Abstract
This study consists of a retrospective chart review to evaluate the use of abdominal imaging to aid in the diagnosis of chronic cytopenia. Patients with unclear aetiology of chronic cytopenia often require complex work-up, and it would be beneficial to develop an algorithm to make this process more efficient. Abdominal imaging is a non-invasive procedure that may provide useful clinical diagnostic information as part of an algorithm for this subset of patients. The medical records of 36 patients were reviewed to determine the association between abdominal imaging results and other components of diagnostic work-up. Abdominal imaging was positive for 21 (58.33%) individuals. Following imaging, 8 individuals (22.22%) required bone marrow biopsy and 12 individuals (33.33%) required frequent monitoring, which were non-significant associations. However, positive imaging results were significantly associated with increased BMI as well as severity of thrombocytopaenia. This study suggests that abdominal imaging warrants further study as a potentially useful addition to diagnostic work-up for chronic cytopenia of unknown aetiology.
INTRODUCTION
Normal blood cell count is defined by normal values in all three major haematopoietic cell lineages (i.e., leukocytes, haemoglobin, and platelets) plus normal differential counts in the white cell compartments. The term ‘cytopenia’ refers to a condition in which one or more lineages show abnormally low counts.1 In other words, it denotes a quantitative decrease in the white blood cells (neutrophils), haemoglobin, or platelet count. Cytopenia referrals represent a large proportion of referrals to a haematologist, and often require a multistep workup that might be time consuming and costly to the patient. Many algorithms have been proposed to investigate leucopenia, anaemia, and thrombocytopenia, and to determine their aetiologies. These algorithms are often useful but are by no means universally applicable or substitute the haematologist’s clinical assessment and judgment.2-4
In many patients, the cause of cytopenia is clinically obvious and the correct diagnosis can be established after the initial examination and basic laboratory assessment. However, some patients with chronic cytopenia, especially in the setting of a tertiary referral centre, have less clear aetiology; therefore, workup requires a multi-step, complex approach with specialised testing that often includes bone marrow examination. It would be advantageous for both patient and physician to develop a refined algorithm to examine and diagnose this subset of patients.
Abdominal ultrasound imaging is a readily available, low cost imaging procedure that does not use ionising radiation, thus posing minimal risk to patients. It is convenient and does not require venous access or administration of contrast material. This modality is effective in evaluating abdominal organs for various indications and aides in evaluating organ dysfunction as a possible aetiology of haematologic abnormality. Abdominal CT and MRI are other possible imaging techniques that can also result in better anatomic definitions of abdominal organs. The role of abdominal ultrasound imaging or abdominal imaging via other modalities has not been investigated as a part of a workup algorithm for cytopenia. The aim of this study was to retrospectively evaluate the use of abdominal imaging in a haematology practice in a tertiary medical centre. Specifically, this study examines the use of abdominal imaging, via an ultrasound or CT scan, to identify the aetiology of haematologic abnormalities. It will also examine the association between abdominal imaging results and need for bone marrow examination for these cases. It was hypothesised that abdominal imaging would lead to more identified aetiologies in adjunct to a thorough history, examination, and laboratory workup for patients referred for haematology evaluation in a tertiary medical centre.
METHODS
This study is a retrospective electronic chart review of patients seen at The University of Kansas Cancer Center, Kansas City, Missouri, USA, which is a tertiary referral centre with a wide referral base that includes primary care physicians as well as medical and surgical subspecialists. This study received Institutional Review Board approval.
SETTING
Patients referred to this haematology clinic were evaluated by thorough medical history, physical examination, review of prescription and over-the-counter medications, and discontinuation of medications suspected to be contributing to cytopenia or medications that are not indicated. Standard laboratory workup includes repeating blood counts; reticulocyte count (if anaemia is present); and peripheral blood smear by a haematologist or haematopathologist. Further workup includes evaluation of nutritional deficiencies including serum iron, vitamin B12, and folate levels; anaemia including direct Coomb’s test, lactate dehydrogenase, haptoglobin (if anaemia is present); serum copper (if neutropenia is present); hepatic and renal functions; thyroid function; chronic infections, including HIV and hepatitis viruses (if indicated); autoimmune disorders; and haematologic malignancies if clinical stigmata are present. If this workup fails to identify the aetiology of the cytopenia, abdominal imaging via an ultrasound or CT scan has been incorporated as a second-tier workup to exclude radiologic evidence of organ dysfunction as a culprit for the haematologic abnormality.
If a diagnosis is made, the patient is managed appropriately and discharged to the referring physician. However, if the aetiology of the haematologic abnormality is not evident despite the above workup, the patient is offered a bone marrow biopsy and aspiration, or offered frequent follow up (i.e., at least every 6 months) with a haematologist if bone marrow examination is not indicated or declined.
This review focusses on the medical charts of patients referred to a single haematologist for one or more cytopenias between August 2011 and July 2013. Inclusion criteria included patients who presented for initial workup and subsequently required abdominal imaging for evaluating the cytopenias. Patients with prior abdominal imaging within 2 years and patients with haematologic malignancy at presentation or diagnosed through workup were excluded. The following data were extracted via medical chart review: patient age, sex, BMI, number of cytopenias, severity of cytopenias, 67 results of abdominal imaging, diagnosis after imaging study, and outcome (i.e., patient discharged or followed infrequently; patient had bone marrow biopsy; or patient needed frequent monitoring).
Analyses
The lower limits of normal haematologic parameters were adopted per institutional laboratory references. For this analysis, the authors defined the severity cut-offs for cytopenias as follows: mild neutropenia was defined as 1,000–1,800×106/L; moderate neutropenia was 500–1,000×106/L; and severe neutropenia was <500×106/L. Mild anaemia was defined as 10.0–13.5 g/dL in men or 12 g/dL in women, moderate anaemia was 8–10 g/dL, and severe anaemia was <8 g/dL. Mild thrombocytopenia was defined as 100–150×106/L, moderate thrombocytopenia was 50–100×109/L, and severe thrombocytopenia was <50×109/L. Descriptive statistics were calculated for subject demographic data and clinical results. Chi-square test (or Fisher’s exact test when indicated) was used to examine the association between abdominal imaging and necessity of subsequent bone marrow biopsy. Chi-square test was used to examine the association between number of cytopenias and abdominal imaging result (i.e., positive or negative). Chi-square test was used to examine the association between severity of cytopenias (i.e., mild versus at least one moderate or severe cytopenia) and abdominal imaging result. Chi-square tests examining the association between 1) presence and the Cochran-Armitage test for 2) severity of thrombocytopenia with positive abdominal imaging result were also run.
The Cochran–Mantel–Haenszel test was used to calculate the 88 odds ratio of abdominal imaging and outcome-monitoring frequency, adjusted for bone marrow biopsy. The Cochran–Armitage test for trend and unconditional logistic regression were run to examine association of BMI and result of abdominal imaging test (i.e., positive or negative), treating BMI as categorical and continuous exposure measures, respectively. All data analyses were performed in SAS 9.3.
RESULTS
Descriptive Results
Thirty-six patients met all inclusion criteria. The demographics and baseline characteristics are outlined in Table 1. The average patient age was 54.4 years (range: 21.0–84.0) and average BMI was 31.5 kg/m2 (range: 18.0–53.0). Table 2 presents a descriptive summary of neutropenia, thrombocytopenia, and anaemia results. In total, 21 individuals (58.33%) had one cytopenia, 14 individuals (38.89%) had two cytopenias, and 1 individual (2.78%) had three cytopenias. Fifteen individuals (41.67%) had only mildly severe cytopenia(s) and 21 individuals (58.33%) had at least one moderate or severe cytopenia. Abdominal imaging consisted of abdominal ultrasound in 33 patients and abdominal CT scan in 3 patients. Imaging identified abnormalities for 21 individuals (58.33%). Abnormalities detected by imaging included splenomegaly (n=14), liver disease or cirrhosis (n=13), renal cell carcinoma (n=2), and ovarian tumour and lymphadenopathy (n=1). Following imaging, eight individuals (22.22%) required bone marrow biopsy and 12 individuals (33.33%) required frequent monitoring.
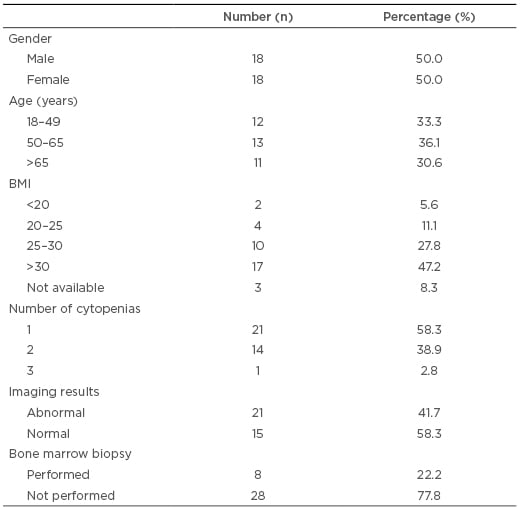
Table 1: Sample demographics and baseline characteristics (N=36).
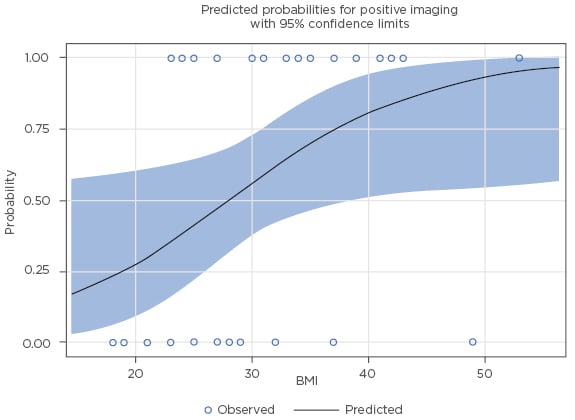
Table 2: Frequency (n, and percentage %) of severity of cytopenias (N=36).
Inferential Results
Abdominal imaging in the study subjects showed abnormalities that are implicated in blood decreases at a high rate, including three occult, clinically significant malignancies. There was not a significant association between detecting abnormal imaging and necessity of bone marrow biopsy (p>0.99). Detecting abnormal imaging and subsequently identifying the probable aetiology of the cytopenia was associated with successful discharge from the haematology clinic or less frequent monitoring, but this did not reach statistical significance (p=0.14). The association between BMI and detecting abnormal imaging was statistically significant; specifically, increased BMI was associated with increased probability of positive imaging result when BMI was assessed both as a categorical (ordinal) measure (p<0.01) and as a continuous measure (p=0.04; see Figure 1).
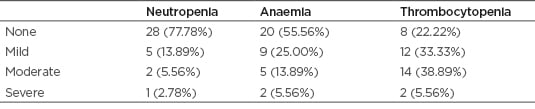
Figure 1: Association between BMI and detection of abnormal abdominal imaging.
There was not a significant association between the number of cytopenias (1 versus ≥2; p=0.86) and detection of abnormal imaging. There was no significant difference in the proportion of positive imaging tests between those with all mild cytopenias compared to those with at least one moderate or severe cytopenia (p=0.23). Thrombocytopenia was significantly associated with detecting abnormal imaging tests. Of those with a diagnosis of thrombocytopenia, 68% had a detected abnormal imaging test result. In contrast, only 25% of individuals without a diagnosis of thrombocytopenia had abnormal imaging (p=0.0461). There was also a significant trend of increasing detection of abnormal imaging, ranging from 25% for individuals without thrombocytopenia to over 80% for those with moderate-to-severe thrombocytopenia (p=0.0094).
DISCUSSION
Blood cell production is tightly controlled by several complexes, interacting biological networks (including the growth factor and cytokine networks), the haematopoietic microenvironment, the immune system, other intercellular communication networks, and diverse intracellular communication networks.5-8 In addition, genetic, epigenetic, and metabolic factors contribute to the regulation of blood cell production. Each of these mechanisms may act together to control and maintain blood cell counts at a remarkably constant ‘physiologic’ range in a healthy person throughout his or her lifetime. This process is very sensitive to many physiologic and pathologic processes that include, but are not limited to, nutritional factors; immune disorders; connective tissue disease; chronic diseases and chronic inflammatory conditions; infections; organ dysfunction in the hepatic, renal, and endocrine systems; medication effects or side effects; and haematologic malignancies and paraneoplastic phenomena in association with solid tumours. Disruption in these regulatory factors or acquisition of a disruption in the normal physiologic processes may cause or contribute to the development of one or more cytopenias. This study investigated the role of abdominal imaging in evaluation of the aetiology of cytopenias at a haematology clinic in a tertiary medical centre. Results yielded a notably high rate (58%) of abnormal abdominal imaging detection in this population. The imaging results have led to identifying the aetiology of the cytopenia in many subjects resulting in a final diagnosis and the lack of need for frequent observation. This is supporting the hypothesis that abdominal imaging would be of value in the algorithms of identifying aetiologies of cytopenia(s). Additionally, abdominal imaging in this cohort identified three subclinical malignancies that were resected with curative intentions, and evidence of clinically significant liver disease triggering the need of referral to the hepatology team.
Abdominal imaging was most likely to be abnormal and therefore helpful for workup of patients with thrombocytopenia, possibly by identifying a high rate of occult liver disease.
Notably, abdominal imaging abnormalities were detected more significantly in association with increased obesity. The authors propose that this is plausibly related to more challenging physical examination in patients with obesity, or due to higher prevalence of liver disease in those subjects. Abdominal imaging did not mitigate the need for bone marrow biopsy although the number of bone marrow biopsies performed in this cohort was small.
CONCLUSION
The results of this small, retrospective chart review yielded initial, clinically relevant observations to support a larger, prospective study of the role of abdominal imaging in diagnosis of chronic cytopenias. In this study, abdominal imaging proved to be a high yield test in the workup of cytopenias as a second-tier test. The imaging is most pertinent in patients with thrombocytopenia and in patients with high BMI. Reaching a more acute assessment of the aetiology of the cytopenias, as assisted by abdominal imaging, can have significant clinical impact on these patients and possibly provide a cost-saving advantage by limiting the need for frequent follow up. Prospective study will be needed to confirm this.







