 10 of 18 studies found positive improvements in blood glucose levels, although four studies reported detrimental increases in blood glucose levels.41 Increased frequency of patient–HCP contact was found in 15 studies.41 In a recent systematic review of 42 controlled trials of mobile technology-based health interventions, modest benefits were found for SMS reminders on appointment attendance.1 In developing countries, a review of mHealth intervention studies (largely SMS messages) reported enhanced mass delivery of health information, remote patient monitoring, self- management, and data monitoring systems for diagnosis and treatment.42 A similar review including nine RCTs found that mHealth interventions (e.g. mobile phone-based interactive software plus management feedback) positively improved chronic illness outcomes. These included clinic attendance, medication adherence, pulmonary function (in asthma patients), emergency visits, hospitalisations, and cost-effectiveness.43
Many of these reviews indicate high heterogeneity in study design (e.g. from RCTs to pilot studies42) and quality. Yet, generally, the extant literature over the years seems to assert that mHealth innovations are potentially effective strategies for promoting healthcare.1,7,32-43 In certain countries, some mHealth technologies have received approval from government agencies such as the US Food and Drug Administration (FDA).32
MOBILE DIGITAL TECHNOLOGIES AND CONTEMPORARY HEALTH NEEDS OF PLURALISTIC SOCIETIES
Despite their potential healthcare and public health benefits, the question remains of whether innovations are being realistically leveraged to the probable epidemic of chronic illnesses9,13 facing contemporary societies. It is argued that unless mHealth is fully accessible to migrants, as well as average residents, ethnocultural minorities, and the most vulnerable across societies, this could breed a digital divide that may severely intensify the global health challenge of socioeconomic inequalities.35,44 As it stands, it is worth asking how many of the world’s population can afford a smartphone. On one hand, most smartphones are overly sophisticated, replete with superfluous apps, many of which consumers may hardly make use of, and are unreasonably expensive. On the other hand, low-end mobile phones tend to lack the basic features and capacity for internet-based healthcare interventions. There is also the question of what percentage of the world’s population has access to a wireless internet connection? Even in the UK, reports indicate that about a fifth of the adult population has absolutely no home internet access.35 This suggests that in low-income countries, more people may have no access to internet-based health interventions. Furthermore, although mHealth innovations are penetrating most modern societies, few public health education efforts are aimed at supporting consumers to effectively use these technologies. Among socioeconomically disadvantaged groups, who generally record lower educational levels, this may also contribute to a digital divide and wider gaps in health inequalities.35,44 Lack of mHealth education may further heighten migrants’ fears that data could lead to deportation, xenophobic, or discriminatory attitudes.45,46 So what is the way forward in effectively harnessing mHealth technologies? Rather than simply increasing access, a strategic and multidisciplinary effort is required.
DIRECTIONS FOR DEVELOPMENT AND ADOPTION OF ‘REALISTICALLY SMART’ MOBILE PHONES
To equitably promote clinical outcomes and public health across the globe via digital health, three things need to be critically considered. First, mobile phones, the most widely available technology, should be designed to realistically address the critical health needs of contemporary pluralistic societies. More practically, RSPs, in addition to the basic features of a mobile phone should have: i) capacity for wireless internet connection; ii) a built-in/affixed sensor for measuring multiple vital health information (e.g. temperature, blood pressure, blood oxygen, glucose levels, and heart rhythm); and iii) a core set of medical and health apps preinstalled. The core set of apps must be approved by appropriate institutions (e.g. food and drug agencies) and help to bridge language barriers, provide clinical diagnosis and treatment support for common health problems, encourage healthy lifestyles and provide evidence-based techniques for risk behaviour change, support self-monitoring and self-management behaviours, and alert users of vital health-related opportunities for socioeconomic resources. For example, RSPs could include an app that easily translates words, sentences, and inscriptions on snapped images from dominant languages into numerous local dialects and vice-versa. This could particularly support migrants and linguistic minority groups to better engage with health information and communicate with HCPs. The RSP could also include an app that picks up all job openings and socioeconomic opportunities within the residing country of the user daily, and display this information in a selected language option.
Secondly, just as going to school is a human right and as such governments strive to bring education to all, so is access to health a human right. Therefore, in this era of digitisation, governments must equally strive to partner with phone developers, app designers, HCPs, and healthcare researchers with a goal to invest in affordable RSPs and gather evidence of their influence on clinical outcomes and public health. Furthermore, the onus lies on governments to make wireless internet widely and freely accessible so that all persons, irrespective of socioeconomic status or geographic location, can access essential internet-based health interventions.
Finally, to prevent creating a new cause of health inequalities and rather promote digital health for all persons, there must be a revolution in public health education efforts across the globe. Public health ministries need to focus on actively training the public to use information and communication technologies. Such education efforts should be drastic enough to ensure that all persons, irrespective of adult age or socioeconomic background, have the knowledge and skills required to connect to the internet, access digital health interventions, take the necessary health actions at any stage of the care continuum, and seek support with security and privacy concerns. It is only when this revolution in public health education efforts parallels the revolution in digital technology healthcare solutions can maximum uptake of these innovations be realised.
LIMITATIONS
Few studies have considered the prevalence of chronic physical illnesses compared with mental illnesses in migrant populations and subpopulations (e.g. reproductive health problems in women migrants). Despite the numerous evaluation studies in mHealth, evidence of long-term, large-scale effectiveness and cost-effectiveness, as well as continued engagement with mHealth programmes, is still not uniformly conclusive across disease areas, innovation types, subpopulations, and countries. While it is largely asserted that developing countries may benefit greatly from mHealth, efficacy, cost-efficacy, and practicality (e.g. concerns about data security) are extremely lacking in these regions.
CONCLUSION
As the world grows progressively diverse due to the continuous rise in migration, there is an increased potential for development of chronic illnesses through reduced access to healthcare information and services and socioeconomic resources. Mobile digital healthcare technologies, owing to their availability and functionality, have the capacity to support achievement of clinical and public health outcomes. Nonetheless, it is important that they are realistically designed and strategically adopted to avoid a digital divide, whereby those most in need of healthcare education and services are the least likely to access digital health interventions. It is recommended that government agencies support intercultural research that provides rigorous evidence for mHealth innovations across regions and sub-regions. Community platforms for updating especially low socioeconomic-status groups on mHealth research (including phenomenological reports from mHealth users) and for soliciting input for further research may help alleviate security concerns and boost adoption of these potentially beneficial technologies.








