BACKGROUND AND AIMS
The Barcelona Clinic Liver Cancer (BCLC) classification is the reference system to stage and prognosticate hepatocellular carcinoma (HCC). The NIACE score1 (tumour nodularity, infiltrative nature of the tumour, serum alpha-fetoprotein level, Child–Pugh score, and ECOG [The Eastern Cooperative Oncology Group] performance status) uniquely considers tumour characteristics but is yet to be validated in an Australian context. It is suggested that the NIACE score may offer prognostic clarity within BCLC classes, which encompass heterogenous tumours matched with single management options. The aim of this study was to compare the survival prognostic value of the NIACE score within the BCLC staging system.
METHODS
Data for this study was retrospectively analysed from a cohort of 2,202 patients with HCC collected across six metropolitan hospitals in Victoria, Australia, from January 2000–August 2018. Patients were included in the study if all markers were available to calculate prognostic scores, including tumour nodularity (0 if <3, 1 if ≥3), tumour infiltration (0 if no, 1.5 if yes), serum alpha-fetoprotein (0 if <200, 1.5 if ≥200 ng/mL), Child–Pugh score (0 if A, 1.5 if B), and ECOG status (0 if 0, 1.5 if ≥1). Baseline characteristics including age, sex, country of birth, ethnicity, aetiology of chronic liver disease, and the presence of cirrhosis were recorded. Survival time was measured from the date of diagnosis todate of death (or censored at last follow-up). Transplant-free survival (TFS) was used as the endpoint for analysis.
RESULTS
A total of 366 patients (86% male, 14% female; median age at diagnosis was 63±12 years; 103 [28.1%] Australian born) were included in the analysis. Aetiology of liver disease was hepatitis B virus (64 [17.4%]), hepatitis C virus (157 [42.8%]), alcohol-associated (143 [39.0%]), and other (108 [29.4%]). The mean serum alpha-fetoprotein level for the cohort was 7,839 ng/mL. Over a median follow-up time of 16 months, 185 patients (50.4%) were found to be deceased. The median TFS for BCLC 0 (n=21), A (n=108), B (n=82), C (n=113), and D (n=39) were 64, 29, 24, 12, and 4 months, respectively (p<0.001). The TFS for NIACE score <2.5 (n=169) versus ≥2.5 (n=197) was 34±3 months versus 12±2 months, respectively (p<0.001). Furthermore, NIACE had prognostic value within BCLC subclasses, with the TFS of patients within BCLC-A (36±7 months versus 20±3 months; p<0.01) and BCLC-B (31±7 months versus 19±4 months; p<0.005) being significantly different for scores of <2.5 versus ≥2.5, respectively (Figure 1).
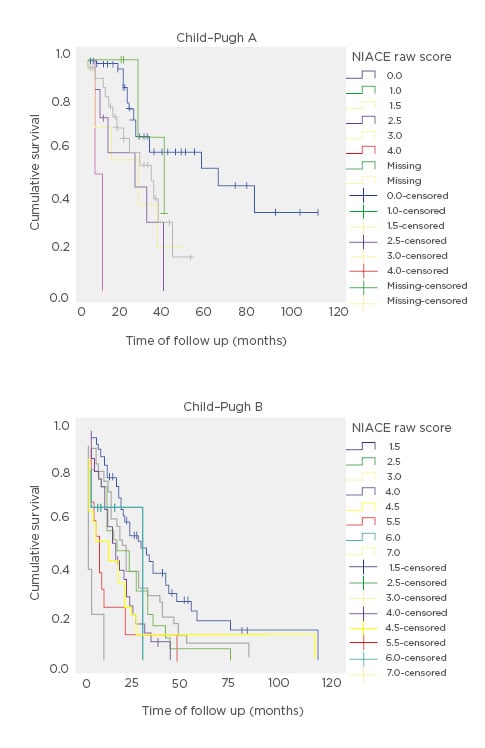
Figure 1: Kaplan–Meier curves showing survival of Child–Pugh A and B hepatocellular carcinoma patients by NIACE raw score.
There was no significant discriminating ability amongst later stage BCLC-C or BCLC-D.
CONCLUSION
Accurate prognostication in HCC is of vital importance to allow for appropriate care planning and optimisation of treatment options. The NIACE score is an easy-to-calculate prognostic score, and this study demonstrated that NIACE can distinguish between two subgroups with different prognosis within early (BCLC-A) and intermediate (BCLC-B) stage HCC. The broader implications of these findings are that they may assist clinicians in improving the accuracy of survival prognostication, thereby helping to define subgroups of patients who may benefit from an intensified treatment strategy. This is the first validation of the score in an Australian population. Further prospective validation of the NIACE score in HCC patients and comparison with other simple scores, such as Albumin-Bilirubin grade, is warranted to confirm its prognostic value and use in guiding decision making in conjunction with the BCLC staging system.








