BACKGROUND AND AIMS
Patients with metabolic dysfunction-associated steatotic liver disease (MASLD) experience difficulties in complying with required lifestyle changes. In particular, long-term improvements have shown to be difficult.1 This study explored the barriers and motivators in patients with MASLD to implement long-term lifestyle changes.
MATERIALS AND METHODS
A quantitative survey with some open-ended questions was distributed via two Dutch patient organisations. The survey included questions about comorbidities, attempts to change lifestyle, motivators and barriers for lifestyle changes, and information provision and information needs. The data was analysed using descriptive statistics.
RESULTS
The survey was completed by 449 patients with MASLD (81% female; mean±standard deviation age: 56±11 years; BMI: 30±5 kg/m2). Sixty-three percent of patients (n=283) self-reported their stage of disease; of which, 16% reported fibrosis/cirrhosis. Patients experienced a high rate of comorbidities, including diabetes mellitus (n=98, 22%), and cardiovascular disease (n=83, 19%). Almost half of the patients (n=210, 47%) experienced joint problems.
The majority of patients attempted one or more lifestyle changes (n=364, 81%), including dietary changes to support weight loss. A low percentage of participants succeeded in permanently changing their diet (n=174, 39%), exercise pattern (n=159, 35%), and permanent weight reduction (n=91, 20%). Most frequently mentioned motivators for lifestyle changes were symptoms of MASLD and/or comorbidities (n=92, 20%), desire to live a long and healthy life (n=76, 17%), and discomfort from being overweight (n=65, 14%). Barriers to implement lifestyle changes were insufficient knowledge about MASLD-related topics (n=177, 39%), stress (n=153, 34%), and lack of practical advice (n= 40, 31%) (Figure 1).
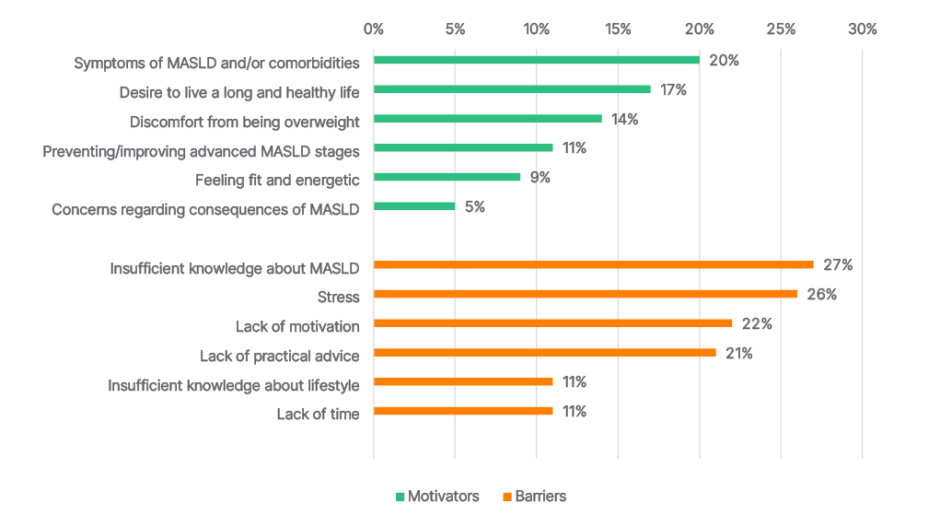
Figure 1: Motivators (n=302) and barriers (n=449).
MASLD: metabolic dysfunction-associated steatotic liver disease.
Information about MASLD was mainly provided by a gastroenterologist (n=210, 47%) or general practitioner (n=123, 27%). Only less than 20% of participants indicated that they had received sufficient information about a broad range of MASLD-related topics. Approximately 72–90% of patients would like to receive more information on almost all MASLD-related topics, including disease specifics and self-management options. Patients were least interested in the topic ‘contact with other patients with MASLD’ (37%).
CONCLUSION
Key reasons to attempt lifestyle changes, in a large population of patients with MASLD, included motivation to improve discomfort and comorbidities related to MASLD and obesity. Although the majority of respondents attempted lifestyle changes, only a minority of them were able to sustain long-term improvements (approximately 20% sustained permanent weight loss). Lack of knowledge about MASLD and stress were key barriers to improving lifestyle in the long term. The authors’ study supports ongoing efforts to increase patients’ knowledge about MASLD and its treatment in order to sustain long-term lifestyle changes.







