Abstract
The prevalence of non-cardiac chest pain (NCCP) ranges from 13–33%. A majority of those presenting with a chief complaint of chest pain are found to have a diagnosis of NCCP. Aerodigestive diseases are a cause of NCCP, and billions of dollars are spent annually on the treatment of NCCP. Furthermore, NCCP can cause significant psychological stress. NCCP is commonly diagnosed when patients have chest pain despite a normal cardiac evaluation. The leading cause of NCCP is gastro-oesophageal reflux disease (GORD). GORD should be suspected in patients who report a history of acid regurgitation, cough, dysphagia, and bloating. Another common cause of NCCP is obstructive airway disease (OAD). A thorough history and review of the symptoms should be performed for those with suspected NCCP, especially because of the contributing end organs. It is known that environmental exposures can commonly cause GORD and OAD; however, NCCP has not been fully explored in the context of environmental exposure. Patients with a history of exposure to particulate matter can develop environmental-exposure-associated GORD and coexisting OAD. This narrative review aims to provide a practical overview of NCCP, its causes, their relation to environmental exposure, and associated biomarkers. The authors used a PubMed search that spanned 2003–2018 to accomplish this. Additionally, this review provides a broad overview of biomarkers of GORD-associated NCCP and OAD-associated NCCP due to environmental exposure.
INTRODUCTION
Chest pain (CP) accounts for 5.7% of emergency department (ED) visits in the USA each year.1 The differential of CP is broad and often includes acute coronary syndrome, which requires a costly work-up and may lead to inpatient care; however, in one study,2 57% of patients presenting with CP were found to have non-cardiac CP (NCCP). The prevalence of NCCP ranges from 13–33% in subjects complaining of CP.3-6
The treatment of NCCP is a global health concern. In a cohort study of USA veterans, the cost of care of CP patients with a low pretest probability for coronary artery disease was $57,336 per patient.7 Another study showed that the high ratio of NCCP cases to cardiac CP (CCP) cases may cause the cumulative annual cost of NCCP to exceed that of CCP.8 Sick leave and interruptions in work-related activities have been seen in 30–60% of patients with NCCP.9 A recent study found that $13 billion were spent annually on CP treatment, and 50% of CP patients were found to have no evidence of cardiac disease.10
NCCP was defined as recurring CP that cannot be differentiated from CCP and has a negative evaluation for cardiac causes.11 Differentiating acute coronary syndrome from NCCP involves the assessment of serum levels of cardiac biomarkers, such as troponin and creatinine-kinase-muscle brain levels; electrocardiography; chest X-ray; and lipid profile.12
Studies have shown that the most common cause of NCCP is gastro-oesophageal reflux disease (GORD). In a 2007 study of 78 patients with NCCP, the prevalence of GORD was 44.8%.13 Additionally, of the 35 patients who had GORD-induced NCCP, 57.1% and 48.6% reported heartburn (HB) and regurgitation, respectively.13 Another cause of NCCP is obstructive airway disease (OAD), with nearly half of patients with OAD reporting CP.14 In addition to OAD and GORD, anxiety has been studied as a contributor to NCCP, with NCCP patients exhibiting higher State Trait Anxiety Inventory scores than controls in a 2014 study.15
OAD and GORD are prevalent in those with a history of occupational or environmental exposure.16-20 In firefighters with World Trade Center (WTC) particulate matter (PM) exposure, there was a significant increase in the prevalence of GORD from 38.4% to 43.8% in the cohort 4 years after the 11th September 2001 terrorist attack at the WTC (9/11).21 Additionally, the biomarker profile of patients with GORD and OAD secondary to PM exposure has been explored by our group and others and may provide insight into contributing pathways.22-40
This review presents an overview of NCCP, its unique features with respect to CCP, the causative role of environmental exposures, and the biomarkers of GORD and OAD, two conditions caused by environmental exposure that can lead to NCCP.
METHODS
Search Strategy
PubMed databases were searched on 28th June 2018. The search was limited to articles that were published within the last 15 years, from 1st January 2003–28th June 2018. Cohort studies, case control studies, narrative reviews, meta-analyses, and statistical summaries were retrieved. Titles, abstracts, and full texts were screened based on relevance to this review. Keywords searched included ‘non-cardiac chest pain’, ‘gastroesophageal reflux disease’, ‘obstructive airway disease’, ‘air pollution’, ‘particulate matter’, ‘occupational exposure’, ‘World Trade Center’, ‘chronic obstructive pulmonary disease’, ‘chest pain’, ‘predictive biomarkers’, ‘low risk chest pain’, ‘HEART Score’, and ‘emergency department summary’. Furthermore, the references of many of the articles identified by the above search strategy were reviewed.
Inclusion and Exclusion Criteria
Studies were included in this narrative review if they were observational, retrospective, systematic reviews, or clinical studies; focussed on providing the epidemiology and aetiology of NCCP; assessed the relation of NCCP with OAD and GORD; discussed OAD and GORD in the context of environmental exposure; or focussed on the use of biomarkers to evaluate environmental-associated causes of NCCP. Studies were excluded if they were published earlier than 2003, were not written in English, or were not conducted on human subjects. Studies that were included in this review were available in their entirety online and were referenced using EndNote® X7 (Thomson Reuters, Philadelphia, Pennsylvania, USA).
RESULTS AND DISCUSSION
Differentiating Non-Cardiac Chest Pain from Cardiac Chest Pain
Several recent studies have attempted to identify low-cost methods of differentiating NCCP and CCP. In a cohort of 331 patients who experienced an acute myocardial infarction, 90% of those reported CP >20 minutes in duration.41 CCP is located proximally, while NCCP localises to the middle-left side of the chest. The same study found that patients with NCCP took medications for CP relief at a lower rate than their CCP counterparts.42
Decision-Making Tools and Scoring Systems That Have Recently Been Used to Risk-Stratify Chest Pain Patients
The HEART Score uses history, ECG findings, age, risk factors, and troponin levels to risk-stratify patients, and has been shown to be able to be used to safely discharge low-risk CP patients from the ED at a higher rate than clinician judgement alone.43 In a 2017 prospective cohort study, use of the HEART pathway, which incorporated the HEART score, resulted in $904,952 in-hospital costs saved over 1 year.44 The North American Chest Pain Rule (NACPR) considers new ischaemic ECG changes, a history of coronary artery disease, the Diamond-Forrester Classification, and troponin levels >99th percentile. If a patient does not meet any of these four criteria, then additional diagnostic studies are not necessary and the patient can be discharged from the ED. In a 2017 cohort study,45 none of those classified by NACPR as very low risk experienced complications 30 days after discharge.
Recent Serum Biomarkers for Differentiating Types of Chest Pain
Along with clinical decision-making tools, serum biomarkers have also been used in the stratification of CP patients. A 2017 study demonstrated that 97% of a subset of low-risk CP patients with normal levels of cystatin C and N-terminal pro-B type natriuretic peptide had normal stress ECG.46 Further studies assessing the effectiveness of using these biomarkers in low-risk CP patients are warranted.
Differential Diagnosis of Non-Cardiac Chest Pain
NCCP has a broad differential, including pulmonary, gastrointestinal, and musculoskeletal causes (Figure 1). The authors will focus on two of the most common causes of environment-associated NCCP: GORD and OAD, highlighted yellow in Figure 1. GORD is the main contributing factor in up to 50% of patients with CP.47 Multiple studies have supported GORD’s association with NCCP.48-51 GORD is also often found in OAD patients.52
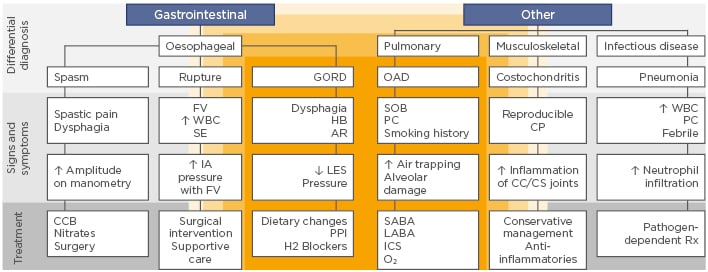
Figure 1: Overview of the differential diagnosis and treatment of chest pain.
PM-associated conditions highlighted in yellow.
↑: increased; ↓: decreased; AR: acid regurgitation; CC: costochondral; CCB: calcium channel blocker; CP: chest pain; CS: costosternal; FV: forceful vomiting; GORD: gastro-oesophageal reflux disease; H2: histamine receptor 2; HB: heartburn; IA: intra-abdominal; ICS: inhaled corticosteroids; LABA: long-acting beta-agonist; LES: lower oesophageal sphincter; OAD: obstructive airway disease; PC: productive cough; PPI: proton pump inhibitor; Rx: treatment; SABA: short-acting beta-agonist; SOB: shortness of breath; SE: subcutaneous emphysema; WBC: white blood cells.
Gastro-Oesophageal Reflux Disease as a Cause of Non-Cardiac Chest Pain
The underlying mechanism of GORD-related NCCP is still an area of active investigation. Oesophageal distension and hypersensitivity have been identified as possible aetiologies. In one case-control study,53 ultrasound imaging demonstrated that patients undergoing a GORD episode had higher cross-sectional area of the oesophagus than controls. Oesophageal hypersensitivity as a cause of NCCP has also been postulated; acid infusion in the distal oesophagus resulted in the lowering of the oesophageal pain threshold in both NCCP and healthy patients.54 Reflux episode duration and acid clearance have been shown to contribute to NCCP.55 A 24-hour ambulatory pH assessment was used to monitor reflux episodes in 120 subjects. Those who reported CP experienced both longer reflux episodes and acid clearance times.55
Gastro-Oesophageal Reflux Disease due to Environmental Exposure
Although there are established risk factors, such as socioeconomic status, obesity, and cigarette smoking, that contribute to the pathogenesis of GORD,56,57 the effect of PM exposure remains an important topic. Studies of environmental exposure and GORD have identified a positive association between the two. In a longitudinal study of Fire Department of New York (FDNY) firefighters, it was determined that GORD was the condition with the highest incidence after 9/11, followed by OAD and chronic rhinosinusitis.16 It was suggested that aerodigestive tract inflammation contributed to the development of GORD.16 In a 2011 retrospective study of WTC-PM-exposed subjects, the incidence of symptoms related to GORD after 9/11 was 20.3%. Two-thirds of those affected still had persistent symptoms up to at least 6 years after the attacks.17
A 2015 clinical study18 showed that patients who had a history of inhalational injury due to sulfur mustard exposure had higher frequencies of GORD symptoms than controls. In a sample size of 120 patients who were exposed to sulfur mustard, acid regurgitation and HB were reported at frequencies of 40.8% and 51.7%, respectively; this was a significantly higher percentage than the control group, in which 6.7% and 8.8% of participants were affected by acid regurgitation and HB, respectively. A study reported that, out of 1,650 subjects who completed an occupational exposure survey, the subset of 224 subjects further classified with a complication of GORD known as Barret’s oesophagus (BO), reported higher self-reported asbestos exposure frequencies than the controls.58
Obstructive Airway Disease as a Cause of Non-Cardiac Chest Pain
There are several potential mechanisms that contribute to OAD patients experiencing thoracic pain. The activation of the visceral pleura receptors has been implicated. Hyperinflation of the lungs seen in chronic obstructive pulmonary disease (COPD) patients causes the visceral pleura to stretch and, as a result, activate the visceral pleura receptors that are connected to the pulmonary parenchyma, leading to pain.59 The intercostal nerves that transmit nociceptive information through the intercostal nerves to the central nervous system have also been suggested as a cause of chronic CP in COPD patients.59 In a 2016 cross-sectional observational study,60 67 patients with OAD were interviewed about the severity and location of their pain, and underwent spirometry and plethysmography. Thoracic pain was reported in 53.7%, in either an isolated pattern or accompanied with pain in another area. Despite the high prevalence of thoracic pain in this study, there were no significant correlations between thoracic pain, hyperinflation, and pulmonary function test data.
Obstructive Airway Disease and Environmental Exposure
In a cross-sectional study conducted in 2017,19 seven district clusters were randomly selected from four Chinese cities with different pollution levels. PM concentrations for each cluster were measured and subjects underwent spirometry. From the data, it was suggested that subjects from areas that had higher concentrations of PM were more prone to obstructive symptoms such as cough, dyspnoea, and wheezing; however, in this study, the effect of PM on COPD was not statistically significant in non-smokers.
In WTC-PM-exposed FDNY rescue workers referred for pulmonary evaluation, 59% of the cohort had indications of OAD, such as elevated residual volume, airway hyper-reactivity, and bronchodilator responsiveness.40 In a 2010 cohort study, significant declines in forced expiratory volume in 1 second (FEV1) were seen in a cohort of firefighters and emergency medical service workers who responded to the WTC terrorist attacks.61 The incidence of those with FEV1 less than the lower limit of normal (LLN) increased in the 6 years after 9/11.61
In a longitudinal study that spanned 20 years, 3,343 people between the ages of 20 and 44 years underwent a detailed questionnaire, spirometry, and occupational assessment. Subjects with COPD or asthma at baseline were excluded. Subjects provided details regarding their occupation and their responses were coded by the International Standard Classification of Occupations (ISCO). These codes were then linked to the ALOHA Job-Exposure Matrix that assigned grades of no, low, or high exposure to various agents for every job code. It was demonstrated that those who were exposed to toxins had a higher incidence of COPD.20
The pathophysiologic and cellular response contributions of PM-exposure to OAD are under investigation. In a systematic review, it was argued that a wide array of proteins that signal a downstream effect of inflammation and oxidative stress can contribute to the pathogenesis of OAD secondary to PM exposure.62 PM exposure of alveolar macrophages and pulmonary epithelial cells led to the release of proinflammatory mediators, such as granulocyte-monocyte colony stimulating factor (GM-CSF), TNF-α, IL-1, IL-8, and IL-6, that facilitate the recruitment of neutrophils and other leukocytes to mediate lung tissue damage.63
Serum Biomarkers of Particulate Matter-Associated Morbidity and Associated Non-Cardiac Chest Pain Conditions
Studies concerning the use of serum biomarkers to assist in the diagnosis, monitoring, and understanding of PM-associated GORD and OAD pathogenesis have been conducted (Table 1).22-27,29-31,33,35-39,64,65
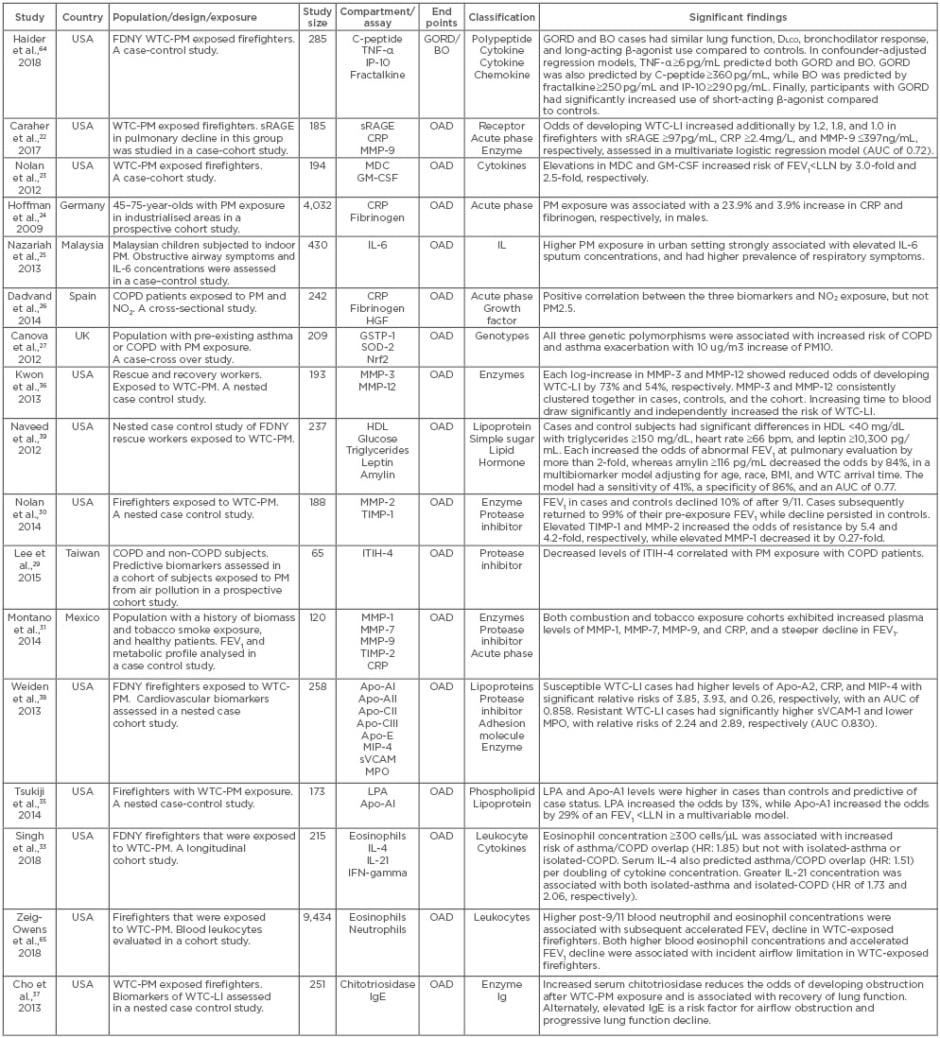
Table 1: Biomarkers of non-cardiac chest pain due to environmental exposure.
Apo: apolipoprotein; AUC: area under the curve; BO: Barrett’s oesophagus; COPD: chronic obstructive pulmonary disease; CRP: C-reactive protein; DLCO: diffusing capacity of the lung for carbon monoxide; FDNY: Fire Department of New York; FEV1: forced expiratory volume in 1 second; GORD: gastro-oesophageal reflux disease; GM-CSF: granulocyte-monocyte colony stimulating factor; GSTP-1: glutathione S-transferase 1; HDL: high density lipoprotein; HGF: hepatocyte growth factor; HR: hazard ratio; IP-10: interferon-gamma inducing protein 10; ITIH-4: inter-alpha-trypsin inhibitor 4; LPA: lysophosphatidic acid; LLN: lower limit of normal; MDC: macrophage-derived chemokine; MIP-4: macrophage inflammatory protein-4; MMP: matrix metalloproteinase; MPO: myeloperoxidase; Nrf2: nuclear factor 2; OAD: obstructive airway disease; PM: particulate matter; SOD2: superoxide dismutase 2; sRAGE: soluble receptor for advanced glycation end-products; sVCAM: soluble vascular cell adhesion molecule-1; TIMP: tissue inhibitor of metalloproteinase; WTC-LI: World Trade Center lung injury; WTC-PM: World Trade Center particulate matter.
Known for its pathophysiologic contributions to cancer, metabolic syndrome, and other conditions, the soluble receptor for advanced glycation end-products has been highly associated with cases of WTC lung injury (WTC-LI), defined as percent FEV1 of predicted normal (FEV1%Pred) <LLN, relative to controls.22 Macrophage-derived chemokine and GM-CSF have been associated with a FEV1%Pred<LLN in firefighters exposed to WTC-PM.23 Metabolic biomarkers, such as glucose, triglycerides, and lipoproteins, can be used to assess pulmonary function loss. In a 2012 nested case control study,39 elevated glucose and leptin levels were predictive of the development of WTC-LI. In cases of WTC-LI, there was also a higher prevalence of individuals with characteristics of metabolic syndrome.39 It has been demonstrated that certain biomarkers could exert a protective effect against OAD. Elevated levels of matrix-metalloproteinase (MMP)-2 and tissue inhibitor of MMP-1, were associated with increased resistance to WTC-LI.30 MMP-3 and MMP-12 were also found to exert a protective effect from developing WTC-LI in a cohort of FDNY firefighters.36
In a 2009 study,24 PM exposure was associated with a 23.9% and 3.9% increase of C-reactive protein and fibrinogen, respectively, in a cohort of individuals from highly industrialised areas in Germany. In a 2013 study,25 high PM exposure was not only associated with increased reporting of obstructive airway symptoms relative to low PM exposure but also was strongly associated with higher sputum IL-6 concentrations. In a cohort of 251 COPD patients, C-reactive protein, hepatocyte growth factor, and fibrinogen were strongly associated with nitrate dioxide exposure in a 2014 study conducted in Spain.26 Genomic biomarkers have also been used to establish incidence of exposure. Glutathione S-transferase 1, superoxide dismutase 2, and nuclear factor 2 were associated with a slight risk for hospitalisation due to COPD and asthma exacerbation secondary to PM exposure.27
Decreased levels of inter-alpha-trypsin inhibitor-4 have been associated with PM exposure in a cohort of PM-exposed subjects in Taiwan.29 Specifically, levels of inter-alpha-trypsin inhibitor-4 were significantly lower in patients with OAD than healthy subjects regardless of their smoking status, up to 3-years post exposure. Increased levels of MMP-1, 7, 9, and tissue inhibitor of MMP-1 were seen in a cohort of COPD patients with biomass exposure and were associated with a significantly lower FEV1 relative to the controls and those with COPD secondary to tobacco smoke exposure.31
Biomarkers of Gastro-Oesophageal Reflux Disease
As with studies of OAD patients, serum biomarkers were also used to establish incidence of GORD secondary to PM exposure. In a 15-year longitudinal study published in 2018,64 biomarkers were identified in a sub-cohort of WTC-PM-exposed FDNY firefighters. A sample of 265 FDNY rescue workers exhibited elevated levels of three serum biomarkers; TNF-α, C-peptide, and MMP-9 were found to be significant predictors of developing GORD secondary to PM exposure.
Expressions of claudin-1 and 2, zonula occludens-1, and filaggrin were found to be changed in those with GORD, as discussed in a 2016 systematic review.66 The same review demonstrated that not only was proteinase-activated receptor-2 (PAR-2) overexpressed in GORD patients but PAR-2 also contributes to the pathogenesis of GORD in the context of visceral hypersensitivity.65 It has been argued that the activation of PAR-2 gives rise to the release of IL-8, causing inflammatory changes and subsequent GORD.67
Biomarkers of Barrett’s Oesophagus
The use of metabolite profiles in patients with BO, a complication of GORD, has been studied. It was shown that creatinine and homocysteine were shown to be differentially expressed in patients with BO relative to those who had GORD; however, the multivariate model was associated with a lower receiver operator characteristic area under the curve.68 Urinary metabolomics also revealed differences between healthy patients and those with BO. Eight metabolites were shown to have significantly different urinary concentrations between the BO and healthy patients, with sucrose and cis-aconitate showing the most significant differences among the two groups in regard to fold changes.69 In WTC-PM-exposed firefighters, TNF-α, IFN-γ, induced protein-10, IL-6, and insulin, when elevated, were strongly associated with BO.64 Further research is needed to continue to characterise the biomarker profile of GORD.
FURTHER NEED FOR RESEARCH
Although there are studies that demonstrate work-related risk factors of GORD,70,71 the environment’s role in GORD pathogenesis has been a neglected topic and PM-induced GORD is poorly understood. Conducting further studies on the prevalence of GORD in subjects who have been exposed to high PM concentrations or are in highly polluted areas can widen the evidence that environmental exposure is an independent risk factor for GORD.
The authors’ lab is currently studying the effect of dietary intervention on WTC-PM-exposed FDNY firefighters to determine its potential therapeutic effect on parameters such as FEV1, fractional exhaled nitric oxide, and the metabolomic profile of those affected with WTC-associated lung disease, and whether these interventions can reduce the incidence of these conditions.
CONCLUSION
NCCP remains a highly prevalent complaint. With its financial cost, NCCP is an individual and societal burden. Despite the commonality and multifactorial nature of NCCP, the underlying mechanism of NCCP in the setting of PM exposure remains unexplained. The environment’s role in the development of GORD and OAD is a dynamic topic that requires further research. Establishing a pathophysiologic basis of environmental exposure-associated NCCP may facilitate treatment and prevention.







