Meeting Summary
Symptoms of the progressive cholestatic liver disease primary biliary cholangitis (PBC) include pruritus and fatigue. Pruritus can persist chronically in at least one-third of people with PBC and can range from mild to severe, with fluctuations over time, including on a daily basis. Proposed causative factors for PBC-associated pruritus include bile acids, lysophosphatidic acid (LPA), and endogenous opioids, with proposed symptom mechanisms linked to increases of these substances, or associated pathways. All offer potential routes for drug treatment to help alleviate pruritus in some patients. PBC-associated pruritus can have a significantly detrimental effect on a person’s quality of life (QoL) due to a sometimes constant feeling of ‘bugs crawling’ on their skin, and the need to ‘tear my skin off’. Pruritus may lead to secondary skin lesions, embarrassment, and social isolation. Pruritus is associated with sleep deprivation and subsequent daytime tiredness and fatigue, as well as depression, and sometimes in the worst cases, leading to suicide. Treatments for PBC-associated pruritus include bile acid sequestrants, rifampicin, opioid antagonists, sertraline, and gabapentin, as well as topical moisturisers, behavioural changes, and ultraviolet light therapy. Though not currently approved for such, ileal bile acid transporter (IBAT) inhibitors are undergoing clinical trials, as success in alleviating pruritus is shown in similar conditions. In patients where PBC-associated pruritus is very severe, liver transplantation is a consideration. At the 2023 European Association for the Study of the Liver (EASL) Congress, leading experts in the field of PBC, including clinician-researchers, a nurse specialist, and a representative from the PBC Foundation, highlighted the importance of discussing, assessing, and treating pruritus in people with PBC, using a holistic approach to understanding and caring for this QoL-affecting symptom.
Introduction
Symptoms of PBC, a chronic, progressive, immune-mediated, cholestatic liver disease arise due to gradual destruction of intrahepatic bile ducts.1 PBC predominantly occurs in middle age, although it can affect people of all ages, and is up to nine times more common in females compared to males.2
Cholestatic pruritus as a symptom of PBC can occur in up to 81% of patients,3 and may persist chronically in at least 35%.4 However, pruritus occurrence shows both inter- and intra-individual variation, with severity fluctuating and not necessarily related to PBC stage or activity.5 For many, pruritus primarily arises in the limbs, especially the soles of the feet and palms of the hands.6 Typically, pruritus occurs more often and is more intense in the evening,6,7 and it may be exacerbated by contact with some fabrics, especially wool; by heat; during pregnancy; during the premenstrual period; and when taking hormone replacement therapy.5,7,8 There is no primary rash associated with cholestatic pruritus;5 however, even though for many scratching does not relieve the itch sensation, patients may persist with scratching to the point of creating secondary skin lesions.6,8
Over two symposia, the experience and treatment of pruritus in people with PBC were discussed by leading experts in the field. They included the clinician-researchers David Jones, Newcastle University, and Newcastle Hospitals NHS Foundation Trust, UK; Cynthia Levy, Division of Digestive Health and Liver Diseases, Schiff Center for Liver Diseases, University of Miami, Florida, USA; Kris Kowdley, Elson S. Floyd College of Medicine, Washington State University, Pullman, USA; Alan Bonder, Division of Gastroenterology and Hepatology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts, USA; Kathryn Houghton, a hepatology research nurse and autoimmune specialist nurse; and Robert Mitchell-Thain, CEO of the PBC Foundation, Edinburgh, UK.
Potential Causative Factors for Cholestatic Pruritus
Cholestatic pruritus occurs when itch receptors in the skin are activated internally and the itch signal is transmitted to the thalamus, where it triggers the itch sensation (Figure 1).9 Several causative factors for the triggers of this sensation in PBC are postulated. As PBC is a disease of the bile ducts, pruritus may occur due to accumulation of bile acids in the blood and skin. Indeed, ingestion of bile acids can induce pruritus in healthy volunteers, or worsen it in patients who are cholestatic, and cholestatic pruritus can be reduced through bile acid sequestrants. However, pruritus occurrence and extent do not necessarily correlate with bile acid levels, and bile acid sequestrants do not reduce this symptom in all patients.7,10-14
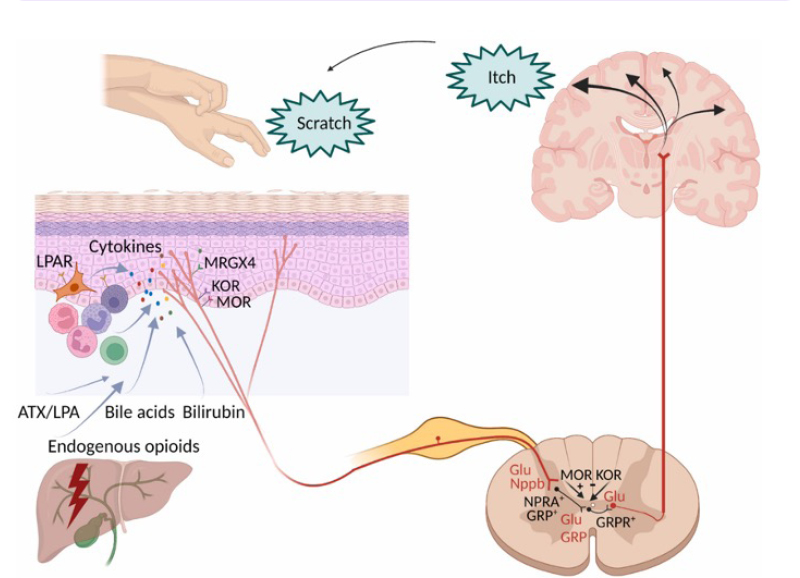
Figure 1: Mechanism of cholestatic pruritus.9
Adapted from Düll MM, Kremer AE.9
ATX: autotaxin; Glu: glutamate; GRP: gastrin-releasing peptide; GRPR+: gastrin-releasing peptide receptor; KOR: k-opioid receptor; LPAR: lysophosphatidic acid receptor; LPA: lysophosphatidic acid; MOR: m-opioid receptor; MRGX4: MAS-related G protein-couple receptor, member X4; Nppb: neuropeptide natriuretic
polypeptide b; NPRA: natriuretic polypeptide receptor.
Another potential cause of cholestatic pruritus is LPA, as activity of autotaxin, the enzyme that hydrolyses LPA from its precursor molecule, correlates with PBC-associated pruritus intensity, and injection of LPA into mice leads to dose-related pruritus. There may also be a role for endogenous opioids, as these are increased in many patients with PBC pruritus, and this symptom can be lessened by opiate antagonists.7
The Patient Experience of Primary Biliary Cholangitis-Associated Pruritus
“PBC-associated pruritus,” Jones said, “is a real problem in a significant group of people but is one that we are perhaps not taking as seriously as we should do, and the people who lose out with that are the patients.” In fact, said Mitchell-Thain, the PBC Foundation has talked to patients “that have been treated for tactile hallucinations or as self-harmers, because of what’s happening inside their own body.”
“Itch is indiscriminate,” highlighted Mitchell-Thain, when discussing an analysis of a PBC Foundation survey including 498 respondents that showed that itch occurred in both males and females, in participants of any age (31–70 years), and regardless of how many years they had been diagnosed with PBC.15 “Itch is more than just itch, though,” they said, “itch is days and days of torture, thousands of thousands of ants and spiders crawling under your hands, your ears, absolutely everywhere.” In confirmation of this, a survey of 201 patients with PBC-related pruritus found that 35% agreed that it was akin to ‘bugs crawling’, 29% responded that the symptom was ‘deep and relentless’, and 18% said it made them want to ‘tear my skin off’.5 As such, Mitchell-Thain asked of healthcare professionals that “when a patient talks to you about their itch, hear them, see them, treat them.”
“Severe itch,” said Jones, “has a really dramatic effect on people.” Using a measure of health utility that assesses QoL,16 a study of 147 people with PBC found that baseline health utility value in participants with severe pruritus17 was similar to patients with severe Parkinson’s disease,18 with both being around 0.5 on a scale of 0–1.17,18
Several studies have found pruritus affects people in several domains, including sleep, mood, and fatigue. For example, in a study of 211 people with PBC, those with pruritus scored significantly worse (p<0.0001) than those with no or mild pruritus on several PBC-40 measures (described below) domains, including fatigue and cognitive, emotional, and social areas.19 With the latter in mind, other studies investigating PBC-associated pruritus have illustrated how it can lead a patient to socially isolate, as they feel self-conscious about scratching, which can impact QoL.20,21
Sleep deprivation in people with PBC-associated pruritus, reported Mitchell-Thain is “a form of torture that can profoundly affect you physically, emotionally, and psychologically.” In a survey by the PBC Foundation, including 395 patients with PBC, 58% reported itch occurring daily, and 72% said they had sleep disturbances.22 Another survey, based on data from the GLIMMER study of an IBAT inhibitor, found that all participants with PBC (n=147) had at least mild sleep interference, with 66% of 35 patients with severe pruritus and 8% of 76 patients with moderate pruritus reporting severe sleep interference.23
Fatigue can also be a symptom of PBC, with 86% of 227 respondents to a PBC Foundation survey reporting this symptom.24 However, Houghton suggested a patient may not know fatigue is related to the pruritus they are experiencing. Bonder reported findings from their autoimmune clinic and registry, where patient demographics, medical, and PBC diagnosis data are captured alongside results of patient QoL surveys. In an analysis of survey data including 118 patients with autoimmune hepatitis (AIH), 31.4% of whom also had PBC, lower scores on fatigue, systemic symptoms, and emotional domains were associated with significant QoL impairment.25 Another analysis showed that poor treatment adherence was more common in patients with AIH and PBC, compared with those with AIH alone, and was significantly associated with lower health-related QoL, which was related to fatigue and systemic symptoms.26
In the PBC Foundation survey discussed above, 31% of 227 people with PBC reported mental health issues.24 Another survey found that 43% of 35 patients with severe pruritus, 11% of 76 patients with moderate pruritus, and 20% of 35 patients with mild pruritus reported moderate or severe depression.23 This was considered as very important by Jones, who recounted how they “knew people who find life intolerable because of their itch, and there have, sadly, been people who have taken their own lives because of it.”
Assessing and Tracking Primary Biliary Cholangitis-Associated Pruritus
Despite the above figures, in an analysis of 8,461 UK hospital-based patients with PBC, 38% did not undergo any assessment of pruritus.27 In another study, 70% of 149 patients said their physician did not evaluate itch.5 Similarly, in the PBC Foundation patient survey of 227 patients, only 60% reported being asked about their symptoms by a clinician in the previous 12 months.24
As PBC-related pruritus is not associated with liver disease severity, occurrence may be perceived by physicians as well-controlled when looking at lab values, even if symptoms interfere with a person’s QoL.28 As such, the speakers discussed various ways a person’s experience of pruritus could be measured. This is vital as, according to Houghton: “The patient’s view of the itch is very subjective, so it is important that you get their view, and not your view, of what you think their itch is.” Indeed, one study showed a mismatch between physician and patient ratings of pruritus occurrence and severity, with concordance rates for mild or moderate pruritus being lower than for severe or very severe pruritus.29
Most simply, Levy discussed how in the clinic, just asking the patient whether they are experiencing pruritus, and whether it is interfering with their QoL, may be enough to gauge if the symptom needs addressing. However, to record the occurrence and level of pruritus, Kowdley suggested: “Itch severity measurements can provide objectivity and a true assessment of a patient’s health and QoL.” They further discussed how, “while the patient is in the waiting room, we give them a visual analogue scale of 0−10, where all they have to do is draw a line as to where their itch is, because how they report the itch when you ask them can be very different to how they record it on a form.”
For this, a numeric rating scale is available, where 0 is no itch and 10 is the worst itch imaginable.30 Itch can also be evaluated using a Patient Global Impression of Severity scale, ranging from Absent to Very Severe.30,31 Levy also recalled how utilising a 0−10 numeric rating scale at each consult can help with comparing pruritus levels over time, and gauge the impact of a treatment, with a 3−4 point reduction being, in their opinion, very clinically relevant.
To investigate how PBC symptoms affect a person, the disease-specific PBC-40 QoL measure contains 40 PBC-related questions, including how often itching disturbs a person’s sleep, whether scratching the itch makes the skin raw, and how often a person is embarrassed because of scratching. Frequency (in the past 4 weeks) is scored from 0 (no itch/does not apply) and 1 (never), to 4 (most of the time) and 5 (always).32,33 The pruritus-specific 5-D itch score can also be used to assess this symptom more thoroughly.34
According to Kowdley, “if you have something the patient can do between visits, especially that can track sleep, we might be able to do even better.” In fact, the PBC Foundation has an app that patients can use to track their symptoms daily over time. The app can graph the data, and a patient can show this to their clinical team, and use it for self-care.35
Measuring symptoms using such tools, suggested Jones, “gives you something to talk about, and it also validates the patient’s experience.” Above all, agreed Kowdley, you need to provide hope, and the patient needs to feel they are believed, and that their concerns about the impact of pruritus on their daily life are taken seriously.
Management of Cholestatic Pruritus in Primary Biliary Cholangitis
The above findings regarding cholestatic pruritus, according to Jones, prompt the question of whether enough priority is being given to managing PBC symptoms and their impact on patients. Indeed, in a study including 211 patients with PBC-associated pruritus, 33% did not receive any treatment for this symptom.3 In one of the PBC Foundation surveys, when discussing itch with their clinician, only 45% of 227 respondents said they were prescribed treatments, and 32% were given information about remedies to try. Still, only 6% were informed of helpful lifestyle changes, and 9% reported the symptom of itch was dismissed as something else, or that they were not believed or taken seriously. Of the 32% of the 227 patients who said they did not raise the issue of itch during their appointments, 35% said they did not think anything could be done to help it, and 12% said there was not enough time in their appointment.24
Findings such as these, said Jones, raise the need for a patient-centric approach, where symptoms are readily assessed and managed in addition to starting disease-modifying therapy. “I do not think it is a stretch,” Jones discussed, “to imagine that if we can stop people suffering from severe itch in PBC, that we can improve their health utility and QoL substantially.”
While the guideline-recommended first-line treatment for PBC, ursodeoxycholic acid, aids some PBC symptoms, it is not shown to improve pruritus.7,36 EASL, the American Association for the Study of Liver Diseases (AASLD), and The British Society of Gastroenterology (BSG) suggest treatment pathways for cholestatic pruritus in PBC. However, these also may not be effective for all patients, and not all have undergone formal clinical testing for PBC. First-line medications are the bile acid sequestrants cholestyramine, colestipol, and colesevelam. For refractory pruritus, rifampicin is the second line treatment, followed by oral opioid antagonists, such as naltrexone and nalmefene, and then the selective serotonin uptake inhibitor sertraline and the anticonvulsant gabapentin.7,13,14
If the patient does not respond to these, there may be clinical trials they can be entered into.7,13,14 In a recent PBC Foundation patient survey (n=227), just over two-thirds of respondents said they would consider participating in a clinical trial; however, only 15% reported they had had a conversation with their clinician about such participation.24 If pruritus is severe, liver transplantation can be considered.7,13,14 While the latter is rare, of note, Mitchell-Thain was speaking at the symposia on behalf of Mo Christie, the Head of Patient Services at the PBC Foundation, and a person with PBC, who agreed to their story being shared. They had been scheduled to appear at this symposium, but were unable to, as they had recently undergone surgery following a liver transplant, due to untreatable pruritus.
Other recommendations, that may mitigate itch but not provide a cure, include training that can help stop the itch-scratch-itch cycle and being taught relaxation techniques. Potential pruritus-relieving treatments include moisturisers and emollients (not water-based); topical agents, such as menthol and camphor; applying moist, cooling skin wraps; and bathing with tepid water. Pruritogenic medications, such as narcotics, should be avoided. Behavioural measures include being in a cool, but not dry, environment; keeping nails short; and avoiding tight or sticky clothing.13,37 Another therapy is controlled ultraviolet exposure,13,37 with Houghton discussing how they have had success in some patients when they combine medication with light therapy under a dermatologist’s guidance.
Of note from PBC Foundation data, people with cholestatic pruritus may be prescribed treatments that are not recommended, such as, in a survey of 395 patients, antihistamines, which were prescribed to approximately 30% of respondents.22 A PBC Foundation analysis of their mobile app data (n=498) showed that many patients still experienced pruritus, despite being prescribed a treatment for PBC (Figure 2A), or a treatment for pruritus (Figure 2B).15
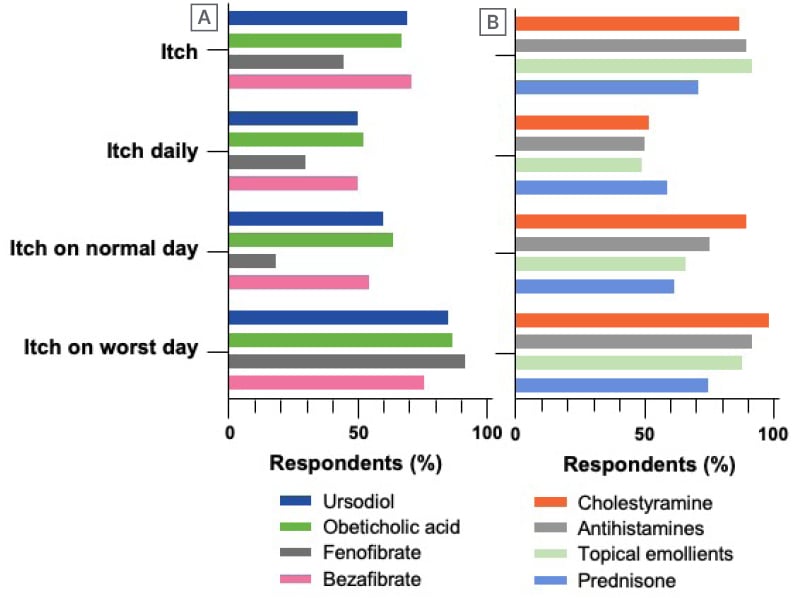
Figure 2: Current therapies for primary biliary cholangitis, or pruritus reported on the PBC Foundation mobile app by patients with primary biliary cholangitis (n=498).
A) Primary biliary cholangitis; B) pruritus.
Itch: itch occurring on any day; itch daily: itch occurring at least once/day; itch on normal day: itch level moderate-to-severe on a typically day; itch on worst day: itch level moderate-to-severe on worse day.
Although not presently indicated for PBC-associated pruritus, Levy discussed the use of IBAT inhibitors, as such treatments have had success in pruritus treatment in the paediatric conditions of progressive familial intrahepatic cholestasis and Alagille syndrome. Two IBAT inhibitors are currently under investigation in adults with PBC (Table 1).38,39
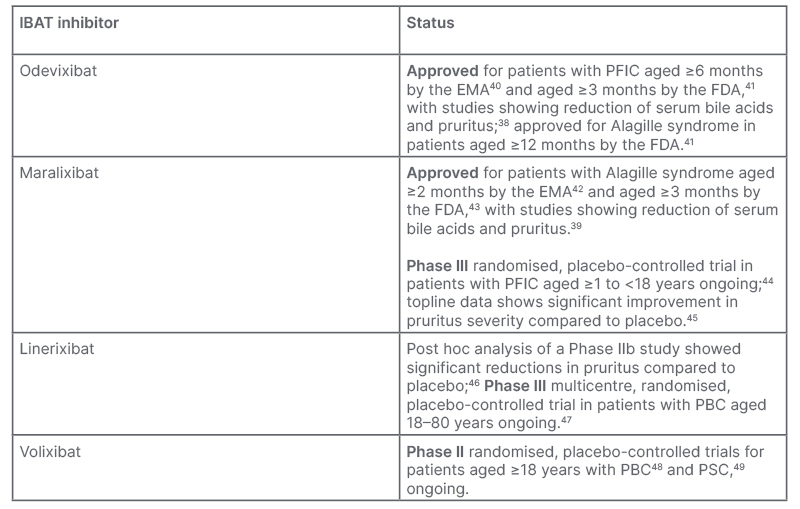
Table 1: Ileal bile acid transporter inhibitors approved and under investigation for the treatment of cholestatic pruritus.
EMA: European Medicines Agency; FDA: U.S. Food and Drug Administration; IBAT: ileal bile acid transporter; PBC: primary biliary cholangitis; PFIC: progressive familial intrahepatic cholestasis; PSC: primary sclerosing cholangitis.
IBAT inhibitors work by decreasing the amount of bile acid re-uptake in the terminal ileum, which occurs as part of enterohepatic circulation following excretion of bile acids into the bile duct, then the duodenum. As the use of IBAT inhibitors increases faecal excretion of bile acids,50 this may lead to some gastrointestinal adverse effects. In Phase II trials of maralixibat for patients with PBC or primary sclerosing cholangitis, approximately 81% of participants experienced treatment-emergent gastrointestinal adverse events.51,52 In linerixibat clinical trials in people with PBC and pruritus (n=147), diarrhoea and abdominal pain led to drug discontinuation in a dose-dependent manner of 14% of the participants who received the active drug (n=111).46
Holistic Care for People with Primary Biliary Cholangitis-Associated Pruritus
“Empowering patients to know what they’re dealing with, and what they’re expecting from their disease, is so important,” stressed Bonder, who reiterated: “We need to take a holistic view in PBC; we need to treat not only the disease but the patient, and we need to have a really good physician-patient relationship.” This includes sharing goals and action plans. Bonder suggested that when managing people with PBC who are experiencing pruritus and fatigue, to focus not only on laboratory test results, and not be shy to ask and discuss these symptoms. Houghton recounted the value of having telephone consults every 2 weeks between 3-monthly clinical visits, and how they use these as an opportunity to explore how a treatment prescribed for pruritus is working, and change it if needed. This means, Houghton mentioned, that “when they come back to the clinic, we’re getting closer to itch management, rather than having a 3-month gap with no contact with any physicians.”
Houghton shared how, in their centre in Newcastle, they have the ‘TRACE’ approach to patient management in PBC: TReatment of exacerbating factors, such as pruritus, anaemia, hypothyroidism, or vitamin D deficiency; Amelioration of associated problems, such as autonomic dysfunction, sleep disturbance, or depression; Coping strategies, including education, social interactions, and regular exercise; and Empathy.7,53 “You’re probably all aware of this,” said Houghton, “but whether you can do it is another thing,” with time being a limiting factor in a usual consult. As such, the Newcastle Hospitals NHS Foundation Trust has a dedicated fatigue clinic where they have time to discuss this symptom and its exacerbating factors. Here, long-term management is discussed, taking into account the broader impacts fatigue can have on a person’s daily life. This may be carried out by a nurse specialist, who, as Houghton states, “may have more time, and (to whom) patients will often tell things that they won’t tell a doctor.”
Bonder also discussed how patients should also be guided to advocacy groups, such as the PBC Foundation,54 for support, and to help manage symptoms. “Sometimes my patients are shy to share common symptoms with me, but when they go to patient advocacy websites or social media pages, they are helping to get resources, and at the next appointment they are happier to share symptoms.”
Conclusion
Cholestatic pruritus is common in patients with PBC, and should be assessed and discussed by a healthcare professional at every visit, as it is often under-recognised and under-treated. This is despite how it can sometimes dramatically impact a patient’s QoL, including associations with sleep disturbances, fatigue, and depression. There are several tools, including those specific to PBC, to health-related QoL, and to pruritus, that could aid assessment and discussion. Several pruritogenic compounds have been implicated in the development of cholestatic itch, including serum bile acids. Treatments leading to reduction of bile acid levels appear to be associated with clinical improvement of itching, and are currently in development for PBC-related pruritus. Treatment is through provision and suggestion of behavioural modifications, and a stepwise approach to medical management.







