INTRODUCTION
Treatment of alcoholic hepatitis with corticosteroids remains controversial, with recent studies indicating only a 28-day survival benefit.1 The neutrophil-to-lymphocyte ratio (NLR) may reflect the systemic inflammatory response, and the authors have previously shown that the NLR can affect the outcome of corticosteroid response in alcoholic hepatitis patients.2 These abstracts aimed to determine the associations of baseline NLR with acute kidney injury (AKI), infection, and Lille response, as well as to externally validate the NLR as a means of identifying patients for corticosteroid therapy.
A) BASELINE NEUTROPHIL-TO-LYMPHOCYTE RATIO INDICATES BOTH PREVALENT AND INCIDENT INFECTION AND ACUTE KIDNEY INJURY, AND PREDICTS LILLE CORTICOSTEROID RESPONSE IN ALCOHOLIC HEPATITIS
The NLR was calculated from 789 patients who participated in the STOPAH trial, with patients randomised to receiving or not receiving prednisolone. Prevalent AKI was defined by an initial creatinine level ≥133.0 μmol/L and incident AKI was defined as either an increase of serum creatinine by 26.5 µmol/L or by 50% by Day 7 in those without baseline AKI. Patients presenting with infections (prevalent infection) were treated prior to randomisation; incident infections were determined after inclusion in the trial.
Those with prevalent AKI had a higher NLR than those without (11.1 versus 6.0; p=0.001; 95% confidence interval [CI]: 2.6–7.6), as did those with prevalent infection compared to those without (7.8 versus 6.3; p=0.02; 95% CI: 0.2–2.8).
A favourable Lille score with prednisolone treatment was more likely if NLR ≥5 versus <5 (56.5% versus 41.1%: p=0.01; overall response [OR]: 1.86; 95% CI: 1.16–2.99). The risk of developing infection after prednisolone treatment was greater if NLR >8 versus <8 after 7 days (17.3% versus 7.4%: p=0.006; OR: 2.60; 95% CI: 1.32–5.14) and 28 days (30.6% versus 20.0%: p=0.031; OR: 1.76; 95% CI: 1.05–2.96). The risk of incident AKI after prednisolone treatment was greater for those with NLR >8 versus <8 (20.8% versus 7.0%: p=0.008; OR: 3.46; 95% CI: 1.39–8.62).
The finding reaffirmed previous observations that prednisolone does not improve outcomes for those with NLR <5 or >8 but does improve outcome beyond 28 days for those with NLR 5–8 (Table 1).
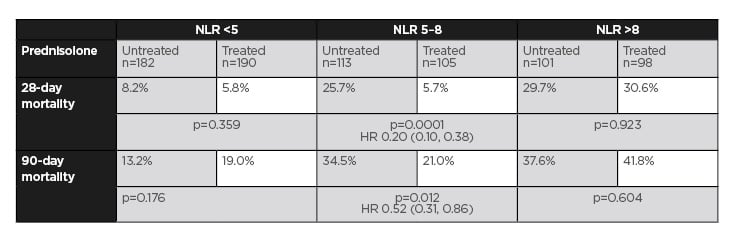
Table 1: Mortality relative to neutrophil-to-lymphocyte ratio category and prednisolone treatment in all patients.
HR: hazard ratio; NLR: neutrophil-to-lymphocyte ratio.
This may be explained by the greater likelihood of achieving a Lille response if NLR <5, but only achieving a reduction in AKI and infection if NLR ≤8.
B) A MODIFIED GLASGOW ALCOHOLIC HEPATITIS SCORE INCORPORATING THE NEUTROPHIL-TO-LYMPHOCYTE RATIO IS SUPERIOR TO OTHER BASELINE SCORES OF PROGNOSIS IN ALCOHOLIC HEPATITIS
In the same cohort of patients, there was a strong correlation between the total white blood cell count (WCC) and NLR: r=0.564; 95% CI: 0.52–0.60; p<0.0001. In view of this, the NLR was incorporated into the Glasgow Alcoholic Hepatitis Score (GAHS)3 with an NLR threshold of 5 replacing the total WCC threshold of 15, creating a modified GAHS (mGAHS). The areas under the curve for mGAHS for 28-day and 90-day outcomes were 0.783 (95% CI: 0.752–0.812) and 0.739 (95% CI: 0.706–0.770), respectively. For 28-day outcome, the mGAHS area under the curve was superior to that of the Maddrey’s discriminant function (0.684: p<0.0001; 95% CI: 0.05–0.14), the original GAHS (0.763: p=0.027; 95% CI: 0.002–0.040), and the model for end-stage liver disease (0.739: p=0.0014; 95% CI: 0.009–0.080).
C) VALIDATION OF THE PRE-TREATMENT NEUTROPHIL-TO-LYMPHOCYTE RATIO TO PREDICT RESPONSE TO CORTICOSTEROIDS IN SEVERE ALCOHOLIC HEPATITIS
The observations from the previous abstract were then tested in an independent validation group of 237 patients. Again, no improvement in outcome with corticosteroids was seen at either 28 days or 90 days for NLR <5 (28-day mortality 10.0% versus 5.1%; p=0.416; 90-day mortality 16.3% versus 18.4% p=0.843) or NLR >8 (28-day mortality 23.5% versus 28.0%; p=0.469; 90-day mortality 39.2% versus 48.0%; p=0.362). In total, 28-day mortality for NLR 5–8 was reduced by corticosteroid treatment (2.7% versus 28.6%; p=0.0023) with a trend to reduced mortality at Day 90: 21.6% versus 37.4%; p=0.097. Those with a mGAHS ≥9 and NLR 5–8 had a significant reduction in 90-day mortality with prednisolone treatment: 23.3% versus 46.4%; p=0.036; hazard ratio: 0.268; 95% CI: 0.10–0.71.
CONCLUSIONS
These abstracts indicate the association of NLR with risk of infection and AKI in alcoholic hepatitis, as well as the chance of a Lille response to alcoholic hepatitis. Incorporation of the NLR in place of WCC improves prognostic accuracy. These results reaffirm and externally validate the observation that corticosteroid treatment for those with NLR <5 or >8 is ineffective but improves outcomes for those with NLR 5–8 beyond 28 days.








