BACKGROUND AND AIMS
The historical International Prognostic Score (IPS-7), which was developed with patient data from the 1980s, and the more recent IPS-3 clinical prediction models are thought to be less powerful in distinguishing good- and poor-risk groups among patients with advanced-stage classical Hodgkin lymphoma (cHL).1,2 Recently, the advanced-stage Hodgkin lymphoma international prognostic index (A-HIPI) model was created, and it was found to be superior when compared to IPS-7 and IPS-3 in terms of predicting prognosis in patients with advanced-stage cHL.2 It has also been validated in a few studies coming from different countries. The authors, for the first time, aimed to validate the A-HIPI model among Turkish patients with cHL, and to compare A-HIPI with other clinical prediction models.
MATERIALS AND METHODS
Patients with advanced-stage (2B, 3, and 4) cHL who were diagnosed between 2005–2018 were evaluated retrospectively. IPS-7, IPS-3, and A-HIPI scores were calculated, and the authors compared the performance of these models in terms of predicting progression-free survival (PFS) and overall survival (OS). To compare their calibration and their power to discriminate between low-risk and high-risk patients, discrimination and calibration analyses were performed. The C-index (Harrell’s Concordance Index) method for discrimination, visual examination of calibration curves, calibration intercepts and calibration slope were evaluated for calibration. Models were compared with Akaike’s information criteria (AIC).
RESULTS
The authors included 207 patients with a median age of 37 years (range: 18–82 years). There were 19 patients (9.2%) aged >65 years. Fifty eight percentage of patients were male, and the percentages of patients with stages 2B, 3, and 4 disease were 28%, 37.2%, and 34.8%, respectively. All but five patients (97.6%) received a combination of doxorubicin, bleomycin, vinblastine, and dacarbazine as first-line therapy. The percentages of patients with IPS-7 scores 0, 1, 2, 3, 4, and ≥5 were 4.3%, 16.4%, 27.5%, 30%, 15%, and 6.8% respectively and 30.4%, 38.7%, 24.6%, and 6.3% for IPS-3 scores 0, 1, 2, and 3 respectively. With the A-HIPI model, the expected 5-year median PFS and OS were 76.6% and 92.3%, respectively. With a median follow-up of 75 months, 37 patients (17.9%) died. The 5-year PFS and OS were 67% and 84.9%. respectively. With regression analyses, all 3 models were found to be prognostic for PFS and OS for the entire cohort. In terms of OS, the model with the highest C-index in the entire sample and in patients ≤65 years of age is A-HIPI (C-index for the entire sample: 0.740, 95% CI: 0.642–0.838; C-index for patients ≤65 years of age of which it is validated: 0.726, 95% CI: 0.613–0.840). In terms of PFS, the model with the highest C-index is IPS-3 (C-index: 0.619, 95% CI: 0.535–0.703). In terms of PFS, the A-HIPI model had the lowest C-index (0.591, 95% CI: 0.506–0.677). The A-HIPI model showed a better fit with the authors’ study data in determining the prognosis in terms of OS by AIC analysis (A-HIPI, IPS-7 ΔAIC: 12.8; A-HIPI, IPS-3 ΔAIC: 9.7), and IPS-3 model showed a better fit in terms of PFS. In the patient group >65 years of age, all three models were not prognostic. In terms of PFS and OS, the A-HIPI model appears to be prognostic and well-calibrated except for the patient group aged >65 years (Figure 1).
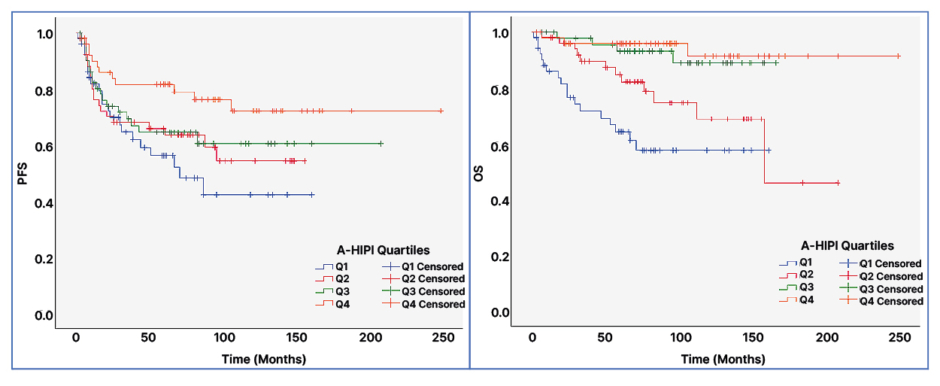
Figure 1: Kaplan-Meier survival analysis for the advanced-stage Hodgkin lymphoma international prognostic index (A-HIPI) quartiles.
Patients were divided into four groups (quartiles) according to their A-HIPI expected PFS and OS scores. Q1 represents the group with the lowest expected survival, and Q4 represents the group with the highest expected survival with the A-HIPI model.
A-HIPI: advanced-stage Hodgkin lymphoma international prognostic index; PFS: progression-free survival; OS: overall survival.
CONCLUSION
The authors’ study validated the A-HIPI model among homogeneously treated patients from a tertiary referral center in Türkiye. The A-HIPI model was observed to have a better performance than other models, except for patients aged >65 years. A new clinical prediction model is needed for patients >65 years as A-HIPI has not been validated for this population.






