A RECENT study highlights an increased risk of thromboembolic events (TEE) in metastatic lung cancer patients treated with immune checkpoint inhibitors (ICIs), particularly those targeting PD-1. Using data from the TriNetX Research Network, which aggregates electronic health records from multiple countries, the study analysed 10,554 patients diagnosed with metastatic lung cancer between 2014 and 2023.
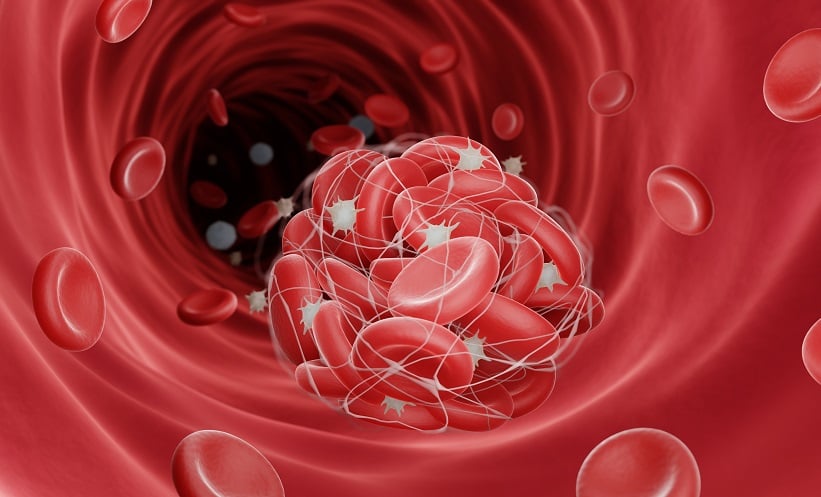
Researchers compared the incidence of venous and arterial thromboembolic events, including deep vein thrombosis (DVT), pulmonary embolism (PE), myocardial infarction (MI), and cerebrovascular accident (CVA), in patients receiving ICIs (anti-PD-1 or anti-PD-L1) with those who did not. The results showed that ICI recipients had a significantly higher incidence of these events compared to non-recipients. Prior to matching for other risk factors, DVT occurred in 20% of ICI recipients, compared to 13.1% in non-recipients. Similarly, PE was found in 17.7% of ICI users, compared to 10.8% in non-users.
When the cohorts were adjusted for demographics and comorbidities, the association remained significant for PE, with ICI recipients having a 1.2 times higher risk of developing pulmonary embolism. Furthermore, patients receiving anti-PD-1 inhibitors had a notably higher rate of PE compared to those receiving anti-PD-L1 inhibitors.
The findings suggest that clinicians should be vigilant for signs of thromboembolism in lung cancer patients undergoing ICI treatment, as these patients face an elevated risk compared to the general population.
Reference
Fowler C et al. Thromboembolic risk among immune checkpoint inhibitor recipients with metastatic lung cancer. Presented at: CHEST Annual Meeting; Oct. 6-9, 2024; Boston.