Meeting Summary
This expert masterclass, supported by an independent grant from OM/Vifor Pharma, brought together physicians specialising in vascular surgery, gynaecology, and dermatology, from Pakistan, Egypt, Turkey, Lebanon, and Germany, to discuss the current management of chronic venous disease and haemorrhoidal disease (HD). The meeting included plenary lectures and interactive case study discussions, allowing delegates and presenters to take part in high-level discussions of pressing issues within the field.
EPIDEMIOLOGY, PREDISPOSING FACTORS, AND PATHOPHYSIOLOGY OF HAEMORRHOIDAL DISEASE
Epidemiology
The scale of HD is difficult to quantify due to patient misconceptions regarding anal health and poor practice both by physicians and the healthcare industry at large. Nevertheless, estimates suggest that haemorrhoids are highly prevalent with 10 million patients a year experiencing symptoms in the USA and >50% of people >50 years of age having had HD within their lifetime.1
Patients mistakenly consider many benign or malignant conditions of the anal area to be related to HD. For example, >50% of patients presenting with distal rectal cancer report having had HD which worsened a little in the preceding weeks. In addition, many patients may self-diagnose and treat conditions such as anal fissures, pruritus, or genital warts as HD. Such self-diagnosis, and the attendant risk of mistaken treatment, is supported by some insurance bodies in order to sustain a lower number of visits to doctors and reduce paid-prescription coverage. Furthermore, clinicians may prefer prescribing anti-haemorrhoidal drugs compared with undertaking detailed investigations into the true nature of anal conditions.
Historical data, based on UK’s National Health Service (NHS) records, indicates that in the 1970s 44% of UK inhabitants had visited their family doctor due to haemorrhoidal symptoms during their lifetime; prevalence of surgery for HD was ~4.5%. More recent epidemiological data from St Mark’s Hospital and Academic Institute, London, UK, the mecca of colorectal surgery in Europe, shows a HD prevalence of 13−36% within the general population.2 The actual prevalence is likely to be a little lower, as misreporting by patients or less experienced family physicians may result in erroneously inflated rates. Data from the USA indicate that HD affects 40−50 people in 100,000 (1.2 million/300 million).3,4 In the USA, >32,000 annual surgeries are carried out, and 1.5 million HD-related prescriptions are paid by Medicare and insurance companies. In addition, millions of people turn to over-the-counter formulas, herbs, or alternative medicines every year.
Predisposing Factors
A number of speculative risk factors for HD have been proffered including: seasonality, occupation, psychiatric conditions, cultural traditions, tight clothing, food style, erect posture, genetic heritability, irrıtable bowel syndrome, and sphincter tonus abnormalities. Evidence-based risk factors include: hormonal changes in pregnancy and child birth, ageing, insufficient dietary fibre or chronic diarrhoea, anal intercourse, constipation, and prolonged straining during defecation. People between the ages of 45–65 years most frequently report symptoms of HD. Gender does not appear to affect HD prevalence, although pregnancy is known to exacerbate symptoms.
Pathophysiology
A study investigated electrical waves associated with sampling, the response caused when a stool moves down and a person squeezes their sphincter to push the stool back up, in ambulatory patients. Sampling produces two wave forms: the ultra-slow wave and the giant ultra-slow wave. Both of these wave forms increased by 30% in people with prolapsing HD compared with controls, and the number of waves per hour was also significantly increased (p<0.05) in prolapsing HD patients. In addition, both day-time and night-time sphincter spike potentials were significantly higher compared with controls. These data indicate a different anorectal physiology in patients with HD, although the direction of causality has yet to be determined. Notably, in the majority of cases, these abnormalities are corrected by haemorrhoidectomy.5 In addition, patients with HD display increased resting anal pressure without any significant change in internal sphincter thickness.6
Shearing of ligaments is a major feature of HD pathophysiology (Figure 1). Straining causes engorgement of veins via blockade of venous return, which causes an increase in venous pressure. The lumen for stools to pass through narrows and the mucosa thins due to this stretching, and enzymes or mediators further contribute to the degradation of supporting tissues in the anal cushions. Matrix metalloproteinase 9 (MMP-9), which has a key role in the pathophysiology of Crohn’s disease, is overexpressed in HD tissue and acts to degrade extracellular proteins such as elastin, fibronectin, and collagen.7 Chronic overstraining with the attendant increases in pressure, stretching of vessels, engorgement, and stretching of the mucosa, eventually results in shearing of these ligaments, resulting in migration of the pile downwards, especially during defecation. In cases where the ligaments are partly intact, the haemorrhoidal piles will return to their original position after straining. However, when all ligaments are lost the pile will drop down and will not return to its original position.
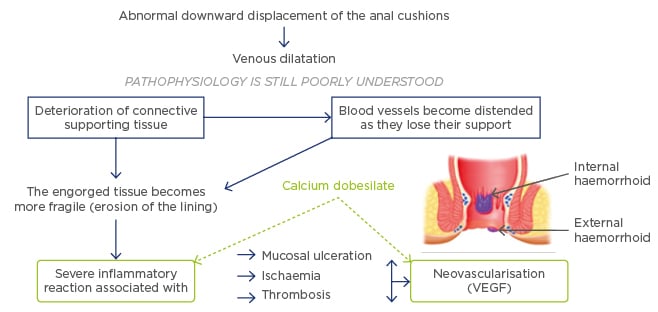
Figure 1: Pathophysiology of haemorrhoidal disease.12
VEGF: vascular endothelial growth factor.
Haemorrhoids have a tendency for hypervascularisation (Figure 1). MMP-9 and the related proteinase MMP-2 promote angioproliferative activity through transforming growth factor-β (TGF-β).8 Expression of the TGF-β binding site endoglin (CD105), vascular endothelial growth factor (VEGF), and microvascular density are all increased in Grade III–IV HD.7,9 In addition to microvascular changes, the terminal branches of the superior rectal artery supplying the anal cushion exhibit larger diameters and greater blood flow, which correlate with HD severity. In the normal anal canal (AC) a sphincter-like structure is formed by a thickened tunica media, however in HD this sphincter-like mechanism disappears. The loss of this mechanism further increases blood flow alongside increased vascularisation.10 These changes are surgery resistant and are likely drivers of recurrence. Dysregulation of the vascular tone, related to changes in vascular smooth muscle and the overlying endothelium, also likely contributes to pathophysiology, as evidenced by venous dilatation/distortion and increased production of vasodilator nitric oxide in HD tissue.7,11 In addition to the above mechanisms, severe inflammation of the vascular wall and connective tissue occurs within haemorrhoidal tissue and has been shown to be associated with complications including ischaemia, thrombosis, and mucosal ulceration (Figure 1).12
In summary, the major features of HD pathophysiology include structural changes to the supporting tissues within the AC; morphological changes to the existing vasculature and extensive neovascularisation; and inflammatory changes within the vascular wall and connective tissue.
CLINICAL SIGNS AND SYMPTOMS
Classification
The American Society for Colorectal Surgeons (ASCRS) has created recommendations for the diagnosis of HD, and the European Society for Coloproctology (ESCP) are currently in the process of creating their own diagnostic criteria. ASCRS guidelines note that the diagnosis of HD is almost always clinical. History must be taken and include data on the extent, severity, and duration of symptoms, as well as information on bleeding, prolapse, pain, and issues of hygiene. Lifestyle considerations such as fluid and fibre intake should also be noted in addition to the review of bowel habits including frequency, consistency, and ease of evacuation.
Physical examination should typically include visual, digital, and anoscopic examinations. Clinicians should look for evidence of thrombosis; concomitant anorectal pathology, especially fissures, fistulas, and abscesses; and crucially, evidence of Crohn’s disease. The presence of a history of conditions related to HD such as inflammatory bowel disease or other rectal conditions should be investigated. In addition, the use of medications which aggravate HD, like metformin, or drugs which increase risk of bleeding, like aspirin, should be recorded.
HD is graded with increasing severity from I−IV (Table 1). Grade I is defined by prominent haemorrhoidal vessels with no prolapse. The pathology is internal and can be visualised by anoscopy and the patient is likely to complain of bleeding, some leakage, and discomfort. Grade II is characterised by prolapse during the Valsalva manoeuvre, straining, and defecation. However, the ligaments are sufficiently intact to pull the piles back up. Grade III is distinct from Grade II because, although the ligaments remain somewhat intact, the prolapse requires manual reduction. Finally, Grade IV HD occurs when there are no remaining intact ligaments; haemorrhoids remain chronically prolapsed and are not manually reducible.
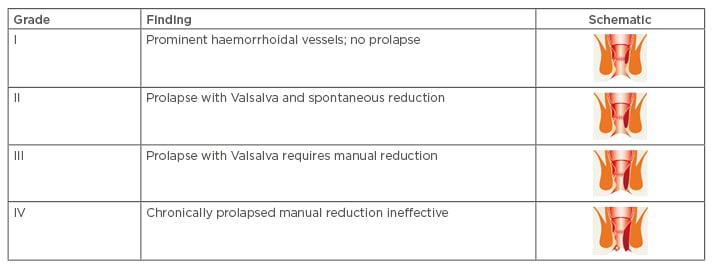
Table 1: Classification of haemorrhoidal disease.
A lesser-known classification exists based on anatomical findings and aimed at describing the difficulty of performing corrective surgery. Primary haemorrhoids are prolapsed and present at the typical three sites of the anal cushions. Secondary haemorrhoids are classified by additional piles between the three primary haemorrhoids; this increases the difficulty of surgery due to the higher risk of stricture. Patient satisfaction is also more difficult to achieve as avoiding stricture is likely to necessitate leaving some minor prolapse. Lastly, the most serious grade is circumferential haemorrhoids, which increase the difficulty of all the above-mentioned issues.13
Symptoms
HD symptoms may be classified as direct (bleeding, palpable, prolapsed piles) or indirect (wet anus with soiling and discomfort, and thrombosis which results in pain). Bleeding related to haemorrhoids is typically bright red, painless, and is visualised by drops of blood in the bowl following defecation. When there is no obvious source of bleeding on anorectal examination or when the patient has significant risk factors for colorectal neoplasia then bleeding should not be attributed to haemorrhoids until the colon is adequately evaluated.14 Depending on the colorectal cancer risk profile, colonoscopy or the cheaper sigmoidoscopy may be recommended. Risk factors beyond bleeding include age, family history, and the presence of previous conditions related to bowel cancer such as inflammatory bowel disease, breast cancer, or an ovarian pathology.
Under normal circumstances, HD is painless and the patient only complains of discomfort. Pain occurs in conjunction with thrombosis, particularly in an external haemorrhoid, or if a fourth- degree internal haemorrhoid becomes strangulated. Related issues such as an underlying abscess or anal fissure may also cause pain.
Physical Examination
Physical examination should include digital examination and anoscopy. The perianal area should be inspected for anal skin tags, external haemorrhoids, perianal dermatitis from anal discharge or faecal soiling, fistula-in-ano, or anal fissure. Straining can ease physical examination in cases of internal haemorrhoids. Digital examination should be used to assess abnormal anorectal masses, anal stenosis and scarring, and anal sphincter tone. In older men, prostatic symptoms, which underlie straining during micturition, should be assessed as part of differential diagnosis.
During anoscopy, haemorrhoidal size, location, severity of inflammation, and bleeding should be noted. This assessment should be used to decide if surgery is indicated and which is the most appropriate form. Intra-rectal retroflexion of the colonoscope or transparent anoscope with flexible endoscope allow excellent visualisation of the AC and can permit recording of pictures in most cases.15
SURGICAL MANAGEMENT OF HAEMORRHOIDAL DISEASE
There are many different surgical procedures available to treat HD, unfortunately, none of them is ideal, necessitating careful consideration as to what the best procedure is for each individual patient. The clinical presentation, severity of disease, and risk of recurrence should all be considered before initiating surgery. Furthermore, although effective, classical procedures are associated with considerable pain and, in some cases, rare but very serious complications.
Depending on the grade of HD presented, physicians may consider lifestyle interventions, pharmacological agents, or office procedures such as rubber-band ligation or cryotherapy, before undertaking surgical interventions. However, for Grade III and IV HD, and refractory cases of Grade II, surgery is often necessary. Open (Milligan-Morgan) and closed (Fergusson) haemorrhoidectomy represent common ‘classical’ procedures. These procedures vary in popularity regionally with Milligan-Morgan more common in Pakistan and Fergusson more common in the USA, for example. Newer forms of haemorrhoidectomy using energy devices like the LigaSure™ device (Medtronic, Minneapolis, Minnesota, USA) or laser ablation are now also available. In addition, procedures which do not excise the prolapsed anal cushion, but rather try to restore the anatomy and physiology of the AC, such as stapled haemorrhoidopexy and haemorrhoidal artery ligation (HAL) with anopexy, are now available.
Haemorrhoidectomy
Surgical treatment is used in about 5–10% of HD cases. Common complications include: urinary retention, pain, bleeding, anal stenosis associated with open surgery, perianal fistula, incontinence, and recurrence. Rates of complications range from 3–12% and, although rare, some like anal stenosis are very difficult to treat. Many patients avoid surgery until they experience circumferential prolapse of the anal cushion at which stage surgery is challenging and patient satisfaction is difficult to achieve. Milligan-Morgan has previously been described as the ‘The Gold Standard’ surgical procedure for HD. However, although good results can be achieved with early Grade III HD, in cases of circumferential prolapse unexcised tissue often leads to patient dissatisfaction.
Milligan-Morgan and Fergusson haemorrhoidectomy have similar results with respect to pain, postoperative complications, scarring, and surgical duration. The choice between these techniques is likely to derive from the personal experience of the surgeon and patient preference.16 Comparison of classical open haemorrhoidectomy showed a significantly shortened surgical time with LigaSure. It has been proved to be a safe and effective procedure with less blood loss and postoperative pain, as well as fewer complications compared with conventional haemorrhoidectomy. In addition, the technique is technically simpler as it avoids the use of sutures and reduces the need for haemostasis.17 However, these benefits have not been demonstrated in all studies and there are additional costs related to this technique.
Minimally Invasive Techniques
The deficiencies in ‘classical’ surgical procedures have led to the development of new techniques which aim to reduce postoperative pain, shorten recovery time, reduce complications, and lower recurrence rates. Unfortunately, current progress suggests that achieving some of these objectives is difficult without a trade-off, for example techniques which reduce postoperative pain may result in a higher recurrence rate.
The minimally invasive technique of mucopexy, with or without mucosal resection and HAL, is being increasingly used. Mucopexy, which is also known as rectoanal repair (RAR), aims to correct the underlying pathophysiology of HD while sparing the sensitive anoderm resulting in a rapid return to normal life without pain, and increased patient satisfaction.18 The trade-off is a slightly higher risk of recurrence, although the procedure can be repeated in cases of recurrence.
Stapled haemorrhoidopexy was introduced approximately a decade ago. The technique involves mucosal and submucosal resection 4–5 cm above the dentate line, an area which is insensitive to pain, with a circular stapler. The distal and proximal mucosa are fixed together using the stapling device following resection. The procedure both interrupts the arterial blood flow to the haemorrhoids, allowing involution of the haemorrhoidal plexus, and pulls the anal cushion back to its normal position. In a systematic review, stapled haemorrhoidopexy resulted in less postoperative pain and improved patient satisfaction (odds ratio [OR]: 2.33; p=0.003), but an increased recurrence rate (OR: 3.48; p=0.02), compared with haemorrhoidectomy. The rate of complications did not differ significantly between the two techniques (20% versus 25%, p=0.06, for haemorrhoidopexy and haemorrhoidectomy, respectively).19 However, stapled haemorrhoidopexy is associated with some serious complications including anastomotic bleeding, requiring blood transfusion, and pelvic sepsis necessitating colostomy.
HAL was introduced many years ago, however the technique was associated with a very high recurrence rate. More recently, it has been combined with RAR (HAL-RAR) resulting in an acceptable recurrence rate. The resulting combined procedure is an effective and minimally invasive treatment for Grade III and Grade IV HD.20 Specialised equipment is available allowing localisation of the haemorrhoidal arteries using a Doppler-ultrasound probe followed by ligation using a suture inserted into the device. The arterial ligation reduces blood flow to the anal cushions while the next part of the procedure uses a running suture to bring the prolapsed anal cushion back to its normal position. The whole procedure is carried out above the dentate line to avoid pain. The technique is relatively easy to master and leaves a more natural appearance than classical haemorrhoidectomy procedures. There is a growing body of evidence on the effectiveness of HAL-RAR and National Institute for Health and Care Excellence (NICE) guidelines state that HAL represents “an efficacious alternative to conventional haemorrhoidectomy or stapled haemorrhoidopexy in the short and medium term [with] no major safety concerns.”21-29
Real-World Experience with Haemorrhoidal Artery Ligation and Rectoanal Repair in Pakistan
A prospective observational study based in the general-surgical units of three hospitals was recently carried out to assess HAL-RAR. Patients (N=150) with symptomatic Grade III or IV HD or failure of band ligation for Grade II underwent HAL-RAR and received 2 weeks of postoperative treatment with the phlebotonic calcium dobesilate. Outcomes including postoperative complications and pain were assessed over a 1-year follow-up which included physician visits at 2 and 6 months.
The majority (n=116) of patients were male with a mean age of 45 years. Mean (range) operating time was 45 minutes (35−65 minutes), with a mean of 7 HALs and 3 RARs per patient. The mean hospital stay per patient was 19 hours (14−48 hours). There were some early issues with postoperative pain (18 patients required narcotic analgesics and four patients complained of excessive pain, which in two patients lasted for 5 days). However, these issues did not persist following more diligent attempts to keep the RAR procedure above the dentate line. Early postoperative complications included retention of urine (n=5) and mild self-limiting bleeding (n=7). Patient satisfaction was high (83%) though the study was limited by the lack of a long-term follow-up and a comparator arm. In summary, HAL-RAR is a safe surgical method, which can reduce symptoms of Grade II and III HD with high patient satisfaction.
MEDICAL MANAGEMENT
Medical management of haemorrhoids is always indicated and is sufficient in >50% of cases. Therapeutic strategies include a combination of flavonoid derivatives, calcium dobesilate, regularisation of gut motility and defecation, general and dietary advice dealing with constipation, and topical treatments (e.g. calcium dobesilate with dextromethorphan and/or lidocaine).
The treatment algorithm for Grade I and II haemorrhoids from the 2006 consensus statement by the Society of Surgeons of Pakistan and Pakistan Medical Association (PMA), recommends dietary and lifestyle modification, micronised purified flavonoid fraction (MPFF), and topical treatment. MPFF is a flavonoid therapy and, as such, acts by prolonging the vasoconstrictor effect of noradrenaline on the vein wall, increasing venous tone, and therefore reducing venous capacitance, distensibility, and venous stasis. In addition, flavonoids act to increase venous return, reduce hypertension, and protect venous valves from leukocyte-induced inflammation and destruction thus helping to prevent the appearance of reflux.
Since these 2006 recommendations, the use of the phlebotonic calcium dobesilate has become more widespread. Calcium dobesilate has previously demonstrated efficacy in the treatment of diabetic retinopathy and chronic venous insufficiency, and beneficial effects include: decreased capillary permeability, decreased platelet aggregation, decreased blood viscosity, decreased bleeding, and increases in lymphatic transport. In addition, calcium dobesilate targets two key pathophysiological features of HD (Figure 1): anti-inflammatory effects have been demonstrated both indirectly through reductions in leukocyte recruitment and directly through inhibition of inflammatory mediators; and antiangiogenic effects have been demonstrated both through reductions in VEGF expression and blockade of VEGF- induced angiogenesis, and through blockade of fibroblast growth factor activity.30-36
Evidence for Efficacy of Phlebotonics in Haemorrhoidal Disease
Calcium dobesilate is indicated for the treatment of HD which does not require surgery. In addition, calcium dobesilate therapy can be utilised within a regimen with includes surgical intervention. Therapy before surgery can be used to reduce inflammation in the run up to surgery, in addition calcium dobesilate can be used post-surgery to reduce symptoms and aid in healing.
Cochrane conducted a systematic review into the evidence base for phlebotonics in HD.37 The review identified 24 eligible randomised controlled trials, 20 of which were eligible for inclusion (N=2,344). Phlebotonics demonstrated a statistically significant beneficial effect in comparison with placebo for the outcomes of pruritus (OR: 0.23; 95% confidence interval [CI]: 0.07–0.79; p=0.02), bleeding (OR: 0.12; 95% CI: 0.04–0.37; p=0.0002); bleeding post-haemorrhoidectomy (OR: 0.18; 95% CI: 0.06–0.58; p=0.004), discharge and leakage (OR: 0.12; 95% CI: 0.04–0.42; p=0.0008), and overall symptom improvement (OR: 15.99; 95% CI: 5.97–42.84; p<0.00001).37 The sole symptom assessed where a significant improvement was not achieved compared with placebo was pain.
Three English language studies assessing the efficacy of calcium dobesilate in HD are available. Sarabia et al.38 conducted a double-blind, 4-week study of calcium dobesilate (1.5 g/day) versus the flavonoid fraction of diosmin (1.5 g twice a day) in 51 patients with acute episodes of HD. Blinding was maintained for the first 10 days and symptoms (pain, discharge, pruritus, oedema, inflammation, bleeding, and anal pressure) assessed at baseline Day 2, Day 8, and at 4 weeks. At Day 2, there was a significant improvement in six of the seven symptoms in the diosmin arm and all seven symptoms in the calcium dobesilate arm (Figure 2). After 4 weeks, 76% of patients in the calcium dobesilate group and 73% in the diosmin group were asymptomatic, both drugs were similarly well-tolerated. In summary, the same efficacy was achieved with half the number of daily doses of calcium dobesilate compared with the active control.38
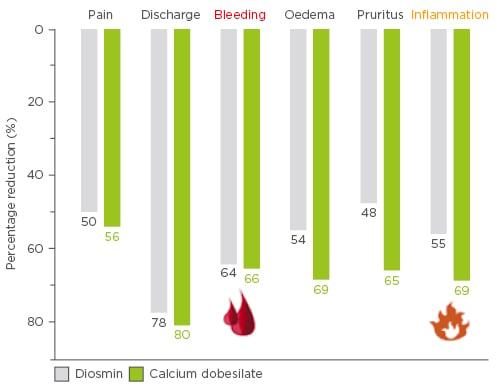
Figure 2: Effect of 2 days of calcium dobesilate or diosmin therapy on haemorrhoidal disease-related symptoms and inflammation.38
In a 2-week randomised double-blind study, patients with Grade I or II HD received either calcium dobesilate (n=29) or a high fibre diet (n=16). Symptoms and anoscopic inflammation were scored on a scale from 0–2 at baseline and after treatment. Patients treated with calcium dobesilate achieved a significant reduction in symptoms and anitis at Week 2 compared with baseline. In addition, anoscopic inflammation was significantly better in the calcium dobesilate group compared with the diet group. The authors concluded that together with the recommendations about diet and bowel and discipline, oral calcium dobesilate treatment provides an efficient, fast, and safe treatment for acute symptoms of HD.39
Calcium dobesilate is currently the only phlebotonic available as a topical therapy. A combined topical/oral regimen was assessed in a 6-week randomised double-blind study of 115 patients with Grade I or II HD treated with a high fibre diet or calcium dobesilate (Week 1: 1 g/day orally; Weeks 2–6: 500 mg/day orally, and 0.5% w/w topically twice daily before and after defecation). Outcomes included both symptom and anoscopic-inflammation scores. In those patients treated with calcium dobesilate, the mean (range) time to symptom relief was 6.5 (2−12) days and approximately 85% of patients achieved a significant reduction in symptoms after 2 weeks. More than 80% of the patients achieved cessation of bleeding and resolution of severe anitis at 6 weeks, as compared to 44% in the diet group. Symptom score and anitis score fell significantly from baseline at 6 weeks (p=0.0002 for both comparisons). In addition, both symptoms and anoscopic inflammation were significantly better in the calcium dobesilate group than in those patients on a high fibre diet alone (p=0.0016 and p=0.0014, respectively).40
MEDICAL MANAGEMENT OF HAEMORRHOIDAL DISEASE WITH CALCIUM DOBESILATE IN PAKISTAN
The burden of HD in Pakistan is difficult to determine. Presentation at medical facilities likely under-represents the true prevalence as treatments by both conventional and non-conventional methods occur outside the clinical environment. Data suggest that 3 days of calcium dobesilate (1.5 g/day) therapy can achieve a 60% reduction in HD symptoms. However, published data from Pakistan are currently lacking.
A study is currently being conducted in two hospitals in Lahore in order to investigate the efficacy of calcium dobesilate in treating HD. The prospective observational study is recruiting adult patients with Grade I or II HD. Patients with recurrent disease, complications such as thrombosed or strangulated haemorrhoids, and those with bleeding disorders are excluded. The primary outcome measure is the mean haemorrhoid symptom score based on the following criteria: pain, discharge, bleeding, pruritus, inflammation, and oedema. Individual symptom scores are assessed on a visual analogue scale. The baseline haemorrhoidal symptom score was noted, and a post-treatment score recorded after 3 days of calcium dobesilate treatment (1.5 g/day).
Based on interim results the majority of patients (N=30) were male (n=24). There was a 54% reduction in symptom score after 3 days, which is in line with expected results. Authors plan to extend the interim results to 300 patients in order to provide country-specific data of calcium dobesilate efficacy in HD disease.
ENDORECTAL ULTRASONOGRAPHY IN HAEMORRHOIDS: A NEW INSIGHT IN AETIOLOGY
Despite an increasingly detailed understanding of the pathophysiology of HD, gaps in knowledge remain regarding the underlying aetiology of the condition. Both defecation and continence rely on the control of the pressure in the AC, however numerous studies using anorectal manometry in both health and disease have left unanswered questions. For example, why do one-third of patients with incontinence maintain a normal anal pressure? Dissonant results led to discussion of whether anorectal manometry represented the correct technique to fully understand the physiology of continence, and if so, whether the correct measurements were being made to properly interrogate anorectal physiology. Anorectal physiology is highly integrated and cannot be adequately studied by focussing on anatomical or physiological factors in a piecemeal fashion. A modern methodological understanding requires a movement towards an integrated theory of coloproctology.
Towards a Mathematical Model of Continence
Despite describing the behaviour of Newtonian fluids, the flow equation has been successfully used by urogynaecologists and vascular surgeons to study the behaviour of non-Newtonian fluids and gain insights into urodynamics and haemodynamics, respectively. Modified for the anorectal system, the flow equation reads thus:
$$Flow~(defecation)~=\frac{intrarectal~pressure}{AC~resistance}$$
In these terms, incontinence can be described as an abnormal flow of gas or bowel contents while a low flow state per unit time describes constipation. The interplay between pressure and resistance described by the flow equation explains why a subset representing approximately one-third of patients with incontinence have normal anal pressure and, conversely, why examples of continent patients with anal prolapse are not uncommon with colorectal clinics.
The main determinants of AC resistance, the length and diameter of the AC, will be well recognised by surgeons. Incontinent patients tend to present with short wide ACs and corrective procedures focus on lengthening and narrowing of the AC. The diameter of the AC is the most important variable as can be recognised in the AC resistance equation where this factor is raised to the power of 4:
$$AC~resistance~=\frac{128 \times dynamic~viscosity~ \big( DV \big) \times AC~length}{3.14 \times \big( AC~diameter \big) ^4}$$
The additional variable represented in the equation, DV, is again intuitively reflected in the clinical practice of providing patients with stool-softening laxatives when constipated and constipating agents in cases of incontinence.
Expanding the flow equation illustrates the increase in pressure, decrease in AC length, increase in AC diameter, and appropriate consistency of faecal matter which is necessary for normal defecation:
$$Flow~ \big( def. \big) ~=~intrarectal~pressure~ \big( IRP \big) \times \frac{3.14 \times \big( AC~diameter \big) ^4}{128 \times DV \times AC~length}$$
These factors can be affected by numerous behavioural and physiological factors including: diet which affects faecal consistency, delayed sensation which increases IRP due to build-up of faecal matter, and coughing which increases the length and decreases the diameter of the AC.
A well-known equation from another field of medicine can be used to gain insight into the effect of pressure on anorectal physiology. The Law of Laplace, which is utilised in both cardiovascular and respiratory physiology, states that the larger the vessel the greater the wall tension required to withstand a given pressure:
$$Wall~tension~ \big( T \big)~=\frac{distending~pressure~ \big( P \big) \times radius~\big( R \big) }{AC~wall~thickness~ \big( \delta \big) }$$
The common variable of radius and diameter (2r) in the Law of Laplace and the Flow equation allows the integration on these two models into a hybrid law of coloproctology:
$$Flow~=~IRP\frac{3.15 \big( T \delta \big) ^4}{8 \times DV \times AC~Length ^4}$$
According to the hybrid law of proctology the AC pressure must drop in order to facilitate defecation, as is known in the literature, in turn the AC wall tension increases as the flow increases during defecation. However, contrary to previous beliefs, the equation indicates that the AC wall thickness must increase during defecation in order to protect the AC against the increasing wall tension and prevent rupture. This increase in AC thickness has since been proved in control subjects using endorectal ultrasonography.41
Anal Canal Wall Thickness and Haemorrhoidal Disease
The relationship between increased wall thickness and defecation led researchers to theorise that there may be a relationship between reduced AC wall thickness and HD. Haemorrhoids may be increasing in size in order to compensate for reduced thickness, eventually resulting in a symptomatic and pathological situation. This proposed lack of wall thickness may be a result of excessive or early straining or a congenital lack of thickness in the AC wall which may predispose to HD.
In order to investigate this theory a prospective cross-sectional study (N=30) was undertaken using endosonography to compare the AC sphincter thickness in patients with HD and controls during rest and push. Fifteen patients presenting at Kasr Al-Aini hospital, Cairo University, Cairo, Egypt, with different degrees of HD and no history of previous anal surgery or concomitant anal disease were enrolled. Controls had no history of anal surgery, painful anal conditions, or anal disease. The whole AC was depicted using two-dimensional (2D) and three-dimensional (3D) imaging following circumferential endosonography carried out at four points, in order to account for the effect of the probe on anal thickness, during both rest and push.
The gender distribution (60% male) was similar in HD and control groups. The majority of the HD patients had Grade III haemorrhoids (60%); the remaining patients were evenly split between Grade II and IV haemorrhoids. Control patients presented with either hernia (60%), goiter (20%), or chronic calculous cholecystitis (20%).
There was no significant difference in the thickness of the internal anal sphincter during rest and push in either the control group or the HD group (Table 2). In the external sphincter, however, there was a significant difference in wall thickness between the rest and push states in the control group, as predicted by the hybrid law of proctology (Table 2). However, there was no significant difference in the thickness of the external sphincter at rest or during push in the HD group (Table 2). Furthermore, there was no significant difference between the internal anal sphincter of HD patients and controls either at rest (2.4 mm versus 2.1 mm, respectively; p=0.071) or during push (2.5 mm versus 2.2 mm, respectively; p=0.175). However, the external anal sphincter was significantly thicker in the HD group compared with the control group at both rest (6.6 mm versus 5.7 mm, respectively; p=0.025) and push (6.9 mm versus 6.2 mm, respectively; p=0.022).
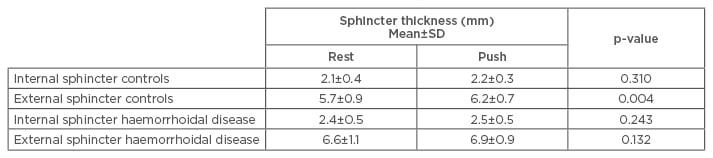
Table 2: Internal and external anal sphincter thickness in haemorrhoidal disease patients and controls during rest and push.
The results suggest a common aetiology for AC problems. High AC wall tension, for example caused by straining against an unrelaxed sphincter, may result in a reflex spasm of anal sphincters which in turn can lead to hypertrophy of the external sphincter muscle. HD can be viewed as a physiological response aimed at protecting the bowel wall against rupture through increasing the size of the anal cushions and, thus, wall thickness. Successful treatment of HD must encompass a behaviour element aimed at achieving normal defecation in response to urgency.41-43
SUMMARY
In summary, HD is associated with bleeding, oedema, pain and/or discomfort. The condition affects 40–50% of the population at one point in their lives and in most countries approximately 4% of the population require surgery. The exclusion of possible malignancy by anorectal endoscopy must be carried out before starting treatment for haemorrhoids with analogous symptoms such as bleeding. Symptoms must be treated, particularly acute bleeding and inflammation of the tissue. Although surgery is necessary for later stages of HD, patients must be saved from unnecessary procedures which are encouraged by some governmental policies such as procedure-related bonuses. Calcium dobesilate is indicated for HD symptoms both in non-surgical cases and pre and post-surgery in order to ‘cool down’ the haemorrhoids before surgery and aid healing afterwards.








