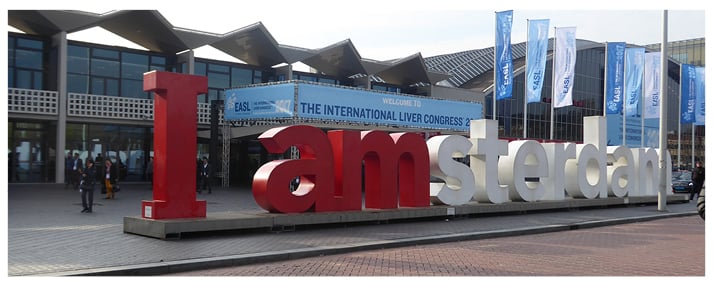
The diverse city of Amsterdam, Netherlands, hosted this year’s International Liver CongressTM (ILC) of the European Association for the Study of the Liver (EASL). Known as ‘the little Venice of the North’ the city boasts impressive architecture and a rich history, much of which can be viewed in its historic centre. Its quirky and lively atmosphere, with cycling routes throughout the city and beautiful canals, makes it the perfect place for the flagship event of the hepatology calendar.
The EASL aims to “promote liver research and improve the treatment of liver diseases worldwide” with its overall vision being: “Many Ways, One Aim: Beating Liver Disease.” As well as recognising the outstanding work of professionals in the field, the congress promoted public awareness about liver diseases, encouraged scientific research into the study of the liver, and endorsed state-of-the-art education for physicians and scientists. By hosting this annual event, the EASL hopes “to reduce the burden of liver disease in Europe by advocating for more research funding and effective prevention policies.”
This April’s 5-day spectacle certainly embodied the goals of the EASL as it brought industry experts and healthcare professionals from around the globe to showcase their expertise in the field of hepatology. This year hosted a plethora of fields surrounding hepatology including gastroenterology, internal medicine, cell biology, transplant surgery, infectious diseases, microbiology and virology, pharmacology, pathology and radiology, and imaging. The event attracted >10,000 delegates and 250 media representatives from 127 countries, making this a momentous occasion with opportunities to learn more about the latest surrounding liver research. The USA provided the greatest number of delegates, closely followed by the UK, Germany, ltaly, France, Spain, China, Netherlands, Belgium, and Switzerland. Among the 2,576 abstracts submitted this year, a total of 1,682 abstracts were accepted. There were 1,510 poster sessions, whilst the remaining 172 were oral sessions.
To honour some of the work in this field, the EASL presented three recognition awards to acknowledge those individuals who are making their mark in the field of hepatology and to thank them for their incredible efforts in advancing the study of the liver. Among these recognition awards was British paediatrician Giorgina Mielli-Vergani (UK), Gustav Paumgartner (Austria), who provided seminal work in polycystic liver disease, and Kenjiro Wake (Japan) for discovery of the Sternzellen in the liver. Now in its third year, the EASL Young Investigators Award category, which is dedicated to young investigators based on their commitment to international liver research and their achievements to date, went to Evaggelia Liaskou (UK) and Jean-Charles Nault (France) who also received a cash prize.
In the following pages, you will find a review of some of the fascinating updates this year’s congress had to offer, alongside some groundbreaking new research into the areas such as hepatitis, cirrhosis, and liver disease. We do hope this year’s congress review section will remind those who attended of some of the fascinating developments in the field that you were lucky enough to have witnessed. For those who did not attend, we hope this brings to light what you missed and truly excites you as you delve further into our journal.
Next year’s congress, which is sure to be even more fascinating and packed with the latest hepatology updates, will be hosted in April from the dates of 11th–15th April in the ‘City of Love’, Paris, France.
Potential Advance in Treatment for Paediatric Cholestatic Liver Disease
RESULTS of a study of a novel ileal bile acid transport inhibitor, known as A4250, were presented at this year’s ILC meeting and reported in an ILC press release dated 22nd April 2017. The inhibitor was shown to reduce the levels of blood (serum) bile acids in children who have cholestatic liver disease. Children can be vulnerable to diseases that either destroy or impair the development of the biliary tree, leading to other problems such as progressive liver injury, cirrhosis, and acid bile retention, which is related to pruritus. Patients and clinicians urgently need novel therapies to help manage pruritus and the increased levels of bile acid serum. A4250 has been demonstrated to reduce the elevated levels of bile serum acids in previous studies without any severe side effects.
Four patients received five doses of A4250 (0.01–0.2 mg/kg), and single doses were initially administered to individuals with intractable itching and cholestatic disease. The drug was administered in tablet form for 4 weeks. Therapy with rifampicin or ursodeoxycholic acid (UDCA) was also available throughout the study if needed. Nineteen individuals, aged between 1 and 17 years, were enrolled reporting itching by a visual itch score using patient data.
Results showed that pruritus improved in 14 of 19 cases and the mean level of serum bile acid was reduced. Seven out of nine individuals displayed considerable reductions in serum bile acid. There were no serious side effects of the drug, and few mild side effects could be related directly to the drug. A4250 blocks the ileal bile acid transporter in the last part of the small intestine, which consequently reduces the levels of bile acids in serum. Reabsorption of intestinal bile acids was inhibited;1 thus, they cannot be recirculated and secreted, making A4250 a highly effective inhibitor of the ileal bile acid transporter.
Prof Marco Marzioni, Clinic of Gastroenterology, Università Politecnica delle Marche “Ospedali Riuniti”, University Hospital of Ancona, Ancona, Italy, commented: “The study results are crucial as they address pruritus, a significant issue in chronic cholestatic diseases. Currently, there are few therapeutic options with limited efficacy, so new treatment strategies for pruritus are of great importance for clinical practice.”
References
- Baghdasaryan E et al. Inhibition of intestinal bile acid absorption improves chloestatic liver and bile duct injury in a mouse of sclerosing cholangitis. J Hepatol. 2016;63(3):674-81.
Norfloxacin Improves Prognosis of Patients with Child–Pugh C Cirrhosis
AN IMPROVEMENT in prognosis for patients with advanced liver disease has been demonstrated as a result of long-term orally administered antibiotic therapy in a multicentre, randomised controlled clinical trial. Norfloxacin administered for 6 months resulted in a reduced risk of infection and death at 6 months in patients diagnosed with Child–Pugh class C cirrhosis. The results of this study were reported in an ILC press release dated 20th April 2017.
“This study shows that long-term oral antibiotic therapy may improve the prognosis of patients with life-threatening liver disease. However, overuse of broad spectrum antibiotics is a subject that has been thoroughly debated over the years,” explained Dr Richard Moreau, Liver Unit, Beaujon Hospital, Clichy, France, the lead study author. He added: “The results from this study provide evidence that 6 months of norfloxacin therapy reduces the risk of infections and death in the short-term, but not in the long-term.”
The Child–Pugh classification scoring is used to evaluate and estimate the prognosis of patients with cirrhosis. Scoring ranges from A–C, with the most advanced cases falling within the C category. Decompensation of the liver, whereby the functioning of the liver is hindered due to extensive scarring, is seen in patients with Child–Pugh class C cirrhosis.
Patients diagnosed with Child–Pugh class C (N=291) were enrolled in to the Phase III study and received either a daily dose of 400 mg norfloxacin or placebo for a 6-month period. On completion of the 6-month treatment phase, it was noted that fewer patients had died in the norfloxacin subgroup compared to placebo (22 [15.3%] versus 36 [24.5%], respectively). Further comparison confirmed the number of patients who had received a liver transplant (norfloxacin [n=17] versus placebo [n=15]).
Patient follow-up was performed for an additional 6 months, subsequent to the 6-month treatment phase, to monitor infection, death, and additional liver-related complications. Cumulative mortality incidence was lower in the active norfloxacin subgroup than the placebo group (15.5% versus 24.8%, respectively). However, at 12-month follow-up the cumulative incidence of death was comparable across the two groups. Analysis also confirmed that at 6-month follow-up, patients who had been administered norfloxacin had developed fewer infections than those receiving placebo (30 [20.8%] versus 46 [31.3%], respectively).
Cognitive Impairment Improved by Faecal Microbiota
FAECAL transplantation of bacteria given from healthy individuals to those suffering from hepatic encephalopathy has been shown to improve cognitive function. The study, presented in an ILC press release dated 21st April 2017, explained that the number of hospitalisations that followed antibiotics and faecal transplantation was 2, compared to 11 in the standard of care arm (lactulose and rifaximin). A significant decline in hospitalisation for recurrent encephalopathy was reported. The treatment was well- tolerated with no serious side effects.
Dr Jasmohan Bajaj, Virginia Commonwealth University, Richmond, Virginia, USA, commented: “The results from this study demonstrate that in patients with hepatic encephalopathy, a faecal transplant improves brain function more than standard of care as well as reducing the number of hospital admissions, including those for recurrent hepatic encephalopathy. Faecal transplantation is an innovative and promising approach to treat this condition, and we look forward to more studies being conducted to confirm our results.”
Twenty men with cirrhosis and who had experienced recurrent episodes of hepatic encephalopathy were randomised to either broad spectrum antibiotics with a single faecal transplantation with a healthy donor and antibiotics for 5 days as well as standard of care treatment, or only rifaximin and lactulose. They were followed-up 150 days after they received treatment. In the faecal transplant group significant cognitive improvements were found on the Psychometric Hepatic Encephalopathy Score and the Stroop App. The results also showed that The Model for End Stage Liver Disease (MELD) score returned to baseline following the faecal transplant (delta -0.2; p=0.5), yet it increased after antibiotic treatment (delta 1.7; p<0.001). In addition, only 1 patient from the faecal transplant group demonstrated a decline in cognitive function, yet following the faecal transplantation returned to baseline.
Researchers Investigate New Ways to Accurately Predict Severe Liver Disease
OBESITY, high alcohol consumption, diabetes, lipid abnormalities, and insulin resistance were described as major contributors to the development of severe liver disease in an ILC press release dated 22nd April 2017. Diabetes was also stated to be the most significant predictor of severe liver disease for individuals who consume substantial amounts of alcohol daily (>140 g/week in women and >210 g/week in men).
Researchers examined which metabolic factors best predicted severe liver diseases whilst classifying the results based on the amount of alcohol consumed reported in the Finnish Health Study 2000, a nationally representative cohort. Waist circumference, total cholesterol, age, and ‘homeostatic model assessment’ (HOMA)-index were used to predict the development of liver disease in those who have no or mild alcohol consumption.
Lead author, Dr Fredrik Aberg, Transplantation and Liver Surgery Clinic, Helsinki University, Helsinki, Finland, commented: “The results of this study can help us identify which people are at risk of developing severe liver disease, so that we can work with them to reduce those risks.” He continued: “It is important that the risk factors identified in our study are considered for use in future risk models so that doctors can identify and counsel those patients at risk for developing liver disease.”
The study used individuals who were representative of the Finnish population and who had participated in the Health 2000 study, conducted between 2000 and 2001. A total of 6,732 individuals were included, all without known liver disease. The research collected follow-up data over the next decade of liver-related cancer, hospital admissions, and deaths.
Prof Philip Newsome, Centre for Liver Research, University of Birmingham, Birmingham, UK, added: “These data emphasise the important role of diabetes and metabolic syndrome in the development of liver disease, reinforcing the need to consider liver disease in such patient groups.”
High Animal-Protein Diet Increases Non-alcoholic Fatty Liver Disease Risk
AN EPIDEMIOLOGICAL study, reported in an ILC press release dated 21st April 2017, has demonstrated that an increased risk of non-alcoholic fatty liver disease (NAFLD) is associated with a diet high in animal protein, which is predominantly observed in overweight, elderly individuals.
NAFLD is an accumulation of fat within the liver, which can ultimately result in cirrhosis, an increased risk of cancer, cardiovascular disease, and kidney malfunction.1 NAFLD has a worldwide incidence of approximately 1 billion people.2 Early stages of NAFLD can be treated with changes to diet and lifestyle to aid weight-loss, however there is speculation, now more than ever, as new evidence emerges proposing that diet composition rather than increased calorie intake is fundamental factor in the development of NAFLD.
“A healthy lifestyle is the cornerstone of treatment in patients with NAFLD, but specific dietary recommendations are lacking,” explained lead study author, Dr Louise Alferink, Department of Gastroenterology and Hepatology, Erasmus Medical Centre, University Medical Centre, Rotterdam, Netherlands.
The study included 3,440 individuals; 30% were lean (BMI <25 kg/m2) and 70% were overweight (BMI of ≥25 kg/m2). The average age was 71 years and NAFLD was present in 35% of patients. The intake of macronutrients was monitored using a validated food-frequency questionnaire and data were analysed in quartiles using the nutrition density methodology. When considering the association between macronutrient intake and NAFLD, noteworthy findings were seen predominantly amongst overweight patients.
Initial results indicated that total protein was associated with increased likelihood of NAFLD (odds ratio [OR]: Q4 versus Q1 1.37; 95% confidence interval [CI]: 1.08–1.73, p=0.005). Furthermore, this association was primarily driven by animal protein (OR: Q4 versus Q1 1.50; 95% CI: 1.17–1.92; p=0.003).
Further consideration of metabolic factors resulted in the acceptance that it was animal protein, rather than total protein, that was mainly responsible for the development of NAFLD.
EASL Governing Board Member, Prof Philip Newsome, Centre for Liver Research, University of Birmingham, Birmingham, UK, commented: “This large population-based study indicates that increased dietary protein, in particular of animal origin, increases the likelihood of developing NAFLD and should be taken into account when counselling patients at risk of developing NAFLD.”
References
- NHS Choices. Non-alcoholic fatty liver disease (NAFLD). 2016. Available at: http://www.nhs.uk/conditions/fatty-liver-disease/Pages/Introduction.aspx. Last accessed: April 2017.
- European Association for the Study of the Liver. The Burden of Liver Disease in Europe. 2013. Available at: http://www.easl.eu/medias/EASLimg/Discover/EU/54ae845caec619f_file.pdf. Last accessed: April 2017.
SIRT Versus Sorafenib: A Dispute Between Overall Survival and Tolerance
PATIENTS with inoperable and locally advanced hepatocellular carcinoma (HCC) have been demonstrated to have a median overall survival score of 8.0 months when treated with selective internal radiation therapy (SIRT), compared to a median of 9.9 months when treated with sorafenib. Results from the SARAH trial, a randomised, open-label, controlled, multicentre investigator-initiated Phase III trial, were reported in an ILC press release dated 22nd April 2017.
The study included 459 individuals, 237 of whom received SIRT, from 25 French clinical centres. In the sorafenib and SIRT groups the median progression-free survival (PFS) was 3.7 months and 4.1 months, respectively (p=0.765). Furthermore, it was found that the cumulative incidence did not differ in either of the studies. In the SIRT group there were 1,297 treatment-related adverse events (AEs) with 230 of these Grade ≥3. In contrast, in the sorafenib group there were 2,837 treatment-related AEs and 411 of these were Grade ≥3. The Global Health Status scale of the EORTC QLQ-C30 questionnaire assessed quality of life, reporting that it was significantly better in patients who received SIRT over sorafenib (p=0.005).
Prof Valérie Vilgrain, Hôpital Beaujon Service de Radiologie, Paris, France, stated: “While SIRT demonstrated significantly reduced side effects, better quality of life, higher response rates, and more effectively controlled tumour progression in the liver, the overall survival of patients was not higher than in the sorafenib group. Nonetheless, this study provides evidence that SIRT may be a better-tolerated alternative for managing this complex and difficult-to-treat disease, deserving further evaluation.”
Prof Alejandro Forner, BCLC group, Liver Unit, Hospital Clinic, Barcelona, Spain and EASL Governing Board member, highlighted the importance of this study: “The SARAH trial is the first reported randomised controlled trial evaluating the survival benefit of SIRT in locally advanced HCC compared to sorafenib.” Prof Alejandro also explained that although SIRT was recognised as safe, it was not shown to have superior survival against sorafenib. Unfortunately, the study did not meet the primary endpoint, indicating that further trials are needed to ensure it can be a treatment option for patients.
Nivolumab: Acceptable Safety and Promising Efficacy Profiles for Sorafenib-Experienced Patients with Advanced Liver Cancer
NIVOLUMUB, an immune-oncology drug, has been shown to produce robust responses in addition to long-term survival rates for sorafenib-experienced patients with advanced liver cancer. Findings were consistent, irrespective of whether or not patients were infected with the hepatitis B or hepatitis C virus. The results were announced in an ILC press release dated 21st April 2017. Interim results from the dose expansion phase of the CheckMate 040 study demonstrated that the overall objective response rate (ORR) by blinded independent central review (BICR) was 14.5% and investigator assessment ORR was 19.3% for sorafenib-experienced patients. The safety profile of nivolumab was comparable to that of other tumour types.
Sorafenib is currently the only approved systemic treatment for hepatocellular carcinoma (HCC); if a patient is unable to tolerate this medication there is currently no effective treatment available.1 Nivolumab has already been shown to be an effective treatment option for other cancer types; however, it has not yet gained regulatory approval for HCC in the European Union (EU).
“The durable responses and survival rates that were achieved with nivolumab are very welcome, especially as the side effects were manageable,” said study author, Dr Bruno Sangro Gómez-Acebo, Hepatology Unit, Clínica Universidad de Navarra, Pamplona, Spain.
The Phase I/II study enrolled patients (N=145) with advanced HCC who were not suitable candidates for surgery. The trial was a multi-cohort, open label study investigating the use of intravenously administered nivolumab (3 mg/kg every 2 weeks). Treatment was maintained until either the cancer progressed, or adverse events became intolerable. The primary endpoint was determined by BICR ORR.
Cancer progression was observed in 91% of patients (n=132), with 8.3% (n=12) intolerant of nivolumab. Interim analysis data of the dose expansion study phase indicated a median follow-up time of 12.9 months. The median duration of response (DOR) has not so far been achieved, 8 out of 21 responders had a DOR of >12 months. The median overall survival was 16.7 months, and it was noted that this was not achieved in patients with chronic viral hepatitis B and C. Responses to nivolumab occurred regardless of tumour programmed death-1 (PD-1) ligand expression. Treatment-related adverse events (Grade 3/4) were seen in 16.6% of patients.
Nivolumab works by acting as a programmed-death-1 (PD-1) immune checkpoint inhibitor, which can restore T-cell-mediated anti-tumour activity, enabling the body to fight against the cancer cells.
References
- European Association for the Study of the Liver (EASL), European Organisation for Research and Treatment of Cancer (EORTC). Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2012;56(4):908-43.
Human Albumin Improves Survival of Patients with Decompensated Cirrhosis
SURVIVAL rates increased in patients with decompensated cirrhosis who had long-term administration of human albumin, as presented from the ANSWER study in an ILC press release dated 22nd April 2017. Management of ascites and quality of life were improved by human albumin treatment; additionally, the number of severe complications and hospitalisations were reduced.
Prof Mauro Bernardi, University of Bologna, Bologna, Italy, stated: “There has been a lack of scientific evidence proving that long-term human albumin can treat cirrhosis with ascites.” Prof Mauro continued: “The ANSWER study has now clarified this issue, showing that human albumin extends survival and helps better manage ascites, as well as reducing the incidence of severe complications of this very serious disease.”
The ANSWER study used a control trial of 440 randomised participants with cirrhosis and uncomplicated ascites, comparing standard diuretic therapy with human albumin (requiring 40 g intravenously twice a week for the first 2 weeks, followed by once a week) to standard diuretic therapy. All the participants were followed up 18 months after the study.
The results showed that patients who received standard therapy and human albumin had a significantly higher survival rate than those who received standard therapy alone. The patients who received standard therapy and human albumin had a 38% reduction in their risk of death. Quality of life, management of ascites, hospital admission, and complications of cirrhosis were demonstrated to have significant benefits for patients administered human albumin. Overall survival was the primary endpoint.
Prof Annalisa Berzigotti, University Clinic for Visceral Surgery and Medicine, University of Bern, Bern, Switzerland, and EASL Governing Board Member said: “The reduction in mortality observed in the albumin-treated arm of this randomised controlled study is a novel and important piece of information. Based on these data, weekly administration of albumin should be considered in patients with cirrhosis and ascites to prevent life- threatening complications.”
Association Between Climate and Cirrhosis
A RECENT study has revealed an intriguing association between climatic and geographical factors and rates of alcoholic cirrhosis according to the results of a study reported in an ILC press release dated 22nd April 2017. The study’s lead author, Dr Neil Shah, Division of Gastroenterology and Hepatology, Department of Medicine, University of North Carolina School of Medicine, Chapel Hill, North Carolina, USA, explained: “Our research reveals that a country’s climate and geographical location have a startling influence on the burden of liver cirrhosis.”
It was hypothesised that geographical location would influence alcohol consumption, thus influencing rates of alcoholic cirrhosis. For instance, it was suggested that individuals might increase alcohol intake in order to deal with cold and dark conditions. As the first stage in investigating this hypothesis, researchers collated and analysed a range of data across 193 countries taken from World Health Organization (WHO) and World Meteorological Organization (WMO) databases.
The results of the univariate analysis revealed an inverse association between mean average temperature and mean annual sunshine hours with the alcohol attributable factor (AAF) of cirrhosis; additionally, there was a positive association with absolute latitude (p<0.05) and the AAF of cirrhosis. After adjusting for the percentage of binge drinkers among active drinkers and alcohol consumption, it was found that average temperature and sunshine hours were still independently associated with the burden of alcohol-attributable liver cirrhosis. According to the data, a 1°C temperature increase was linked with a 0.3% decrease in the AAF of cirrhosis.
A significant amount of further research needs to be carried out based on this initial finding. Firstly, the correlation of these factors does not necessarily imply causality so further testing of this hypothesis should be carried out. Additionally, there is a vast range of other factors, such as culture and religion, that may influence this association. The design of geographically specific healthcare policies that consider climatic variables will doubtlessly prove to be highly debated and require a lot of supporting evidence.
Severe Periodontitis Associated with Mortality in Cirrhosis
SEVERE periodontitis was found to be a strong predictor of mortality in patients with cirrhosis in a recent study. The prediction held true after adjustments were made for a number of risk factors. The results of this prospective study were reported in an ILC press release dated 20th April 2017.
Currently, periodontitis is prevalent amongst adults: 10–15% have a severe form of the disease and >35% have periodontitis. Furthermore, periodontitis is found frequently in patients with cirrhosis and previous research has implied that periodontitis is linked to the progression of liver diseases.
Researchers followed-up 184 consecutively enrolled patients with cirrhosis for an average of 1 year and assessed their oral health. At the beginning of the study, 44% of the patients were found to have severe periodontitis, as assessed by standard periodontology criteria. Over the follow-up period, almost half of the patients in the study died; the primary cause of death was complications of cirrhosis. Analyses were carried out on the association of periodontitis with mortality after adjustments were made for present alcohol use, smoking status, sex, age, comorbidity, Child–Pugh score, Model of End-Stage Liver Disease (MELD) score, cirrhosis aetiology, and nutritional risk score. The analyses revealed an association between severe periodontitis and greater all-cause mortality.
Lead study author Dr Lea Ladegaard Grønkjaer, Aarhus University Hospital, Aarhus, Denmark, spoke about the possible mechanism behind this finding, and explained that: “Periodontitis may act as a persistent source of oral bacterial translocation, causing inflammation and increasing cirrhosis complications. As it can be treated successfully, however, we hope that our findings motivate more trials on this subject.”
With an association between gum disease and increased mortality having been demonstrated, the next research direction is to investigate whether improvements in gum care will result in improved outcomes in patients with liver cirrhosis.
Successful Results of Trial of Fibrate Therapy in Primary Biliary Cholangitis Patients
PRIMARY biliary cholangitis (PBC) patients who have an inadequate response to treatment with ursodeoxycholic acid (UDCA) can demonstrate significant improvements to their condition through fibrate therapy, according to the results of a study presented at this year’s ILC meeting and reported in an ILC press release dated 22nd April 2017.
Many PBC patients respond well to the administration of UDCA, with disease progression slowed and improved liver function tests often taking place. However, >30% of patients do not respond adequately to UDCA and remain at a high risk of disease progression, which could lead to lower survival rates and the need for a liver transplant. A study was therefore undertaken to test a new treatment method for such patients.
The BEZURSO study was a randomised, double-blind, placebo-controlled trial of bezafibrate in combination with UDCA in 100 patients who had an inadequate biochemical response to UDCA, as defined by the Paris-2 criteria. The patients were randomised to either 400 mg/day of bezafibrate or placebo in addition to UDCA for 2 years. The results showed that the primary endpoint of normalisation of liver function tests was met in 15 (30%) of the patients, compared with no patients in the placebo group.
Additionally, alkaline phosphatase normalisation was achieved in 67% of patients in the bezafibrate group as opposed to no patients in the placebo group. There were also significant reductions in surrogate markers of liver disease (liver stiffness and ELF score, which are predictors of liver failure and mortality) and fatigue and itching in the bezafibrate group compared to the placebo group. Rates of serious adverse events and end-stage liver complications were the same across both groups.
Dr Christophe Corpechot, Head, Reference Center for Inflammatory Biliary Diseases, Paris, France, and lead author of the study commented: “The study provides evidence supporting the use of a combination of fibrates and UDCA in this population, with normalisation of liver function tests, improved symptoms, and prevention of liver disease progression.”
New Research Avenue for Fatigue in Primary Biliary Cholangitis
STUDY of fatigue in the rare disease primary biliary cholangitis (PBC) has begun, with results of the first randomised, controlled, double-blind trial being reported at this year’s ILC Congress, according to an ILC press release dated 20th April 2017.
PBC is a rare, chronic, autoimmune disease that can damage bile ducts, often leading to cirrhosis, liver failure, or cancer. Symptoms such as pruritus and fatigue can cause a very low quality of life for sufferers; roughly 25% of patients’ work and social lives are detrimentally affected by fatigue, a symptom which does not correlate to disease severity. The RITPBC study examined whether rituximab could reduce the severity of fatigue symptoms in PBC patients, as well as assessing the safety and tolerability of rituximab, and the sustainability of the positive effects of the drug. The improvement of fatigue domain score of the PBC-40, a disease-specific quality of life questionnaire, at 12 weeks was the primary objective of the trial.
The team randomised 57 PBC patients with moderate-to-severe fatigue to receive two doses of rituximab or placebo on Days 1 and 15, with follow-up of ≤12 months. No statistically significant difference was noted in fatigue score between the two arms of the study, but an improvement in fatigue for patients in both groups from the beginning of the study was reported. The rituximab arm also showed improved anaerobic threshold compared with placebo. Four serious adverse events were reported in the trial: one death before the drug was started and three events in the placebo arm.
Prof Marco Marzioni, Clinic of Gastroenterology, Università Politecnica delle Marche “Ospedali Riuniti”, University Hospital of Ancona, Ancona, Italy, commented: “The current trial shows that although rituximab was not effective in reducing fatigue, there is nevertheless still a connection between the symptom and the immunopathological process. Therefore, further characterisation of the type of fatigue experienced by PBC patients may be crucial in helping identify optimal treatment.”

Risk Factors for Paediatric Liver Disease Confirmed
CHILDHOOD infection of hepatitis C virus (HCV) has been linked to serious long-term liver disease in a recent study reported in an ILC press release dated 20th April 2017. The study found that >33% of young people age <18 who had HCV went on to develop liver problems, including 5% developing liver cancer and >4% eventually receiving a liver transplant.
The study, from a group of researchers at Birmingham Children’s Hospital, Birmingham, UK, considered data from patients who were estimated to have contracted HCV infection when they were <18 years of age taken from the HCV Research UK database. The data were collected between July 2012 and October 2016 from 51 adult and 7 paediatric centres, with a total of 1,014 patients, of whom 72% were male. The team found that intravenous drug abuse was the predominant cause of infection (n=535), followed by blood products (n=224), and acquisition at birth (n=116). Genotype 1 was the most common type of infection (57% of patients) but 35% had genotype 3, the most difficult strain to cure.
In the cohort, liver disease was present in 354 patients (33%) and 269 patients had cirrhosis (27%); 55 had hepatocellular carcinoma (5%), with 47 (5%) having received a liver transplant. Patients who contracted HCV at birth were shown to have developed cirrhosis at a younger age than those who contracted it from intravenous drug use (median 36 years versus 48 years, respectively).
It is hoped that by defining those most at risk of liver disease, more could be done to detect and treat the diseases amongst the most vulnerable groups. First author Dr Lin Modin, Birmingham Children’s Hospital, commented: “Our study showed that more than one-third of young people infected with HCV in childhood have serious long-term liver disease. Detection of HCV should be aimed at relevant risk groups, particularly young intravenous drug abusers.”
Improved Patient Reported Outcomes for Direct-Acting Antiviral Treatment Combination Therapy
HEPATITIS C virus (HCV) and cirrhosis patients experience greater improvement of patient-reported outcome (PRO) scores in comparison to patients without cirrhosis when treated with the direct-acting antiviral (DAA) combination sofosbuvir (SOF) and velpatasvir (VEL), with or without voxilaprevir (VOX), according to an analysis presented at ILC 2017.
This treatment combination, already shown to be safe and effective against all HCV genotypes in different populations, showed significant improvements in PROs, particularly regarding cirrhosis patients, following achievement of sustained virologic response at 12 weeks (SVR12).
The study analysed information from 1,908 chronic HCV patients enrolled in the POLARIS 1, 2, 3, and 4 studies, which assessed the efficacy and safety of SOF/VEL/VOX in treating HCV infected patients. Questionnaires ascertained outcomes from 26 PRO domain scores, relating to quality of life, fatigue, work productivity, and activity impairment in these patients. The results showed that in patients with and without cirrhosis in both the SOF/VEL/VOX and SOF/VEL treatment groups, the overall cure rate (SVR12) was 94%. Following successful treatment, cirrhosis patients gained major improvements in their PRO scores compared to when treatment began. These were similar to or greater than patients without cirrhosis. No PRO improvements were seen in those cirrhosis patients treated with placebo.
“This analysis showed that although patients with HCV and cirrhosis have significantly impaired PROs, they experience the greatest improvement during treatment with SOF/VEL with or without VOX, when compared to those without cirrhosis,” explained Dr Zobair Younossi, Center for Liver Diseases, Washington DC, Washington, USA, lead author of the study, in an ILC press release dated 20th April 2017. “We also found that achieving a SVR with the drugs was associated with substantial gains in outcomes.”
The improvements seen in PROs of HCV-related cirrhosis patients from this particular DAA therapy are likely to impact the significant indirect, as well as direct costs linked to HCV-related cirrhosis in the future.
Optimism for Treatment of Challenging Hepatitis C Virus Subgroup
ENDURANCE-3, a Phase III, open-label, active-controlled study, has demonstrated a 95% sustained virologic response rate at 12 weeks post-treatment (SVR12) for patients being treated for hepatitis C virus (HCV). The study assessed the oral, once-daily treatment regimen of glecaprevir/pibrentasvir (G/P) in comparison to the more common treatment of sofosbuvir and daclatasvir against the most challenging subgroup of HCV patients: genotype 3.
For the study, 348 treatment-naïve, non-cirrhotic HCV genotype 3 patients were randomised to receive a daily dose of G/P for 12 weeks or sofosbuvir and daclatasvir. Thereafter, 157 patients were given G/P for 8 weeks. The percentage of patients who achieved SVR12 was the primary endpoint, and this was achieved by 95% of patients who received G/P for 12 weeks (222/233; 95% confidence interval [CI]: 93–98) and 97% of patients who received sofosbuvir and daclatasvir for 12 weeks (111/115; 95% CI: 91–99). In both groups, 1% of patients relapsed. Of the cohort who received G/P for 8 weeks, 95% achieved SVR12 (149/157; 95% CI: 92–98) and 3% relapsed. Adverse events were reported to be mostly mild (71%), and no treatment-related adverse events were serious.
Lead author of the study Dr Graham Foster, Queen Mary University of London, London, UK, explained: “While there has been great progress made in the treatment of patients with hepatitis C, there remain limited options for those with genotype 3 disease. As such, we are pleased to see that the investigational combination of G/P achieved high SVR12 rates in treatment-naïve, non-cirrhotic patients.” He added: “Treatment with this once-daily regimen for 8 weeks could provide a highly efficacious and well-tolerated option for treatment-naïve, non-cirrhotic patients with hepatitis C, genotype 3, if approved by the regulatory authorities.”
Treatment Regimen May Offer Cure for Hepatitis C-Infected Children
CHILDREN infected with hepatitis C virus (HCV) can be cured of the condition through the use of direct-acting antiviral (DAA) treatment, according to the results of a study presented in an ILC press release dated 21st April 2017. The study analysed an investigational dosage of once-daily ledipasvir 45 mg/sofosbuvir 200 mg (LDV/SOF) in a cohort of 6–11 year olds.
Unlike adults with HCV, who are regularly treated with DAAs, children with the condition mainly receive 24–48 weeks of pegylated interferon plus ribavirin (RBV), a treatment which can cause severe side effects.
For this ongoing, open-label study, 90 children aged between 6 and 11 years with chronic HCV were enrolled. HCV genotype 1 infected children who received either 12 weeks (n=85) or 24 weeks of LDV/SOF treatment (n=1) if they had cirrhosis and failed previous pegylated interferon plus RBV treatment. Genotype 3 patients received 24 weeks of LDV/SOF plus RBV (n=2) and genotype 4 patients were given LDV/SOF for 12 weeks (n=2). Most of the children in the group were white, male, treatment-naïve, and vertically infected.
Following completion of 12 weeks of treatment, 99% (n=89/90) of the group had undetectable levels of HCV/RNA. There was only one case of relapse: a genotype 1, treatment-naïve patient with cirrhosis. There were no instances of severe or life-threatening adverse events, and no children discontinued the study due to side effects. The most common side effects reported in 10% of patients were headache, fever, and abdominal pain.
“DAAs have transformed the treatment of adults with chronic HCV, however, studies of these new therapies in children are required,” stated Dr Karen Murray, University of Washington School of Medicine and Seattle Children’s Hospital, Seattle, Washington, USA. “These data establish the use of the oral DAAs as an important treatment option in HCV-infected children aged 6–11 years old.”
Higher Levels of Hepatitis E in Germany Than Previously Recorded
THE FREQUENCY of hepatitis E virus (HEV) RNA was found to be higher in Germany than had been reported in the past, according to the results of a study reported on in an ILC press release dated 21st April 2017. These findings add support to calls for screening for HEV RNA at blood donation centres, which is currently non-compulsory.
The study authors used a HEV polymerase chain reaction (PCR) assay to screen pools of 24 donations; reactive pools were then individually examined to detect HEV RNA positive donations. Overall, 13,441 blood donations at the University Hospital Hamburg-Eppendorf, Hamburg, Germany, were tested and 15 (0.11%) were found to be HEV RNA positive. One of these 15 positive donors presented with acute self-limiting hepatitis, and the remaining 14 were healthy and asymptomatic. One of the asymptomatic patients had donated blood products that had been transfused into nine immunocompromised patients prior to this screening. One of these nine patients had detectable serum HEV RNA before their death, which was caused by acute-on-chronic liver failure complicated by pseudomonas sepsis.
These findings are pertinent as they lend weight to the argument that HEV RNA should be screened for at blood donation centres.
HEV infection is often asymptomatic, so blood donors may not realise they are infected; thus, HEV RNA positive blood may be transfused into patients, as indeed is what occurred in this study. Lead study author Dr Dirk Westhölter, University Hospital Hamburg-Eppendorf, Hamburg, Germany, spoke about this concern and the need for further research, and stated: “Since HEV infection can have serious consequences among the immunocompromised and a single positive donor can give rise to HEV infection in several other patients, there is a need for longer term studies to analyse the effectiveness of routine HEV blood donor screening, and to determine whether this process should be implemented at blood clinics everywhere.”
Sustained Removal from Liver Transplant List After Hepatitis C Treatment
PATIENTS who had been taken off the liver transplant list after undergoing successful direct-acting antiviral (DAA) therapy for chronic hepatitis C virus (HCV) and severe liver damage were found to have a favourable outcome >1 year later. The results from this study were reported in an ILC press release dated 21st April 2017. Today, chronic HCV is the most common reason for liver transplantation in adults. With >8,500 patients in Europe on the waiting list for a liver transplant, this number only expected to increase. Studies such as this one, tracking the outcomes of those removed from the transplant list are of great importance. Lead study author, Dr Luca Belli, Gastroenterology and Hepatology Liver Unit, Niguarda Hospital, Milan, Italy, announced that: “The results of this study are very encouraging with clinical improvement due to DAA therapy lasting over a year in nearly all patients.”
In this retrospective study, the authors tracked 38 patients who were treated with DAA therapy for decompensated cirrhosis without liver cancer and, following clinical improvement, were taken off the liver transplant list. After a median follow-up time of 15 months from being taken off the list, 37 patients were still alive and 1 of these patients had been relisted for clinical re-decompensation. The patient who died did so due to rapidly progressing hepatocellular carcinoma. Results showed that median Model of End-Stage Liver Disease (MELD) scores were 9, 78 weeks since the start of DAA therapy, which was an improvement from 14 at the start of therapy; furthermore, median Child–Pugh scores improved from 9 at the beginning of therapy to 6 after 78 weeks.
Dr Belli spoke about the need for further study, stating: “We still need to follow these patients for much longer to confirm the results and assess the long-term risks of deterioration, but so far the risk of dying after delisting is much lower than that of dying after receiving a liver transplant.”
New Clinical Practice Guidelines Unveiled for Liver Disease Management
FOUR Clinical Practice Guidelines (CPGs) were unveiled at this year’s ILC Congress, designed to support healthcare professionals’ clinical decision-making across a number of specific liver diseases. The announcement was initially made in an official ILC press release issued on 19th April 2017. Each individual guideline was also presented in detail during the event.
Broadly, CPGs are used to assist the decision-making processes related to a specific clinical circumstance and can be useful to a varied audience, including; physicians, health service providers, patients, and caregivers. In this instance, these four CPGs have been developed to outline best practice advice for the management of patients with certain liver diseases.
The recently announced CPGs included the revision of one existing guideline on the ‘Management of Hepatitis B virus infection’ and the publication of an additional three original guidelines, including:
- Management of Acute (fulminant) Liver Failure
- Role of endoscopy in Primary Sclerosing Cholangitis (PSC)
- The treatment and management of patients with Primary Biliary Cholangitis
Specific focus was placed on the European Society for Gynaecological Endoscopy/European Association for the Study of the Liver (ESGE/EASL) guideline on the role of endoscopy in PSC.
“The EASL Primary Biliary Cholangitis guidelines are meant to support clinicians in establishing a long-term commitment with patients and their disease, providing indications on how to stratify the risk from diagnosis to disease progression. The guidelines will also help identify which patients require second-line treatment, in which advances are fortunately being made,” explained Prof Marco Marzioni, Clinic of Gastroenterology, Università Politecnica delle Marche “Ospedali Riuniti”, University Hospital of Ancona, Ancona, Italy.
Prof Marzioni, who was involved in writing the guideline, added: “The EASL-ESGE guidelines have been developed by the two societies to identify the optimal approach for the management of PSC. As extra-hepatic bile ducts are involved in the disease, a multidisciplinary approach is a key factor for the success of management. The guidelines provide a tool to fine tune the endoscopic and medical treatments of patients with PSC.”








