Abstract
Background and Aim: Different techniques have been developed in order to optimise the practice of intubation with GlideScope® (Verathon Inc, Bothell, Washington, USA) video-assisted laryngoscope. This study aimed to demonstrate the use of a new, safe, and effective technique by inserting both the video-assisted laryngoscope blade and endotracheal tube (ETT) together.
Methods: A prospective, randomised study was conducted with 50 patients who were anticipated as difficult for endotracheal intubation, aged 18–90 years, with an American Society of Anesthesiologists’ (ASA) classification of Grades I–IV, and who presented for elective surgery. The patients were divided into 2 groups of 25 participants: an intubation with traditional GlideScope (TG) technique group, and combined GlideScope (CG) and ETT simultaneous insertion group. The optimal glottic view and the time-to-intubation were recorded. Postintubation airway trauma and both practitioners’ and patients’ satisfaction were documented. The categorical data are presented as a number and percentage and were subjected to Fisher’s exact or Chi-square test for analysis. The statistical significance was p≤0.05.
Results: The optimal glottic view was 64% in TG and 72% in CG (p=0.216); intubation was achieved within ≤15 secs in 22 patients in TG and all patients in CG (p=0.077); and 88% of patients in TG showed high satisfaction scores compared to 92% in CG (p=0.646). The practitioners’ satisfaction was 76% in TG and 96% in CG (p=0.042).
Conclusion: Simultaneous insertion of both the GlideScope blade and ETT could provide fast, effective, and safe endotracheal intubation.
INTRODUCTION
Airway management is a fundamental anaesthetic practice. Delay in securing an airway could be extremely serious in certain conditions. Therefore, many techniques and a lot of equipment are used to manage the problem. Anaesthetists must have the skills, different tools, and techniques of airway management. GlideScope® video-assisted laryngoscope (GVAL) has been a revolution in difficult airway intubation since its introduction in 2003. Recent studies have proposed the GVAL as the first choice for intubation in a difficult airway.1-6 Practitioners could encounter up to three problems when intubating with the hyperangulated blades of GVAL: the laryngoscope may be too close to the glottic opening, the practitioner may not direct the tip of the endotracheal tube (ETT) to enter the vocal cord opening, or they may be unable to advance the tip via the glottic opening.6,7 It was hypothesised that combined insertion of both the GVAL blade and ETT provides a fast, safe, and effective alternative to the traditional GlideScope technique. In this study, the authors aimed to adopt a new combined GlideScope technique to achieve improvement in these parameters during endotracheal intubation. The secondary objective was to optimise, if possible, the use of GlideScope and to reduce the risks and complications related to its use.
METHODS AND MATERIALS
This prospective, randomised, comparative study was conducted during the period from March 2017 to August 2018. Ethical approval was obtained from the Hospital Ethical Committee. Informed written consent from all patients was taken. A total of 50 patients aged 18–90 years with an American Society of Anesthesiologists’ (ASA) classification of Grade I–IV, anticipated difficulty in airway intubation, and who presented for elective surgery under general anaesthesia were enrolled in the study. Exclusion criteria included patients with unanticipated difficult intubation, airway trauma, airway pathology, bleeding tendency, emergency procedure, pregnancy, full stomach, or need for rapid sequence intubation. Additionally, patients unwilling to participate were excluded. All patients were informed about the study and written consent was obtained. Routine preoperative evaluation including medical history and physical examination was performed. Proper airway assessment and evaluation was carried out by an experienced consultant anaesthetist. All patients fulfilled the criteria of anticipated difficult intubation. Every patient had at least two criteria out of the history of difficult intubation, Mallampati Score III/IV, thyromental distance <6 cm, and neck circumference >40 cm. All patients were premedicated with ondansetron 4 mg and dexamethasone 8 mg intravenously. All patients received intravenous midazolam, at a dosage of 0.5–2.0 mg, in the holding area before moving to the operating room.
Patients were randomly selected and assigned to 1 of the 2 groups with 25 patients in each (TG and CG) using a computer-generated block randomisation program. The results of the allocation were kept in an opaque envelope in the operating room and were picked randomly by a designated person per patient. TG consisted of the patients who were intubated with GlideScope; the blade was inserted, followed by optimisation of the glottic opening, and finally ETT insertion via the mouth for tracheal intubation. In CG both the GlideScope and ETT were inserted at the same time, and the glottic opening was optimised for tracheal intubation.
After tracheal intubation the stylet was removed and ETT placement was confirmed by lung auscultation and end-tidal carbon dioxide and secured into place. The intubation procedure was performed by consultant anaesthetists with sufficient experience in using GlideScope (>10 years). The optimum view of the glottis (based on Cormack–Lehane [CL] system classification); the time-to-intubation (TTI), defined as the time needed from blade insertion to ETT placement; postintubation airway trauma; and practitioner and patient satisfaction were all assessed and evaluated. The primary outcome of the study was based on the TTI (divided into 3 categories: ≤15, 15–30, and >30 seconds) and CL classification (scored as excellent [CL=1], good [CL=2/3], and bad [CL>3]). The intubation time category was selected based on the observation that most complete GlideScope intubations could be performed in >30 sec, and the time was recorded by the assigned anaesthetic technician. The secondary objectives were postintubation airway trauma and satisfaction of the patients and practitioners. The satisfaction of the patients and practitioners performing the procedure was assessed using a 1–10 satisfaction score. Construction of a pilot questionnaire was carried out for both patients and practitioners to validate the scores.
Data entry and analysis using the Statistical Package for Social Sciences 21.0 (IBM, Armonk, New York, USA) was performed. For the purpose of sample size calculation, TTI was used as the primary outcome of this study. More than one trial for intubation was excluded from the study. No previous studies have compared this technique for the GlideScope with the traditional method; however, some studies compared the GlideScope with the conventional laryngoscope, using 25 patients per group. Assuming the same, a 2-sided Type 1 error of 0.05%, power of 80%, and sample size of 25 for each group was required to detect a significant difference. A total of 58 patients were enrolled and randomised in the study, however, 4 patients were excluded from each group, therefore, 50 patients were included in the study, with 25 in each group (Figure 1). The categorical data are presented as a number and percentage and were subjected to Fisher’s exact or Chi-square test for analysis. The statistical significance was considered at p≤0.05.
RESULTS
There were no significant differences between the two groups regarding the criteria of anticipated difficult intubation (Table 1).
The field of view and optimum access for intubation obtained during the procedure was assessed in both groups. It was divided into three categories: excellent, good, and poor view, based on glottic opening, centralisation, and epiglottic view. A total of 16 patients in TG (64%) showed an excellent field view compared to 18 patients (72%) in CG. The good field view was demonstrated in 8 patients (32%) in TG compared to 6 patients (24%) in CG. The differences between both groups regarding the excellent and good field view were not significant. In the study, 2 patients, 1 from each group, showed bad field view; however, the intubation was successful (Table 2).
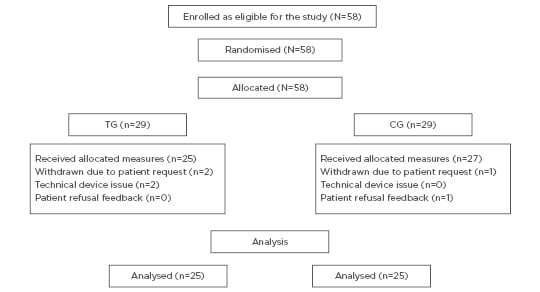
Figure 1: Diagram for sample size of the study.
CG: combined GlideScope®; TG: traditional GlideScope.
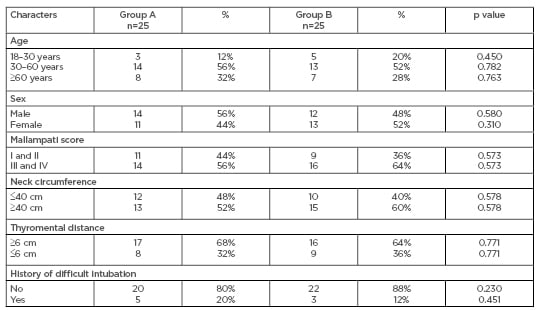
Table 1: Age, sex, airway parameters, and history of difficult intubation distribution.
The TTI from the beginning of the blade insertion to tube placement was assessed and divided into three categories: <15, 15–30, and >30 seconds (when more than one attempt was used). Most patients in the TG group (n=22) were successfully intubated within <15 seconds compared to all patients in CG. No significant differences were found (p=0.0767). Postintubation airway trauma was also evaluated. One patient in the study, from the TG group, experienced minor airway trauma because of upper lip injury, which only needed patient reassurance. There were no significant differences (p=0.322) (Table 2).
The satisfaction of the patients and practitioners performing the procedure is shown in Table 2. A satisfaction score of 1–10 was used. A score of 8–10, 4–7, and 0–3 were considered as high, fair, and bad satisfaction, respectively, <3 was also considered as a bad satisfaction score. The number of patients in the TG and CG groups who reflected a high satisfaction score was 22 (88%) and 23 (92%), respectively, with no significant statistical difference (p=0.646). Additionally, 76% of the practitioners reported a high satisfaction score during the procedures in TG compared to 96% in CG (p=0.042).
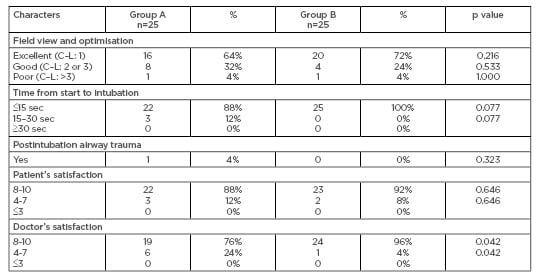
Table 2: Field view, time from start to intubation, postintubation airway trauma, and satisfaction.
C–L: Cormack–Lehane.
DISCUSSION
To the authors’ knowledge, this is the first study to evaluate this new technique for intubation with GVAL. It is crucial to consider laryngoscopy and intubation as two separate steps in airway management, because there is a possibility of facing difficulty in either step. Although GlideScope provided a good or excellent view of the glottis, the intubation was not always straightforward. Many types of stylets and ETT are used to increase successful intubation with GlideScope; however, there are numerous reports of airway trauma during intubation attempts.1,2 The good-to-excellent glottic view offered by GlideScope has markedly increased its popularity over recent years compared to direct laryngoscopy.3 Different studies performed in emergency departments have shown intubation using GlideScope requires significantly more time. The rates of successful intubation on first attempt are not significantly different between GlideScope and direct laryngoscopy.4
Successful ETT placement is usually best achieved by using a stylet formed in the shape of a hockey stick with a 90° bend. Once the tube enters the glottis the stylet is withdrawn by approximately 3 cm, followed by advancing of the tube slightly in order to prevent hitting the tracheal wall.5,6
The authors found that the differences between the TG and CG groups regarding the excellent and good field view were not significant. Only two patients in the study, one from each group, showed a poor field view, despite successful intubation. Evaluation of TTI, starting from the beginning of blade insertion up to ETT placement, revealed no significant difference. All the patients were intubated within 30 seconds in both groups. Postintubation airway trauma was also evaluated. One patient in the study, from the TG group, experienced minor airway trauma due to upper lip injury, which only required patient reassurance. This difference was not significant.
The satisfaction of the patients and practitioners performing the procedure was assessed using a 1–10 satisfaction score. There were no significant differences in patients’ satisfaction; however, the practitioners showed higher satisfaction in the CG group compared to the TG group (p=0.042). To improve ETT insertion through the mouth, Bacon et al.7 recommended GlideScope blade insertion to the left of the mouth midline. They also recommended ascending the scope to improve the laryngeal view and holding of the tube at the level of the connector to improve the manoeuvrability.7 Kramer et al.8 used the technique of ETT insertion through the mouth in a horizontal plane to GlideScope, and once the tube had passed the flange of the GlideScope, they rotated it to the vertical position. Cho et al.9 found that the insertion of the blade of the GlideScope nearer to the left corner of the mouth resulted in a larger space for ETT insertion. With this manoeuvre, Cho et al.9 noticed a potential avoidance of oropharyngeal mucosal injury. They also showed that introduction of ETT into the mouth prior to the insertion of the GlideScope may result in airway trauma.
Walls et al.10 reported a case in which, despite Grade 1 laryngeal view, they encountered difficulty in ETT insertion via the vocal cord to the trachea due to a steep posterior angle of the trachea with the laryngeal/glottic axis. They successfully completed ETT insertion using a sharply curved malleable stylet. Once the ETT entered the glottis it was then rotated 180° clockwise to enable passage down the trachea.10 A similar manoeuvre was used in another reported case by Xue et al.,11 after the failure of 90° rotation and relaxation of the tilt angle of the GlideScope. However, in reply to Walls et al.,10 Sharma et al.12 considered their manoeuvre during tube insertion and removal of the stylet as traumatic and suggested the use of another manoeuvre. Dow et al.13 used a reverse loading technique by loading the tube on the lubricated curved stylet as usual (inherent memory of the tube), followed by bending the distal stylet in the opposite direction to the inherent memory of the ETT, the tube was loaded and bent backwards against its natural curve.
A successful GVAL tracheal intubation has been performed by Bader et al.14 in 12 patients consecutively, with strict cervical stabilisation using a J-shaped tube. Direction of the ETT via the vocal cord could also be achieved by using a gum-elastic bougie or a long, semi-rigid catheter with a controllable tip.15,16 Dupanovic et al.17 adopted a gear stick technique by bending the proximal end of the stylet 90° to the right to form a handle, in addition to 90° curving of the distal tube anteriorly. They had held the handle like an automobile gear lever. They inserted the tip of the ETT via the right corner of the mouth.17 Corda et al.18 found that a jaw thrust manoeuvre was often helpful in improving the glottic view when the GlideScope is used; however, cricoid pressure showed no significant improvement. They recommend the use of jaw thrust as a first line manoeuvre to aid glottic visualisation and tracheal intubation during GVAL.18
The limitations of this study included the lack of blinding in the intubation methods, the need for sufficient experience in handling both GlideScope and ETT, and the need for sufficient mouth opening to cope with both the GlideScope blade and ETT.
CONCLUSION
Combined GlideScope techniques reduces the incidence of lost glottic view, reduces time to complete intubation, and reduces trauma as the ETT passed under vision with the blade. However, training is needed to synchronise the handling of GlideScope and ETT at the same time.








