BACKGROUND AND AIMS
Bacterial infection (BI) is a common event in the natural history of cirrhosis, often requiring hospitalisation due to hepatic and extra-hepatic organ dysfunction. Diagnostic criteria for severe infection and sepsis currently adopted in the general population display suboptimal accuracy in patients with cirrhosis.1 Common serum biomarkers such as C-reactive protein (CRP), white blood cells (WBC), and procalcitonin (PCT) are often inaccurate in the early diagnosis of BI in cirrhosis. Presepsin (PSP), a 13 kDa fragment of CD14, is released into the blood upon the activation of monocytes in response to BI and has been evaluated as a promising diagnostic sepsis biomarker and prognostic tool in different populations.2,3 This study aimed to prospectively evaluate PSP in a cohort of hospitalised patients with cirrhosis, with and without BI, to investigate its diagnostic accuracy in comparison with other commonly used biomarkers (i.e., CRP, PCT, and WBC); and to evaluate its prognostic role in short-term mortality.
MATERIALS AND METHODS
All cirrhotic patients admitted at Padua University Hospital between 2016 and 2019 were consecutively enrolled. Patients aged <18 or >80 years and with a prior solid organ transplant were excluded. For each patient, PSP was measured at hospitalisation by Pathfast™ technique (chemiluminescent enzyme immune assay) and its diagnostic accuracy was compared with that of CRP, PCT, and WBC. The 28-day outcome of each patient was evaluated considering liver transplantation as a competing event. Predictors of mortality were assessed with multivariable analysis.
RESULTS
Two-hundred and seventy-eight patients with cirrhosis were prospectively enrolled (males: 179; females: 99; mean±standard deviation [SD] age: 56±11 years; alcohol-related disease: 47.5%), for a total of 448 hospitalisations. The mean±SD Child–Pugh and Model for End-Stage Liver Disease (MELD) score at admission was 9.3±2.5 and 18±8, respectively, whereas 22.5% patients fulfilled criteria of acute-on-chronic liver failure. BI occurred in 28.3% of cases at hospitalisation, with the lower respiratory tract and blood being the most common sources (24% and 19%, respectively). In the whole cohort, the mean±SD PSP value was 1,620±3,014 ng/L. There was a correlation between serum PSP values and severity of underlying liver disease according to Child–Pugh class (p=0.001). Furthermore, serum PSP values were significantly higher in patients with BI than in those without (p=0.001). When comparing patients with similar underlying liver dysfunction, PSP significantly varied according to infectious status in those belonging to Child–Pugh A class (p<0.001), but not among patients with Child–Pugh B and C class (each p=0.06; Figure 1). A PSP cut-off value of 752 ng/L was able to retrieve the best diagnostic accuracy for BI, displaying an area under the curve–receiver operating characteristic equal to 0.685 (95% confidence interval [CI]: 0.63–0.73), with a sensitivity and specificity equal to 66.1% (95% CI: 57.2–74.4) and 63.2% (95% CI: 57.7–68.5), respectively. The diagnostic accuracy of PSP was lower than that of CRP (p=0.002), similar to that of PCT (p=0.18), and better than that of WBC (p=0.006). The short-term mortality was 13.8% in the whole cohort and was significantly higher among patients with BI at hospitalisation than in those without at competing risks analysis (p<0.001). At multivariate analysis, age, acute-on-chronic liver failure at hospitalisation, PSP (hazard ratio: 2.37; 95% CI: 1.29–4.34), but not CRP nor BI, were independent predictors of short-term mortality.
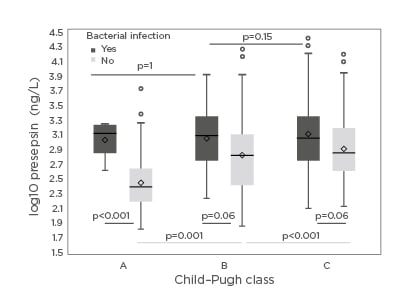
Figure 1: Presepsin values according to severity of underlying liver disease and bacterial infection.
CONCLUSION
Hospitalised patients with cirrhosis had high values of serum PSP. It seemed to be influenced by the severity of underlying liver disease and displayed a diagnostic accuracy lower than that of CRP, but equal to PCT, suggesting a possible role in infection monitoring. PSP was an independent predictor of short-term mortality, reinforcing the role of a proinflammatory state in decompensated cirrhosis.

![EMJ Hepatology [Supplement 2] ILC Congress Review 2020](https://www.emjreviews.com/wp-content/uploads/2020/10/EMJ-Hepatology-8-Suppl-2-Feature-Image-940x572.jpg)






