Abstract
Medical education is lagging behind advances in planetary health knowledge due to the considerable barriers to introducing new topics into medical curricula. This potentially leaves doctors of the future ill-equipped to deal with the health challenges associated with environmental degradation. The recently conceived ‘infusion’ approach by the Icahn School of Medicine at Mount Sinai, New York, USA, represents a promising method for integrating planetary health topics into medical education. Adopting this approach, the International Medical Education Collaboration on Climate and Sustainability (IMECCS) was founded, with the goal of empowering healthcare students and faculty members worldwide to integrate planetary health education into their curricula.
IMECCS consists of medical students and faculty members at universities in the USA, UK, and Honduras with experience in introducing planetary health topics into medical curricula. Based on discussions of challenges and successes, the group created an online open-access resource bank designed to enable a medical student or faculty member, without prior experience, to implement a planetary health curriculum and infuse these topics into existing teaching sessions at their institution.
Key Points
1. Planetary health is underemphasised in medical school curricula. There are numerous barriers to implementing changes to existing curricula. This article was written by an international group of authors who collaborated to identify and tackle those barriers.
2. This article describes a streamlined approach and framework that medical schools across the globe can adopt to start narrowing this gap, and prioritising future physician education on these important topics.
3. The authors’ generalisable platform is aimed at empowering healthcare students and faculty members worldwide to implement changes to their medical school curricula, with a resource bank of educational content and guides. This content is designed to be easily ‘infused’ into already existing teaching sessions, allowing educators to teach planetary health topics without prior knowledge.
INTRODUCTION
The climate crisis is a health crisis that has the potential to cause significant morbidity and mortality to human populations, and to worsen health inequities across the globe.1,2 The healthcare sector itself is a major contributor to this crisis.3 To combat the present and forecasted threats of global environmental change on human health, it is important that we, as a global society, prepare doctors for a future with an unstable climate, equip them to serve patients given this changing landscape, and empower them to practice sustainably. The reality of this looming health disaster has only recently become widely appreciated within the medical community, and planetary health (PH) has only truly been conceived as a science and concept in the last decade.4,5
It is well recognised that medical curricula and practice tend to lag behind advances in scientific research.6 This, in part, has led to a paucity of teaching on PH topics at medical schools globally.7 Given the role that doctors will have in mitigating the worst of the health consequences of the approaching environmental crises, there is a certain urgency to educate students on PH topics, and we cannot afford the typical lag from research to curriculum. The slow dissemination of PH research into the classroom and clinical spaces has meant that educating current and future doctors on PH topics is a major challenge, which now requires innovative solutions.
At the medical school level, solutions to this challenge must address fundamental barriers to change and implementation, which are common, to varying degrees, across all medical schools. Various methods and frameworks to overcome these barriers, and to integrate PH topics into the curricula, have been suggested in the literature, but uptake still appears slow from medical schools globally.8-11
The authors founded the International Medical Education Collaboration on Climate and Sustainability (IMECCS) in 2020, in response to discussions on the barriers to introducing comprehensive PH education to medical school curricula. The authors quickly began to identify common themes in their struggles. Now, with faculty and medical student representatives in eight medical institutions and across three continents, the authors have worked to develop a generalisable platform that supports others to successfully overcome these barriers. IMECCS’ resources include a framework for the successful integration of relevant and critical PH material into the already existing medical curriculum, as well as a publicly available database of ready-to-use, well-cited slides covering an array of PH topics and content.
BARRIERS TO IMPLEMENTING PLANETARY HEALTH TOPICS INTO THE MEDICAL CURRICULUM
Through the authors’ work, the following common barriers to implementing a PH curriculum were identified.
Limited Time Within a Dense Medical Curriculum
As with introducing any new topics into the undergraduate medical curriculum, there is little room for additional content without removing existing teaching sessions, or risking overwhelming students who are already under considerable pressure. Understandably, these factors can lead to pushback from faculty and students when attempting to add new content to the curriculum.12
Variable Educator Awareness and Subject Knowledge About Planetary Health
Due to the longstanding dearth of education on PH topics, many educators lack the confidence or base knowledge to teach on these topics, even if relevant to their specialty.11,13,14 For example, respiratory physicians may have never been equipped with the knowledge that different inhalers have considerably different emissions profiles, or stroke physicians may not know that pollution has strong links to cerebrovascular disease.15,16 Therefore, these important topics are not covered in their teaching sessions.
Lack of Bandwidth Among Medical Faculty for Curriculum Change
Even with knowledgeable and eager faculty, finding adequate staff with capacity to change medical curricula can be challenging without additional specific PH education funding, mandates, or staff resources. Effectively creating a PH curriculum requires a significant amount of time in researching and generating materials, communicating with educators, delivering teaching sessions, and developing assessment tools.
Perceived Lack of Interest in Planetary Health Topics?
Another barrier the authors had anticipated was student and faculty appetite for the introduction of PH topics. However, in their experience, engagement in PH topics was high amongst both educators and students, and met mostly with great enthusiasm. This experience is supported by the literature exploring attitudes towards the climate crisis among medical professionals.8,17-20 It has been well documented that there is global demand for medical teaching on PH topics, which is unmatched in supply from medical curricula.
Strategies to Implement Planetary Health Education
Given the heterogeneity of institutional structures and cultural norms, it is difficult to overcome all barriers for all organisations without local expertise and institutional support. To make their approach as generalisable as possible, the authors sought input from medical students, and junior and senior faculty members from multiple institutions across the UK, the USA, and Honduras. This group, IMECCS, has the express goal of empowering healthcare students and faculty members worldwide to integrate climate and sustainability education into their curricula, by creating open source educational content and guides for implementation.21
A consensus was reached to develop a resource bank of materials that would enable relatively easy implementation of a PH curriculum in any undergraduate or graduate medical course. This bank would provide a roadmap from inception to full integration of a PH curriculum, so that any engaged individual, student, or faculty member could approach their organisation with a proposal to introduce PH into the curriculum.
In addition to referencing excellent pre-existing educational resources, including the Planetary Health Report Card (PHRC), Medical Students for a Sustainable Future (MS4SF), and the Global Consortium on Climate and Health Education (GCCHE), the authors focused on leveraging the experiences of their multi-institutional working group, to identify specific topic areas within the existing medical curricula where collaborators had experienced success in introducing PH.11,22-24 These topic areas were separated into categories that would reflect teaching sessions common across all medical schools.
Curriculum Infusion
To provide a reliable framework for implementation, a robust overarching approach was required. The recently conceived ‘infusion’ approach to integrating PH topics represents a promising solution to introducing PH into the medical curriculum. The approach was developed by staff and students at the Icahn School of Medicine at Mount Sinai, New York, USA, who implemented a ‘Climate Change Curriculum Infusion Project’.8 This strategy was subsequently adopted by Southampton Medical School, UK, which in 2023 was one of only four universities globally to achieve an ‘A grade’ for curriculum in the PHRC.23,25
The approach attempts to overcome the aforementioned barriers by inserting PH topics into already existing lecture content, sparing the need to add separate lectures on climate topics, or for educators to spend additional time and energy researching the PH implications of their lecture topics. After an assessment of the medical curriculum, specific teaching sessions are identified, in which PH material could be organically inserted to maintain relevance to clinical topics. Medical educators are approached with ready-made material to ‘infuse’ into their teaching sessions (Figure 1). This approach is beneficial, as it allows for a relatively easy introduction of PH teaching across the medical curriculum, to which it is almost ubiquitously relevant.
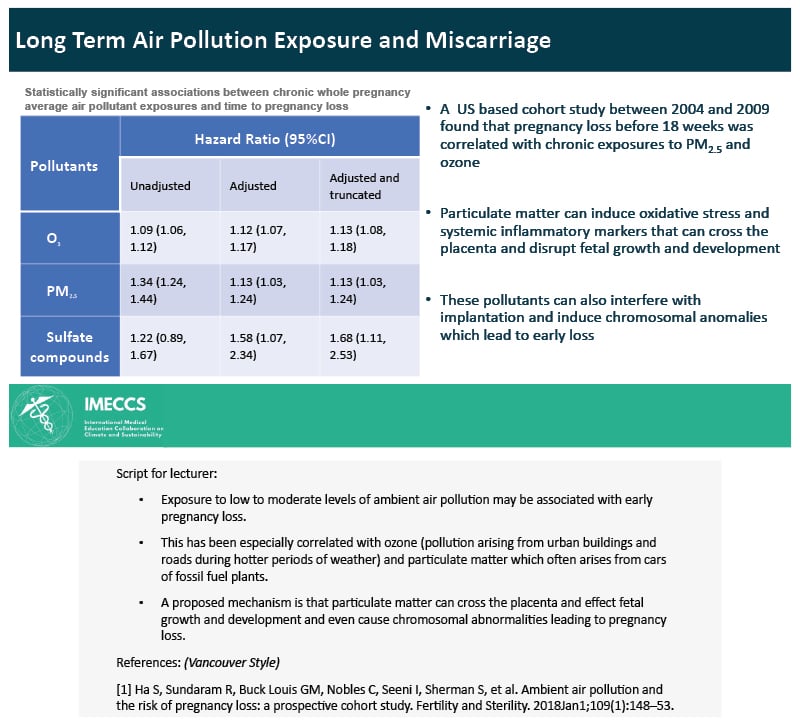
Figure 1: Example of International Medical Education Collaboration on Climate and Sustainability
(IMECCS) slide with script and reference.26
IMECCS: International Medical Education Collaboration on Climate and Sustainability.
Other ways of integrating environmental health topics include problem-based learning approaches and standalone distinct modules.22 Medical schools that appear to be leading the way in implementing PH curriculum, such as Keele University, UK, which was one of the top-ranking medical schools in the PHRC, tend to have multifaceted approaches, both infusing content but also delivering standalone teaching sessions and workshops.22 However, following collaborator discussions, the authors decided that the infusion approach offered the greatest generalisability as a starting point for curriculum development, and as such, was used as a basis upon which the resources were created.
CREATING AN OPEN-ACCESS RESOURCE BANK
How-To Guide and Model of Implementation
Based on the authors’ collective experiences in implementing PH content at their respective medical institutions, they distilled common steps for PH infusion. These steps were amalgamated to create the circular six step ‘IMECCS Model of Climate and Sustainability Implementation’ (Figure 2), and an associated how-to guide that it is anticipated individuals can utilise in their PH infusion process.
The six steps of this implementation model map out the process by which an individual can implement a PH curriculum at their medical school. The six steps are detailed in Figure 2, and are accompanied by an illustration of how these steps were carried out in practice at Southampton Medical School, where this model was implemented.
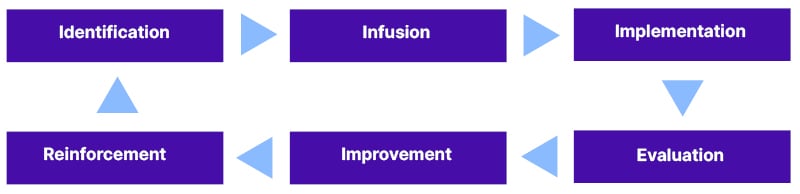
Figure 2: International Medical Education Collaboration on Climate and Sustainability (IMECCS) Model of Climate and Sustainability Implementation.
Identification
Identification refers to an initial assessment or audit of the undergraduate medical curriculum, to identify where there are potential opportunities to incorporate PH topics. An audit would involve identifying a relevant set of PH learning outcomes, as adopted by the institutions’ governing body, and assessing which learning outcomes are covered by the current curriculum. A recent study detailed a methodology whereby UK medical schools’ curricula were audited against learning outcomes referenced by the General Medical Council (GMC).27-29 A similar approach can be taken on an individual institution level. Additionally, the PHRC provides an excellent assessment of curricula. Following this assessment, individual teaching sessions or modules should be identified where there may be an opportunity for the introduction of PH topics.
This step also includes the process of identifying influential members of faculty who might be amenable to helping support the transformation of curricula. These faculty members can help advocate for change.
Worked example at the University of Southampton
A junior doctor initially approached a Professor of Public Health regarding the implementation of a PH curriculum. The professor was very enthusiastic, and supported an audit of the curriculum against an agreed set of learning outcomes. Specific teaching sessions were identified and targeted for infusion of PH topics.
Infusion
Once specific teaching sessions or modules have been identified, the corresponding educators should be contacted to gauge their interest in including PH content in their teaching sessions. If they are amenable, they can then be provided with ready-made materials, as provided by IMECSS. For example, a lecture discussing miscarriage could include IMECCS’ ‘Miscarriage and Pollution’ slides; an example is shown in Figure 1.
Worked example at the University of Southampton
Following the audit, the team emailed educators who were teaching targeted sessions. Educators who showed an interest in including PH content were provided with slides appropriate for their specific teaching session(s). For example, slides regarding the environmental and health co-benefits of a plant-based diet were provided for a nutrition lecture.
Implementation
Prior to the teaching of these topics, educators may need to be provided with some support, for example, bulleted talking points, to increase their comfort in teaching the topic. All IMECCS slides are provided with extensive notes for the educator, to support them in delivering the new content.
Worked example at the University of Southampton
In some cases, the team arranged meetings with individual educators to discuss and agree on the topics for infusion, and where they might fit best in their teaching sessions.
Evaluation
The assessment of the current progress of implementation across the curriculum step can include formal student assessment, in the form of essays or exam questions; student and staff surveys; and qualitative feedback from educators.30 Similarly to the identification step, internal audits, or the PHRC can provide an evaluation of progress towards implementing a comprehensive PH curriculum.
Worked example at the University of Southampton
Some formal assessment questions were written and added to the end-of-year exams for pre-clinical students. In addition, the undergraduate curriculum went through a second audit phase to identify where there was inadequate coverage of the PH learning outcomes.
Improvement
The refining of current resources is based on the evaluation step, as is tailoring them to educator and student feedback. If gaps in the PH curriculum persist, further infusion and implementation may be required in additional teaching sessions across the curriculum.
Worked example at the University of Southampton
After the second audit, new material was added to existing infusion materials, and further educators were engaged from a wide variety of subject areas. This second round led to further coverage of learning outcomes.
Reinforcement
To ensure the sustained teaching of PH topics, it is important to regularly reinforce the importance with educators. As such, the authors recommend that after each academic year, educators are re-engaged and, if necessary, provided with up-to-date materials.
Worked example at the University of Southampton
The team compiled a list of educators who have been engaged previously. These educators are emailed on a yearly basis to ask if any further support is required, and if the content was used in their teaching sessions.
Creating Teaching Materials
The infusion approach can be utilised in curricula with both case-based and didactic teaching methods. While case-based teaching has become increasingly popular, lecture-based teaching remains one of the most common methods of educating medical students. As such, the authors chose to create teaching materials in the form of lecture slides, with the intention that this medium would be the most utilisable globally for infusion into medical curricula.
For effective and successful infusion, it was essential that the slides be relevant, concise, well-referenced and, most importantly, include a script for the educators. The slides were designed to be used by educators with no necessary prior experience in teaching PH topics, so a detailed script is essential to all materials.
The creation of the slides was divided amongst collaborators, with an independent reviewer for each topic nominated to ensure the quality of the slides and scripts, correct formatting, and adequate referencing.
Three categories of teaching materials were identified for the open access platform: ‘Climate and Health’, ‘Clinical Skills’, and ‘Sustainability in Practice’. Within these categories, further subcategorisation was made to reflect common education themes or topics in medical education, and so that materials could be easily navigated by the user.
Sharing Resources
A simple website was designed, so that any user could easily access materials. In April 2021, IMECCS.org21 was launched online, with open access to all materials. Users are required to complete a short survey to gain access.
Overcoming Barriers to Implementation
This project was born out of a need for free, easy access educational materials to improve coverage of PH topics in medical curricula worldwide. The aim was to create a ‘one-stop shop’, complete with an implementation framework, and well-cited, ready-to-use lecture slides that a student or faculty member could use to introduce these topics into their medical school’s curriculum, with or without dedicated institutional support and resources. This strategy addresses the barriers to implementing PH education for medical students.
The infusion approach was used as a basis for IMECCS resources, as it offers the possibility of overcoming two major barriers to implementation: limited time within a dense medical curriculum, and variable educator awareness and subject knowledge about planetary health. The approach does not overly burden the already densely-packed medical curriculum. Inserting PH content strategically across the course means that no additional lectures are required. Integrating the topics within existing teaching sessions also keeps the content relevant to medical students, who may not have otherwise engaged in elective or non-core PH modules, and is less likely to overwhelm them than adding standalone mandatory lectures.
The infusion approach does not require advanced educator knowledge. With this method, premade, well-cited content is provided to the educator, empowering them to teach the topic with minimal additional cognitive load, or time spent researching. This approach helps to reduce the burden on the educator to create novel material, and reduces anxiety about teaching outside of their core expertise.
The success of the initial curriculum infusion projects at the Icahn School of Medicine at Mount Sinai, and the University of Southampton, benefitted greatly from strong support from motivated faculty. The authors recognise that without such support from individuals in positions of power, creating resources and gaining educator buy-in can be significantly more challenging. Students and educators alike may lack the confidence and capacity to create quality material, and to integrate PH topics effectively into the curriculum. Though top-down support is ideal, the authors hope that their implementation framework and database of lecture slides will minimise effort, and facilitate bottom-up infusion of climate change topics by motivated students and faculty, even in the absence of institutional support, thereby addressing the third barrier: lack of bandwidth among medical faculty for curriculum change.
So far, the resource has been used globally, and has received anecdotal positive feedback. A limitation of the authors’ work was that they did not robustly collect this feedback from users. Although they initially collected data as to individuals’ motivations for accessing the platform, this was for quality improvement purposes, and, as such, relevant ethics were not obtained at the time, so this data cannot be published. It is important that this data is collected and published in the future, to understand the utility of open access resources.
There is still much room for growth and development in this space. Specifically, there is a need for assessment materials for educators, in the form of essays, and short answer and multiple-choice questions.31 In addition, the provision of other forms of educational material may be beneficial for both educators and students, such as problem-based learning cases.32 The GCCHE, in collaboration with Brigham and Women’s Hospital, Boston, Massachusetts, USA; Massachusetts General Hospital, Boston, USA; University of California San Francisco, USA; and Emory University School of Medicine, Atlanta, Georgia, USA, are in the process of developing such resources through their ‘Climate Resources for Health Education Initiative’, which will be particularly useful for PH educators.24
CONCLUSION
There is a clear need for the integration of PH topics into medical curricula worldwide. There are various barriers to including new material into existing curricula. Through IMECCS, the authors have created a free online resource21 for medical students or faculty users to help overcome these barriers, and enable the introduction of PH topics into undergraduate curricula globally.







