Meeting Summary
Primary biliary cholangitis (PBC) is a progressive, immune-mediated liver disease that can be chronic and, in some cases, fatal. Cholestatic pruritus is a common symptom of PBC; however, it is consistently underassessed and undertreated. The pruritus can be moderate to severe, and persistent over years. Patients can experience changes in severity over the course of the day, with pruritus often being most troublesome in the evening and at night. Occurrence is associated with sleep disturbance, leading to daytime fatigue and mood disorders, as well as having a huge impact on health-related quality of life (HRQoL). Assessment of cholestatic pruritus should be carried out by healthcare professionals (HCP) at every consult with a patient with PBC to ascertain occurrence, severity, and the effect on HRQoL. Severity assessment can be carried out using a simple 0–10 numerical rating, or visual analogue scale, and the patient’s quality of life can be assessed with more involved measures, such as the PBC-40 tool. Patients can also track changes in symptoms over time on dedicated phone apps, and share these data at consults. Treatment for PBC is primarily with ursodeoxycholic acid (UDCA); however, this drug has not been shown to significantly improve cholestatic pruritus. Guidelines recommend anion-exchange resins as first-line treatment for pruritus, with pregnane X receptor agonists, oral opiate antagonists, and selective serotonin reuptake inhibitors also suggested as second/third-line treatment. Of note though, few of these have been specifically licensed for cholestatic pruritus and clinical trial data supporting their use remain limited. Other measures include training patients to stop the itch-scratch-itch cycle and the use of moisturising and/or cooling creams. At the American Association for the Study of Liver Diseases (AASLD) 2023 Liver Meeting in Boston, Massachusetts, USA, two HCPs with expertise in PBC, along with a patient representative, discussed these aspects of cholestatic pruritus, and how patients with this symptom can be recognised, assessed, and helped.
INTRODUCTION
PBC is a chronic, progressive, immune-mediated cholestatic liver disease that involves gradual intrahepatic bile duct destruction. In some cases, PBC may necessitate liver transplantation and it can be fatal if left untreated.1,2 Similar to most autoimmune diseases,3 PBC is far more common in females than in males, with up to 90% of middle-aged patients with the condition being female.4 At the AASLD 2023 Liver Meeting, this symposium concentrated on the symptom of cholestatic pruritus, which can occur in up to 81% of patients with PBC.5 The symposium involved two HCPs with expertise in PBC, Emma Culver, a Consultant Hepatologist and Honorary Senior Lecturer in Gastroenterology and Hepatology, John Radcliffe Hospital, Oxford, UK; and Stuart Gordon, a Clinical Hepatologist and Division of Hepatology Director, Henry Ford Hospital and Wayne State University School of Medicine, Detroit, Michigan, USA; plus a patient, Maria Morais, a registered nurse from Canada who underwent a liver transplant in 2021 as a result of her PBC.
Cholestatic pruritus typically occurs without a primary rash, though scratching may lead to secondary skin lesions. In one study of PBC, just over half of the patients with cholestatic pruritus rated the intensity as moderate to severe. In around a third of patients with cholestatic pruritus, symptoms can be persistent and chronic;6 however, levels and occurrence can fluctuate both between patients and in a single patient over the course of the disease, depending on the season, and throughout the day.7 Of note, while some studies have found no correlation between cholestatic pruritus occurrence and intensity and biological parameters of PBC severity,8 others have found that patients with clinically significant cholestatic pruritus had higher alkaline phosphatase levels, and more frequently had cirrhosis compared to those with no or mild pruritus.5,6
When cholestatic pruritus arises, it may be described by patients as ‘deep’ and ‘relentless’, being ‘prickly’ or like ‘needles’, and feeling like ‘bugs crawling’.7 “These are words that we should be listening for,” said Culver, “and realising that this is clinically significant to them.” Gordon discussed how “I’ve had patients describe it to me as the type of itch that, the more you itch, the more it scratches, the more you scratch, the more it itches, [so they try to] dig out their skin to try to get to the itch.” Morais described her own experience with cholestatic pruritus, which, she reported, started in her big toe, where, on scratching, it became “red, inflamed, on fire, irritated, [and] bumpy. I just couldn’t get rid of it,” she explained. Similar to Morais, for many, pruritus most frequently occurs in the limbs.9 However, Morais described how the pruritus she experienced also occurred “in other [parts] of my body, my belly, the sides of my abdomen, the tops of my hands, in-between my fingers, and there was absolutely nothing I could do personally to manage it.” Pruritus may also be more predominant in hotter and colder seasons, and can be worsened by contact with clothing.7,10
CHOLESTATIC PRURITUS, HEALTH-RELATED QUALITY OF LIFE, AND RELATIONSHIP WITH OTHER PRIMARY BILIARY CHOLANGITIS SYMPTOMS
Cholestatic pruritus can significantly impact HRQoL.5,11-14 Indeed, one study14 collated data which showed that HRQoL of patients with PBC and severe pruritus was equivalent to, or lower than, people with chronic obstructive pulmonary disease,15 Parkinson’s disease,16 end-stage renal disease,17 or heart failure.18 Morais’ experience reflected this and described how “overall my QoL was not great and [it was] very overwhelming in the whole other complexities of this autoimmune disease.” She discussed how “I was already very anxious [and] depressed about having this ‘sentence’ of cirrhosis and the itching just added to it. It became a psychological issue for me, because [I asked myself], ‘was I really that itchy’? It was uncontrollable and [I was] inconsolable. My social relationships started to be impacted to where I didn’t want to go out. I secretively was thankful for COVID that I didn’t need to see anybody. I was in a state of ascites, I was in a state of itching and scratching, and it was really embarrassing.” Morais also discussed how it impacted “my world, my work, my colleagues, others.” She reported people would look at her skin, maybe thinking it was contagious, and “that’s the last thing that you want, for people to avoid you, and you become more isolated.”
“It’s very rare that pruritus occurs on its own,” said Culver. Indeed, other PBC-associated symptoms include fatigue, cognitive problems, and emotional dysfunction, and there is a relationship between cholestatic pruritus and these other symptoms.19 For example, patients with pruritus and PBC report significantly higher fatigue scores compared to those with PBC but without pruritus,20 and almost a third of patients with severe cholestatic pruritus report severe depression.21 Studies have also found significant correlations between level of itch and higher median PBC-40 scores on all domains.22
For many patients with PBC, pruritus can be worse in the evening and at night.7,10 Indeed, in a study of patients with PBC, 65% of 164 patients reported worse pruritus levels at night, and 74% of 162 patients said pruritus interfered with sleep.7 Other studies have also highlighted problems with getting to sleep and waking up early attributed to cholestatic pruritus.9,23 Such issues were relevant for Morais who recounted how “sleep was also a great concern for me. Typically, in the evening after supper, I would start to itch and to scratch and I tried really hard [not to] and my husband was saying ‘stop that’, but I could not control it, and even my son [would say] ‘look what’s going to happen to your skin’.”
RECOGNITION AND ASSESSMENT OF CHOLESTATIC PRURITUS
Despite cholestatic pruritus being common in patients with PBC, it is often unrecognised in clinics and may not be discussed by patients or their HCPs (Figure 1).7,24 For example, one large UK-based study found that of 8,968 patients with PBC, 38% had not been assessed for pruritus within the previous 2 years.25 Previous studies have found even higher levels, with around two-thirds of patients never being evaluated for itch in some investigations.7,26 In fact, cholestatic pruritus was only recognised in the World Health Organization’s (WHO) International Classification of Diseases (ICD-11) in 2022, defined as “pruritus due to defective elimination of bile” (EC90.11).27 Having this recognition is important, explained Culver, “because it helps us in real time to record, to monitor, and to follow patients for this important symptom in the real world.”
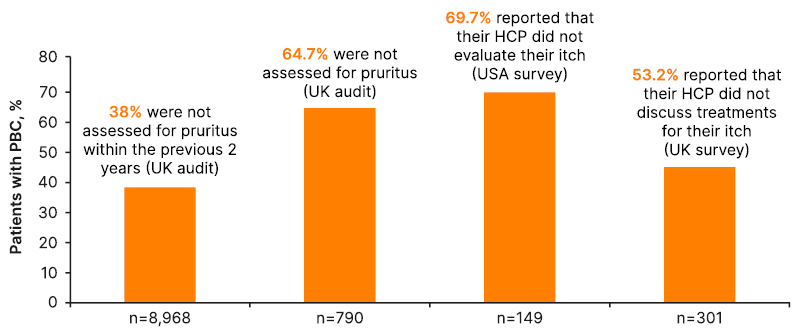
Figure 1: Underassessment of pruritus in patients with primary biliary cholangitis.7,24-26
HCP: healthcare professional; PBC: primary biliary cholangitis.
According to Culver, with regard to pruritus symptoms of PBC, “it’s important to be able to ask the question [and] to assess and evaluate patients when they come to the clinic.” Indeed, the European Association for the Study of the Liver (EASL) and UK-PBC/British Society of Gastroenterology (BSG) guidelines state that all patients with PBC should be evaluated for cholestatic pruritus.2,28
Culver suggested that one simple question to start with “is actually to say to a patient, ‘are you experiencing itch?’. Often we don’t necessarily do that.” The point of evaluating pruritus, according to Culver, is that “we want to get an idea [of] how it’s impacting them. Is it impacting their sleep? Are they able to do daily activities? Do they scratch until they bleed?”
Culver went on to discuss how HCPs should “think about how we might both numerically score the intensity [of pruritus] and think about how it impacts on everyday life.” This can be carried out with simple and rapid measures, such as unidimensional intensity visual analogue or numerical rating scales (Figure 2). With these, patients are asked to draw on a 10 cm line, or rate from 0–10, how bothersome the pruritus is, with 0 being ‘no itch’ and 10 being ‘worst imaginable itch’.29,30 Such scales can be used to rate both average and worst itch scores over a stated length of time. One study utilising a visual analogue scale suggested that clinically significant severe to very severe pruritus would be any score ≥7.29 The importance of using such scales, said Culver, “is the reproducibility, so each time you see [a patient] in clinic or on a regular basis, you should be repeating that score to get an idea of how things change over time.”
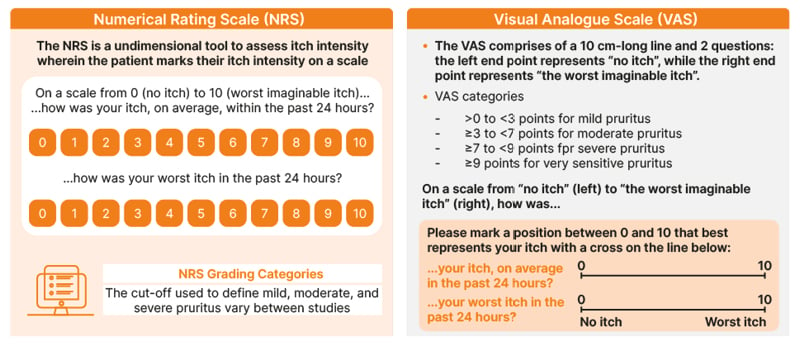
Figure 2: Cholestatic pruritus assessment tools.29,30
NRS: numerical rating scale; VAS: visual analogue scale.
A tool to assess the quality of life of a patient with PBC is the PBC-40, a validated 40-question tool that investigates the impact of PBC across six domains: general PBC symptoms, itch, fatigue, cognition, emotional realms, and social life. For the itch domain, PCB-40 asks a patient to rate if pruritus disturbed their sleep, if they scratched their skin so much they made it raw, and if they felt embarrassed by their pruritus. Answers are scored from 1 (never) to 5 (always), for a total score of 3–15.31
Gordon highlighted how measures, such as the PBC-40 or visual analogue or numerical rating scales, are not routinely used in the clinic but “we should start implementing this into our clinical practices and start asking patients to complete a questionnaire, to tell us more about their degree of pruritus.” Also important though, discussed Culver, is “to do a clinical exam and look for excoriations of the skin. Often, patients will tell you they’re not that itchy, but they’re sitting there actually scratching themselves in front of you, so it’s important to be able to document that when we’re thinking about evaluating the pruritus itself.”
An interesting discussion point at the end of the session was: “How can we get patients and their HCPs to be more engaged in the discussion and who should lead it in the clinical setting?” Morais said that “for me, it’s a shared responsibility between the patient and the healthcare provider, but certainly, as a patient, we’re not aware of what the disease progression could be. I’m not sure what I’m going to feel or what kind of treatments [there] will be along the way, so the initiation has to be on the healthcare providers’ side.”
Culver agreed and discussed how “for the HCP, it’s really important that they acknowledge the [patient’s] symptoms and ask from the beginning about those symptoms. There are different ways of being able to bring that to the table, including apps where patients can potentially monitor their symptoms over time and bring it with them so they can show the physician.” Indeed, the PBC Foundation has a ‘self-care app’ where patients can log their symptoms daily and thus track them over time. The app plots the data on a graph so an HCP can use the data generated to provide and track the utility of care prescribed for cholestatic pruritus.32 Morais discussed how “I kept a journal of when my itch was the worst, the most intense, and where it was. I took a picture of my toe, just out of curiosity and record keeping.” She suggested that, at the very least, a patient with PBC should make some notes they can bring to their next appointment.
When asked: “What barriers do you feel that both patients and HCPs encounter when we talk about pruritus?” Gordon discussed how “from the HCP perspective, we’re sort of overwhelmed when a patient comes through our clinic [and forget] to ask all the correct questions. We’re looking at their bone health, at sicca syndrome, their thyroid function, and it’s maybe just not occurring to [HCPs] on a regular basis, each time a patient comes in, to continue to ask those three words ‘do you itch?’.”
Gordon suggested that “maybe there should be a formal checklist, maybe there should be a nurse intake person to be able to ask all of these questions.” He explained how “for a lot of patients, their eyes will light up when they’re asked [the question ‘do you itch?’ and] say ‘no one’s really asked me that before.’ It’s just remembering to ask the proper questions, these are barriers that we [don’t] recognise do exist.” Gordon also recounted how patients might underestimate the degree of their pruritus, giving the example of a patient who was kept awake at night by this symptom but didn’t spontaneously report it as severe. “You [need to] engage them to find out if this is quite significant and impairing their QoL,” he said.
Morais added that “maybe the patients don’t have the confidence to bring things up in a short period of time where their focus is perhaps on how PBC is going to affect them long-term. If you talk about cirrhosis and liver damage, patients are very tense about that.” Morais also pointed out that a patient “might come from a cultural perspective [where] the physician is the authority and you don’t question and you wait to be questioned, so I think the more dialogue that can happen the better, but it’s how the healthcare provider can put [the patient] at ease.”
TREATMENT FOR CHOLESTATIC PRURITUS
PBC treatment algorithms focus on disease-modification, with first-line treatment being UDCA.2,10,33 According to Gordon, UDCA is, “as we all know, life-saving. It improves histology, etc., and is the first line of therapy. But,” he continued, “there’s sort of a misperception out there on the part of many clinicians that cholestatic pruritus is improved with UDCA.” Indeed, this is reflected in several studies of this therapy that have not shown a significant impact of UDCA on cholestatic pruritus reduction.34,35
As a condition associated with PBC, cholestatic pruritus is often undertreated. For example, in TARGET-PBC, a USA-based longitudinal observational cohort study, 33% of 63 patients with PBC with moderate-severe itch reported that they had never received any treatment for their itch. Of the 51% that were currently receiving an anti-pruritic treatment, only approximately 25% were prescribed guideline-recommended first-line therapy. Overall, 64% of patients had taken antihistamines,5 which, while cholestatic pruritus is not histamine-related,36 have been shown to provide some relief from pruritus,7 although this is potentially due to sedative properties.10
Culver highlighted how traditional treatment paradigms for PBC may suffer from low levels of patient contact, such that once UDCA is prescribed, a patient might not be asked back to assess liver function for another 12 months, which is too infrequent to adequately monitor symptoms such as pruritus. A new treatment paradigm recently suggested by Levy and colleagues includes more personalised care that assesses not only liver function tests, but also associated symptom occurrence (Figure 3). This paradigm also includes talking to patients about their aspirational goals, such as achieving a normal HRQoL.37 Culver discussed how it’s important to “think about how we might manage the pruritus both in terms of pharmacotherapy, and in terms of non-pharmacotherapy coping mechanisms.”
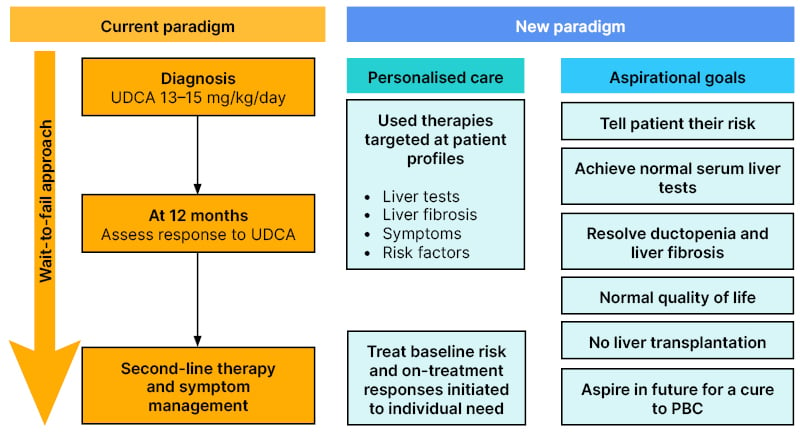
Figure 3: New primary biliary cholangitis treatment paradigm.37
This figure has been taken from Levy C et al. Clinical Gastroenterology and Hepatology. 2023;21:2076-87 and is available under the Creative Commons CC BY-NC-ND 4.0 licence which permits non-commercial use of the work as published.
PBC: primary biliary cholangitis; UDCA: ursodeoxycholic acid.
One reason for difficulties in supplying a suitable treatment for cholestatic pruritus may be because the exact causative factors are not fully elucidated. Bile acid accumulation in the blood plays a role; however, there is not a strong correlation between bile acid levels and severity of pruritus.2,10,28,38 Pruritus intensity is correlated with levels of lysophosphatidic acid, and/or it may be associated with increases in endogenous opioids, as shown in patients with PBC-related pruritus.10
EASL, AASLD, and the Asian Pacific Association for the Study of the Liver (APASL) all recommend anion-exchange resins, such as cholestyramine, as first-line treatment for pruritus.2,10,33 However, limited clinical trials of such agents for this indication have been carried out, and adverse events include diarrhoea, vomiting, constipation, and abdominal pain.39 While EASL and APASL recommend a pregnane X receptor agonist, such as rifampicin, as second-line treatment, and an oral opiate antagonist for third-line treatment,2,33 the AASLD places both of these agents, along with selective serotonin reuptake inhibitors, in the second-line.10 Of note, though, these medications are not licensed for cholestatic pruritus.39 At the end of the treatment lines for persistent and intractable cholestatic pruritus, EASL suggests liver transplantation.2
According to Gordon though, “clinically and anecdotally, these are difficult treatment regimens [that] have evolved over the decades. The [problem with the] use of cholestyramine is timing so that it doesn’t interfere with other agents, and, of course, [there is] a lot of gastrointestinal upset.39 There’s always concern about using a pregnane X receptor [agonist, as] sometimes it works, sometimes it doesn’t, [and] we’re always concerned about some of the literature suggesting cholestasis and liver injury itself, [especially] using it in patients with more advanced liver disease, or using it for a longer period of time.”39 Gordon concluded that “there are various guidance documents and suggestions out there, but still some missing elements and inadequate treatments overall.”
Culver also suggested to “think about how you can incorporate things like mindfulness within treatment. There are also a number of clinical trials now that are open to patients and it’s really important for those patients, where we have no U.S. Food and Drug Administration (FDA) approved medication, and who are persistently itchy, to think about the role of clinical trials and how we might engage our patient population to find a better therapy.”
Other therapy recommendations, which may provide some symptom relief, include behavioural training to stop the itch-scratch-itch cycle; supervised ultraviolet light exposure; relaxation techniques; practical suggestions such as wearing loose clothing and keeping fingernails short; using topical agents (e.g., camphor, menthol); applying moisturisers and emollients; and bathing in tepid water.2,10,40 However, Morais discussed how for the pruritus she experienced, “there was nothing I could do to get rid of it or manage it. I tried mild soaps and moisturisers; temporary, hardly any relief. I spent a whack of money on nothing and I still have [those] all in my cupboard. I look at that and it makes me very sad that there was nothing for me at that time that really worked. I did the typical trying to scratch with a pad, air it out, salt water.” Morais explained how “most PBC patients go to a cold application to calm down the itch. Because of my Raynaud’s, the last thing I wanted to do was use cold so I did what should not be done, I tried to put really, really hot water to that point of not feeling it anymore, which is extremely dangerous, but that for me was what I needed to do. I ended up seeking medication, I tried two different things [but they] did not help.”
CONCLUSIONS
Culver concluded by saying that for patients with PBC, “we have to have a much more holistic idea of care, we have to think about telling the patients their risk, and about trying to normalise and improve QoL with a particular concentration on the symptoms that matter the most to them, which are itch and fatigue, and how it might affect them in terms of social isolation, and their ability to do their daily activities. That’s in a line alongside what we talk about a lot, which is normalising liver function tests and preventing transplantation.”







