BACKGROUND AND AIMS
The gut microbiome might affect the severity of metabolic dysfunction-associated steatotic liver disease (MASLD);1-3 however, data regarding their association in Asian populations is limited. The authors analysed the differences in the gut microbial composition of Thai patients with MASLD, according to the severity of liver fibrosis assessed by MRI.
METHOD
This cross-sectional study included 156 patients with MASLD (51% male, mean age: 56±10 years). Liver steatosis grades ≥1 were identified by MR-proton density fat fraction ≥5.2%. Based on MR-elastography (MRE) at the cut-off of 2.97 kPa, there were 131 patients with mild fibrosis (F01) and 25 patients with significant fibrosis (F234). The single nucleotide polymorphisms of PNPLA3, TM6SF2, and HSD17B13 were assessed by allelic discrimination assays. Faecal specimens were sequenced targeting the V4 region of the 16S rRNA gene and analysed using the nf-core ampliseq bioinformatics pipeline. Differential analysis of individual taxa between two groups was conducted through linear discriminant analysis effect size (LEFSe), employing a cut-off of LEFSe >2 and a significance level of p<0.05.
RESULTS
There was no significant difference in alpha-diversities (Chao1, Shannon, and Simpson indices) between patients with F01 and F234. However, the beta diversity significantly differed between the two groups (p=0.012). High abundances of Fusobacterium and Escherichia-Shigella, pathogenic bacteria, contributing to the inflammatory process and carcinogenesis, were significantly detected in the faecal samples of patients with F234 compared to those in the F01 group (odds ratio: 3.31; 95% CI: 1.30–8.42; p=0.012). Additionally, enriched Fusobacterium significantly correlated with MRE (Pearson correlation coefficient: 0.235; p=0.003). In contrast, the abundance of Lachnospira, a short-chain fatty acid-producing bacterium, was significantly lower in patients with F234 compared to the F01 group (odds ratio: 0.38; 95% CI: 0.15–0.93; p=0.033). The enrichment of Lachnospira was also negatively correlated with MRE (Pearson correlation coefficient:-0.206; p=0.010). Using the random forest classifier, the gut microbial signature of three genera could differentiate the groups with high diagnostic accuracy (area under the curve: 0.93). The bacterial genera, PNPLA3 polymorphisms, old age, and diabetes were independently associated with advanced fibrosis in multivariable analyses (Figure 1).
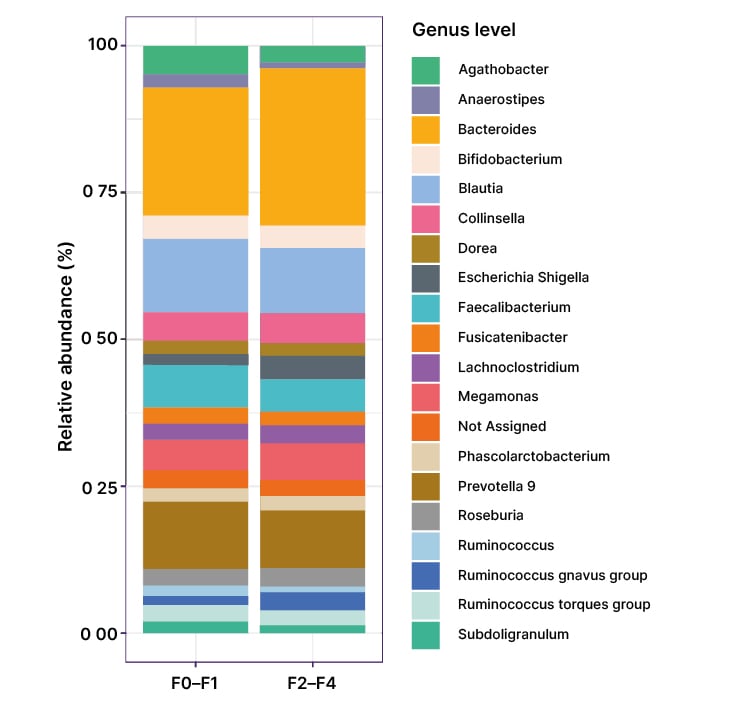
Figure 1: The top 20 relative bacterial compositions at the genus level in the F01 and F234 groups.
CONCLUSION
In an analysis of the gut microbiome of Thai patients with MASLD, the authors found that gut dysbiosis was correlated with the severity of liver disease. Specifically, greater abundance of bacterial genera involving inflammatory processes and lower enrichment of beneficial bacteria were significantly associated with fibrosis severity in patients with MASLD. These results indicated that the imbalance of enriched pathogenic genera and decreased beneficial bacteria, in association with several clinical and genetic factors, were potential contributors to the pathogenesis and progression of MASLD.







