ONE IN FIVE patients hospitalised with cirrhosis succumbs to the condition, highlighting its grave prognosis. Infections, predominantly from multidrug-resistant organisms (MDROs), play a critical role in acute decompensation and acute-on-chronic liver failure (ACLF). Bacterial breaches in immune defences and ineffective clearance exacerbate this risk, placing antimicrobial therapy at the heart of treatment strategies. However, antimicrobial resistance presents escalating challenges, particularly in Europe and globally, necessitating innovative approaches.
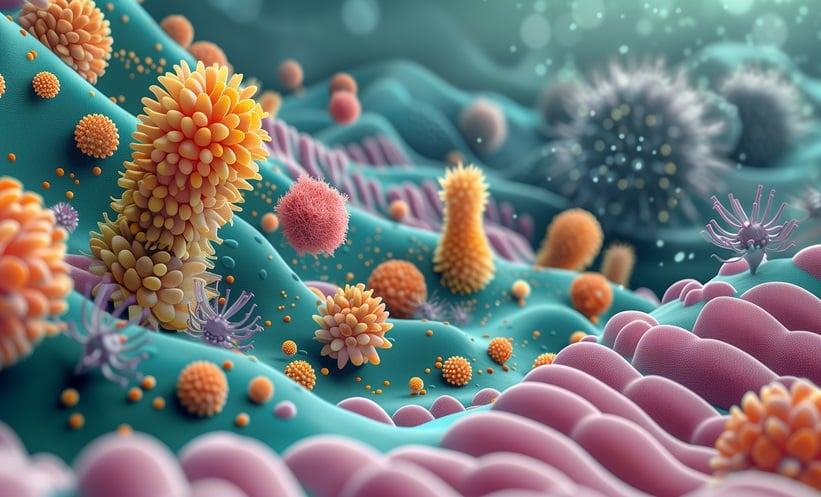
Cirrhosis-associated immune dysfunction (CAID) heightens infection susceptibility through low-grade systemic inflammation and gut-liver axis alterations, including microbiome disruption and increased intestinal permeability. Gut dysbiosis, characterised by imbalances in microbial communities, fosters MDRO proliferation and worsens clinical outcomes. Emerging evidence underscores the interplay between gut and oral microbiomes, with microbial translocation from the mouth to the gut linked to decompensation. For instance, periodontitis, present in up to 68% of cirrhotic patients, has been implicated in worsening liver function. Intriguingly, periodontal therapy may mitigate systemic inflammation and improve disease markers.
Advances in shotgun metagenomic sequencing (SMGS) have enabled deeper insights into microbiome changes. Studies reveal reduced microbial diversity in the oral and gut niches as cirrhosis progresses, with pathogenic bacteria such as Enterococcaceae and Veillonellaceae gaining dominance. These shifts correlate with functional alterations, including disrupted metabolic pathways and increased ammonia production, a contributor to hepatic encephalopathy.
The resistome – genes conferring antimicrobial resistance – represents a critical area of study. Gut ARGs, amplified by inflammation and dysbiosis, pose significant threats, while the oral resistome appears more stable. These findings suggest selective pressures beyond antibiotic use, driven by disease severity.
Future research must adopt a longitudinal, multicentric approach to disentangle causative mechanisms and explore precision therapies targeting both microbiomes. Non-antibiotic treatments, including nutritional and periodontal interventions, offer promising pathways. Understanding these microbiome dynamics is vital for improving outcomes in cirrhosis, especially amidst the rising tide of MDRO infections.
Katie Wright, EMJ
Reference
Lee S et al. Oral-gut microbiome interactions in advanced cirrhosis: characterisation of pathogenic enterotypes and salivatypes, virulence factors and antimicrobial resistance. J Hepatol. 2024;DOI:10.1016/j.jhep.2024.09.046.