Paracetamol, or acetaminophen, is the most commonly used drug in Western countries. Use of the drug is markedly commonplace because it can be obtained without a prescription. A recent nationwide study (SALT III) showed that paracetamol-induced acute liver failure is increasing and is the main cause of acute liver failure leading to registration for liver transplantation (42.1%, including 17.6% of paracetamol misuse).1 The study aimed to assess the knowledge of prescribers (practitioners and residents), care and drug providers (including nurses and pharmacists), and students regarding paracetamol use in the University Medical Centre, Montpellier School of Medicine, Montpellier, France.
This prospective study was performed using a questionnaire comprising five questions regarding paracetamol prescription in adult patients:
What is the primary cause of liver failure in France?
What is the maximal daily dose of paracetamol for chronic usage?
What is the maximal unitary dose of paracetamol?
What is the minimal time interval between two doses?
What are the promoting factors of paracetamol hepatotoxicity?
The questionnaire has been validated by the Committee for the Security of Medication Use (COSEMED) of the hospital and submitted from November 2017–October 2018 during professional meetings or via the hospital intranet website.
During this 1-year period, 1,118 questionnaires were completed by various care providers: medical practitioners (n=130; 12%), nurses (n=408; 36%), students (n=101; 9%), residents (n=201; 18%), and pharmacists (n=30; 3%). The overall rate of correct answers ranged from 54.6% for students to 73.7% for pharmacists. The answers were excellent regarding the maximum unit dose (95.1–99.4% for care workers and 84.5% for students) and the interval between doses (93.0–98.2% for care workers and 83.5% for students). Regarding the role of paracetamol in liver failure, the answers were good (60.4–82.6% for care workers and 66.1% for students). In contrast, the answers were poorer concerning the maximum daily chronic dose (14.4–50.1% for care workers and 10.1% for students), with some answers of 6 g per day. The identification of cofactors of hepatotoxicity was variable: good for chronic alcoholism, but low for undernutrition or antalgic co-medications (Figure 1).
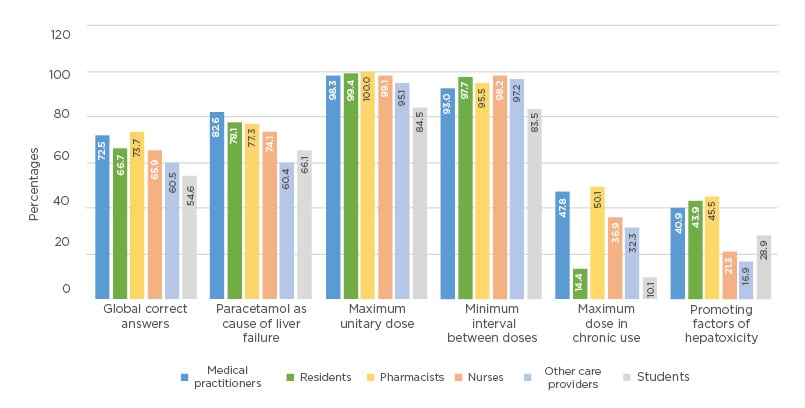
Figure 1: Distribution of answers by interviewed care providers.
The knowledge regarding the proper use of paracetamol is insufficient for the maximum chronic dosage, the risk of paracetamol hepatotoxicity, and its contributing factors. These results encourage the promotion of a more intensive and specific teaching of all care providers involved in the use of this drug.








