Abstract
The COVID-19 pandemic has overwhelmed the already limited healthcare systems of low resource Asian countries. It has had a profound impact on inflammatory bowel disease (IBD) patient care in this region, where the disease is emerging. Fear of increased risk of COVID-19 due to disease or drugs, lack of access to medications, laboratory testing, endoscopy, surgery, infusion centres, and even remote medical consultation have made the lives of patients with IBD in this region more difficult than before. Similarly, physicians faced challenges due to limited testing facilities and therapeutic armamentarium for IBD management in the face of the COVID-19 pandemic. There was also the fear of potential spread of COVID-19 during colonoscopy or physical consultation, with the shortage of protective equipment, and unfamiliarity with teleconsultation and the remote monitoring of IBD. Most of the healthcare systems in these countries faced similar challenges in disease containment and management due to overwhelmed healthcare facilities in the face of crisis, inadequate vaccination drive in highly populous regions, and the unequal distribution of healthcare facilities centred in urban areas. COVID-19-specific safety norms, proper psychological support, and IBD-focused COVID-19 information can help alleviate patient concerns. Widespread adaptation of telemedicine, being up to date with current evidence, and performing endoscopy in high-priority cases, with precautions, can help physicians treat patients with IBD optimally. Additionally, the restructuring of the public health system, widespread vaccine rollout, and, ultimately, containment of the pandemic, can improve healthcare outcomes of patients with IBD in low resource countries.
Key Points
1. Healthcare in low resource countries in Asia has been overwhelmed due to the COVID-19 pandemic, particularly with regard to the emerging disease of inflammatory bowel disease (IBD).2. Both patients with IBD and physicians treating the disease have faced myriad challenges, from lack of access to medications and limited testing facilities, to the fear of COVID-19 spreading during in-person consultations.
3. In this article, the authors propose many solutions to alleviate healthcare for patients with IBD during the pandemic, including widening the use of telemedicine and prioritising management guidelines for this patient group.
INTRODUCTION
Since the declaration of the COVID-19 pandemic on 11th March 2020, the disease has barrelled across 222 countries, infecting nearly 1.5 billion people. The spread continues unabated.1 The rapidly increasing demand for health facilities and healthcare workers has had a huge impact and has overstretched the global healthcare systems in even the most developed of nations.2
In this scenario, management of patients with chronic lifelong diseases such as inflammatory bowel disease (IBD) requires special considerations.3 These patients are often malnourished and immunocompromised, and, therefore, are at high risk of COVID-19 infection. The medication protocol may need to be modified, ensuring disease control, and avoiding steroids in particular, which could be associated with a poor prognosis.4 Additionally, there are issues of hospital visits for follow-ups or infusions, performance of elective procedures and surgeries, and allaying the fears and anxieties of patients.5 These are global concerns as the pandemic continues, and second and third waves of infections are being reported.
There are unique challenges in IBD management in the developing world, which are quite distinct from those in developed countries.6 These range from the perspectives of patients regarding access to care and affordability of drugs during lockdowns, to the physician’s perspective of diagnostic dilemmas due to high prevalence of other infectious febrile illnesses. The rural and primary healthcare network of these low resource countries is ill-equipped to deal with IBD with limited resources, management facilities, or physician awareness.
This review attempts to analyse the various challenges in the management of IBD amidst the pandemic in limited resource settings, the possible change in standard practices warranted, and future strategies to optimise therapy more suited to the region. For the purpose of the review, the authors considered low- and middle-income countries in Asia (Figure 1) based on World Bank classification as resource-limited countries, as they face similar challenges.7 The authors interviewed IBD specialists from these countries for their opinions and conducted a questionnaire-based survey of patients for the purpose of this review, since precise published data is limited.
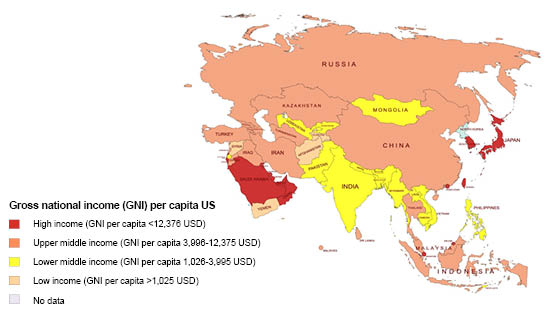
Figure 1: Gross national income per capita in Asian countries according to World Bank.7
THE IMPACT OF THE PANDEMIC ON INFLAMMATORY BOWEL DISEASE MANAGEMENT HAS BOTH PATIENT AND PHYSICIAN PERSPECTIVES
The Patient Perspective
The fear of increased risk of COVID-19 infection
The fear of contracting COVID-19 in patients with IBD is exacerbated by the general perception that IBD and its immunosuppressive therapies predispose an increased risk of contracting infection. Hence, most patients are afraid of visiting the hospital or IBD centre to consult a gastroenterologist. There is a lack of IBD management information for during the pandemic for the average patient, mainly due to the paucity of teleconsultation facilities and group awareness sessions.8 The majority of hospitals in India saw a drop in outpatient numbers by more than 50% for many months, and routine follow-ups also dropped by nearly 60%.9 Endoscopy units in India were performing at less than 10% of their usual volume during April 2020.10 Most teleconsultations did not focus on information and allaying of fears due to lack of adequate training in telemedicine (Figure 2).11,12
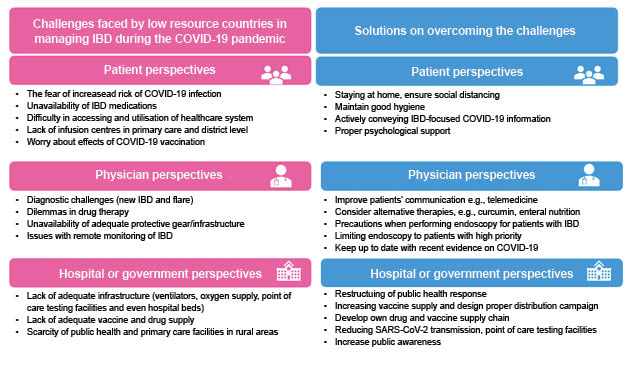
Figure 2: Summary of the challenges faced in low resource countries in Asia and proposed strategies to overcome them.
IBD: inflammatory bowel disease; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2.
This trend has been noted across the world. In fact, a 50% drop in emergency department visits was reported in the USA.13 In a global survey of 3,815 patients from 51 countries in Europe, America, Australia, Africa, and Asia, 85% of respondents feared developing the COVID-19 infection.5 About one-third of patients believed that IBD predisposes them to an increased risk of contracting COVID-19 infection. Eighty-seven per cent of patients were afraid to travel, and more than 70% were afraid to visit hospitals or IBD centres. Surprisingly a physician consultation did not help, and alleviated worries in only 11.1% of cases. Patient association and support groups were the most helpful (82.5%), but these are not available in the majority of low resource countries.5
Online consultation and telemedicine have become the norm in many countries. In a study from China, only 13% of patients with IBD visited hospitals, or emergency departments in non-COVID-19 hospitals, while 50% had online consultations with their physicians. Scheduled follow-ups were impacted in up to 70% of cases due to the pandemic.14
In Wuhan, China, the epicentre of COVID-19, all 318 patients with IBD from a regional IBD centre only sought medical care, or contacted doctors and pharmacies online after receiving educational and instructional information from the regional IBD centre through mobile messages and WeChat (Tencent Holdings Ltd., Shenzhen, China).15
However, telemedicine and online consultations are not readily available in resource-limited countries. The internet penetration rate in India, with a relatively better economy, was still 45% in 2020.16 The availability is likely to be worse in other countries, and is less than 20% in Bangladesh.17
Apart from limited internet facilities, network coverage, the unavailability of regulatory frameworks for data protection, a lack of information technology training, accessibility, and affordability are issues that need to be resolved.18-20 Another hurdle for widespread implementation of telemedicine in developing countries is the cultural resistance, as it is hard for patients to believe that they can receive healthcare without an in-person physician visit.21 The lack of widespread availability and/or acceptability of telemedicine pose specific challenges to IBD management in these regions.
Unavailability of drugs
Shortage of drug supply, high cost and/or side effects of therapy, and a lack of universal health insurance have affected access to medications for patients with IBD during the pandemic.22 Nearly two-thirds of patients with IBD had the perception that immunosuppressive IBD medications predispose them to COVID-19 infection. Despite this, only a small proportion actually stop their medications (4%).5 The national Chinese Society of Gastroenterology (CSG) did recommend the temporary cessation of biologics and immunosuppressants in the initial phase of the COVID-19 outbreak.15 In a digital survey from India, 46% of patients reported difficulty in availability of immunomodulators and biologics. Availability was better in urban areas (64%) compared with rural areas (37%), although not statistically significant.8 In the authors’ experience, nearly 4% stopped their IBD medications mainly due to the fear of getting COVID-19 infection, unavailability, a switch to alternative medicines, or awaiting a doctor’s approval pending consultation. Of the authors’ patients on biologics, 12% missed their scheduled dose due to the inability to visit the infusion centre during lockdown, and the unavailability of local infusion centres with expertise. The lack of infusion centres or trained primary physicians or nurses with regard to biologic infusion in districts and primary care settings was the reason why the majority of patients missed their scheduled biologics, which can lead to disease flare.23-25
The unavailability of drugs is another issue inherent to resource-limited countries. The lockdown policy has made it difficult for patients to visit medical clinics or hospitals for drugs. There has been a disruption of many drug supply chains, and the import and export of pharmaceuticals. For example, India depends on China for around 70% of the active pharmaceutical ingredients that it uses in pharmaceutical manufacturing.26 On the other hand, Myanmar depends on India for supplies of mesalamine (Table 1). If the pandemic continues long-term, this may drastically affect drug availability in many countries in the developing world, who depend on others for drug supply. This is likely to increase the cost of medications, resulting in patients discontinuing therapy, and becoming inclined to switch to often unproven complementary and alternative medications, more so in resource limited settings.27 Moreover, unscrupulous faith healers are commonplace in this region.28 Loss of pay or employment due to economic crisis, mental stress due to COVID-19-related mortality, and paranoia around media coverage further complicates the situation.
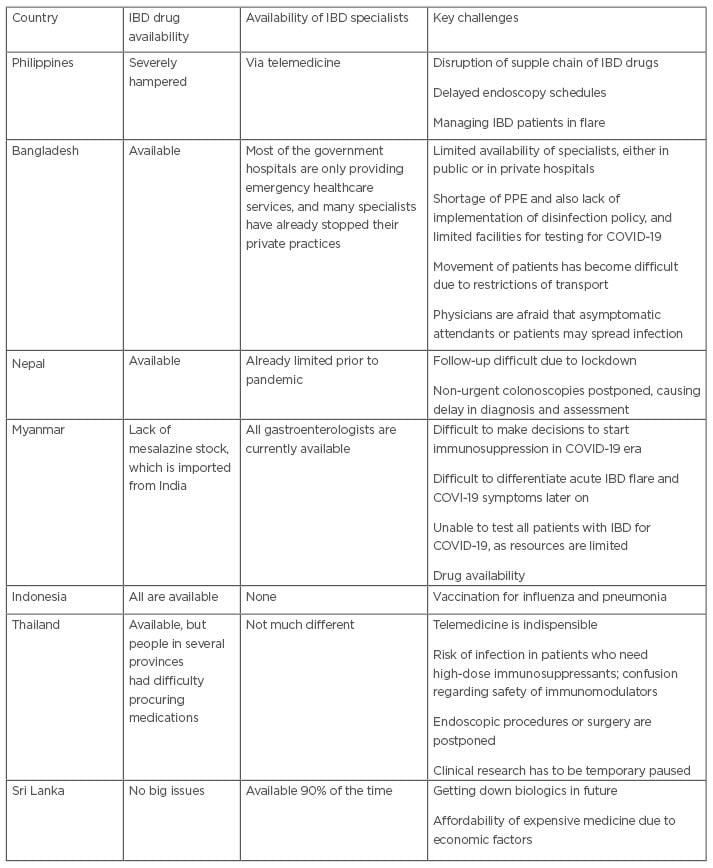
Table 1: Survey of inflammatory bowel disease specialists about challenges faced during the COVID-19 pandemic in resource-limited settings.
IBD: inflammatory bowel disease; PPE: personal protection equipment.
Difficulty in accessing and utilising healthcare systems
Poor access to healthcare is a key factor contributing to sub-optimal disease outcomes in patients with IBD in resource-limited settings. It is well understood that there is an unequal distribution of healthcare systems, with gross disparity between rural and urban settings in this entire region.27
The COVID-19 outbreak has highlighted these limitations. IBD management has been centred around urban tertiary care centres, with patients travelling to cities for adequate care. With continuing lockdowns and travel restrictions, including the risks of public transport such as buses and trains, this has not been possible. This has resulted in patients having no option but the local health centre. Diagnostic tests, including colonoscopies, are not available in the majority of rural settings.27 Also, there is poor awareness and understanding about IBD in primary healthcare centres.
The authors found, as a part of our teleconsultation experience, that patients missed their biologic doses because the local physician was uncertain on the mode of administration and risks, as well as a lack of confidence on the part of the patients. In our survey, more than one-third of the patients could not consult a doctor in person or online.
In a survey of IBD physicians, a respondent from Pakistan reported that the fear and stigma of testing positive for the severe acute respiratory syndrome coronavirus 2 infection inhibited patients from accessing medical care.29 Family and community pressure to consult with faith healers, lack of social support or patient support groups, high cost of medications, and no universal health insurance are challenges patients with IBD face in day-to-day life in resource-limited settings, according to a patient survey from South Asia.28 The COVID-19 pandemic has complicated these issues even further, with a lack of proper information and guidance, with patients stopping medications such as steroids and biologics, and taking herbal or other alternative therapies thought to be safer.24 In the authors’ survey, they found that more than a quarter of patients with IBD use complementary and alternative medications, the most common reason being perception of safety.30
Physician Factors
New diagnosis of inflammatory bowel disease
Current recommendations for new diagnosis of IBD during the ongoing pandemic suggests a higher threshold for endoscopy in patients presenting with abdominal pain and altered bowel habit, and carefully ruling out gastrointestinal manifestations of COVID-19 infection, infectious causes of diarrhoea, and irritable bowel syndrome by throat swab testing, stool culture or toxin assay, and stool biomarker (faecal calprotectin), respectively.31 The International Organization For the Study of Inflammatory Bowel Disease (IOIBD) expert list of recommendations considers new diagnosis of IBD as a high priority for endoscopy, even during the pandemic.32
However, such recommendations may not be practical in resource-limited countries. The lack of COVID-19 testing facilities; adequate colonoscopy services, particularly in rural hospitals; or widespread availability of calprotectin assay poses difficulties. Patients are unable to travel to higher centres with adequate diagnostic facilities due to lockdown restrictions.22 In an international survey of IBD physicians, including the IBD-Emerging Nations’ Consortium (IBD-ENC) region consisting of the low resource countries of Asia, show that some centres were avoiding endoscopy, even in newly-diagnosed patients, and a few treated cases of likely colitis with empirical 5-amino salicylic acid (5-ASA) therapy.29
Dilemmas in drug therapy
Immunosuppressive drugs have been associated with an increased risk of opportunistic viral infections, and, as such, physicians have been concerned of their usage during the pandemic.33 In a questionnaire-based survey of 813 physicians from 72 countries, more than two-thirds of the physicians believed that IBD drugs are associated with increased risk of COVID-19. In fact, 10% of the physicians stopped IBD drugs as a preventative measure (highest: thiopurines -72.7%; followed by steroids: -43.6%).5 This has important clinical implications on treating those who cannot afford treatment. Stopping azathioprine, a low-cost therapy, may lead to severe flares requiring steroids that are even more harmful, or high-cost biologics, which most would not be able to afford. Biologic therapy, however, is considered to be relatively safe and not associated with adverse outcomes in patients with COVID-19, while systemic corticosteroid was associated with a nearly seven-fold higher risk of developing severe COVID-19 infection.4 However, cost, unavailability, and the high risk of latent tuberculosis in resource-limited settings precluded its widespread use.34 These dilemmas between risk and benefit of therapy are unique in low resource settings, and should be balanced on individual basis (Table 1).27
The Surveillance Epidemiology of Coronavirus Under Research Exclusion (SECURE)-IBD data also suggests increased risk of severe COVID-19 with mesalamine; more so if associated with anti-TNF therapy. Although this uncontrolled observational data has limitations, the current therapeutic armamentarium to combat IBD is limited in resource-limited countries.35
Diagnosis and treatment of flare
For diagnosis of IBD flare, guidelines recommend initially non-invasive measures such as faecal calprotectin measurement, followed by drug level monitoring, failing which endoscopy can be considered.36 Moreover, all patients with IBD presenting with diarrhoea are recommended to test for COVID-19 infection to discriminate true IBD flare from diarrhoea due to COVID-19, as at least 5% of patients present with isolated gastrointestinal symptoms.37 However, these facilities are often not available in resource-limited settings.
Surgeries for IBD have also been delayed due to fear of contamination of intensive care units and operating theatres. Setting up a network of COVID-19-free hospitals, with dedicated IBD physicians and surgeons, and co-operation with other centres in the region, can allow prompt management of patients with IBD with severe flare, and can improve outcomes.38
Availability of protective gear and infrastructure
Colonoscopy is the diagnostic procedure of choice in IBD. The Asian-Pacific Society for Digestive Endoscopy (APSDE) recommends that the entire endoscopy and colonoscopy staff team should wear full personal protective equipment (PPE).39 However, given the worldwide shortage of PPE, this is impossible, especially in resource-limited countries.40 Countries such as India have started manufacture their own PPE to meet the shortage, but still more manufacturing machines are needed to reduce the supply and demand gap.41,42 The Centers for Disease Control and Prevention (CDC) has issued a guidance on the extended use of N95 respirators in order to conserve resources.43 Perhaps this should also be considered in order to conserve resources to protect healthcare workers in resource-limited settings.
In a worldwide survey of IBD physicians, respondents from Bangladesh and Thailand reported a lack of PPE supply, and a discrepancy between private and public hospitals for availability was reported in Brazil.29
To add to this problem, there are shortages of equipment and infrastructure (shortage of intensive care units, ventilators, oxygen supply, and critical care personnel) to manage COVID-19 patients with IBD, a lack of critical care specialists, and a lack of awareness of IBD in community physicians.44 Managing the combination of IBD and COVID-19 in this pandemic is a major challenge in low resource countries.
Issues with remote monitoring of inflammatory bowel disease
Telemedicine has emerged as an important resource in the management of patients with IBD during the COVID-19 pandemic, particularly in remote regions.45 However, it is a difficult proposition in resource-limited settings where the internet is not widely available, and many physicians are still not digital-friendly. Moreover, few physicians are concerned about a hindrance to direct clinical decision-making, loss of relationship and trust with the patient, and the vulnerability of digital record maintenance.46 As a consequence, resource-limited settings are still seeing sizeable in-person outpatient clinic walk-ins, though reduced from normal numbers, in Indonesia, Myanmar and Vietnam, compared with New Zealand, Canada, the UK, Qatar, and the USA, where the outpatient departments were effectively closed.29
Barriers to vaccination
The uptake of recommended vaccines amongst patients with IBD have been sub-optimal historically. Vaccine distribution across the general population in resource-limited settings may have inordinate delays. India vaccinated less than 2% of its population earlier in 2021, which has now improved, with 70% of the population receiving at least one dose of a COVID-19 vaccine.44 Hence, an increase in vaccine supply and a distribution campaign are warranted to cover both urban and rural areas.44 The cost of vaccination should be kept under control so that vaccines can reach poorer communities. Proper storage facilities are warranted to maintain the vaccine cold chain, which is essential for vaccine efficacy. In view of the immunocompromised state of many patients with IBD, priority status should be given for vaccination. Since the mortality of COVID-19 infection increases exponentially with age, vaccination strategy is largely based on age in many countries, where older people (>60–65 years) are often given priority. IBD is an underlying health condition that puts patients at higher risk of serious disease and mortality; hence, vaccination should be prioritised in patients with IBD aged between 16–64 years.47
There are concerns among patients with IBD and physicians regarding the safety and long-term effects of COVID-19 vaccination in IBD. Perceived risk of increased adverse events, interaction between IBD medications and vaccine, scepticism about long-term safety, and lack of typical scrutiny for COVID-19 vaccination are barriers to vaccination in patients with IBD.48,49 However, the risk of adverse event to COVID-19 vaccination in patients with IBD is very low, and similar to that of general population. However, patients with IBD on immunomodulators can have sub-optimal antibody responses to vaccination, especially after a single dose of vaccine. Two vaccine doses lead to seroconversion in most patients. Delayed second dosing of vaccinations should be avoided, especially in patients receiving infliximab.50 Hence, dissemination of proper information to patients with IBD, all IBD care providers, practicing physicians, gastroenterologists, and local government authorities are required to improve vaccination drive in this subgroup of patients.
Perspectives on How to Overcome, and the Way Forward
The effect of the COVID-19 pandemic in the resource-limited settings of Asia (Figure 2) is less commonly recognised.22 There are unique challenges and obstacles to implement global guidelines.
Widespread implementation of telemedicine in resource-limited settings is difficult, given that only a limited number of patients could use this service. Lack of universal access to the internet and smartphone facilities has reduced the impact of telemedicine in these regions. In spite of the obstacles, digital and telephonic remote consultation technology has been used like never before for follow-up of patients with IBD during the pandemic. The Government of India (GoI) have legalised teleconsultation during the pandemic. They also introduced the eSanjeevani telemedicine service in August 2020, which performed nearly 3 million non-COVID-19 consultations to March 2021.12 There was an overwhelming response to online certificate and diploma courses in telemedicine among physicians, which already indicates the increasing popularity of telemedicine.12 This could have a lasting effect in India, where the healthcare system distribution is skewed towards urban areas. Group patient awareness programs and video conferences can be useful in educating patients about COVID-19 and IBD.8
Reorganisation of IBD management strategies is warranted in pandemic settings. Shortages of beds during the COVID-19 pandemic is an important issue in the developing world, as many centres were converted to COVID-19 centres. Rescheduling of appointments to video or telephonic consultation, treating flares with oral steroids after real-time PCR testing (available for free), and/or the escalation of 5-ASA dosage, limiting endoscopy for emergency (acute severe colitis, haemorrhage, etc.), and admitting only if steroids fail through online appointment, can help to manage patients with IBD in resource-limited settings.2
Optimising drug management in IBD in resource-limited settings is different from other parts of the world. According to the American and European guidelines of IBD in COVID-19, steroids and azathioprine are considered unsafe, whereas biologics and 5-ASA are considered safe. They also advise to stop or taper steroids quickly (10 mg/week) if used for treatment of flares and recommend anti-TNF monotherapy for maintenance of remission.36,51 However, due to the lack of universal health insurance, most of the treatment expenditure is borne by patients. Moreover, the risk of reactivation of tuberculosis is also substantial. This hinders the use of Western guidelines in the resource-limited Asian context. These guidelines are based more on opinions, rather than high-quality scientific evidence. In a digital survey of patients with IBD, the frequency of COVID-19 was not higher in patients using immunomodulators, although the sample size was small. Therefore, steroids and azathioprine remain attractive options for treating flares and maintaining remission, due to their low cost.22 COVID-19 testing prior to initiation of steroids or immunomodulators; adequate COVID-19 safety precautions; universal COVID-19 vaccinations for all patients with IBD; and use of alternative therapies like enteral nutrition and curcumin can be useful drug management strategies in patients with IBD in the current scenario, in resource-limited settings.52
Limiting endoscopy to high-priority cases (e.g., acute severe ulcerative colitis, acute gastrointestinal bleeding, cholangitis in concurrent primary sclerosing cholangitis, partial small bowel obstruction, and new diagnosis of IBD), postponing of screening endoscopy for cancer surveillance, and the use of faecal calprotectin to assess disease activity are useful strategies to manage endoscopy in patients with IBD during the pandemic. However, nearly a half of patients could not undergo investigations like faecal calprotectin and total leucocyte count, according to a telephonic survey of patients undergoing teleconsultation.8 Widespread availability of faecal calprotectin testing is an issue in resource-limited settings.
Limited outpatient services, initiation of telemedicine services, and admitting only complicated IBD cases such acute severe colitis can help manage the shortage of beds.22,52
Training physicians in telemedicine skills and biologic infusion, regular educational activity with IBD, and COVID-19-related information for physicians taking care of patients with IBD can improve care.12
IBD opinion leaders in this region should come together in resource-limited areas to prioritise management guidelines of patients with IBD, based on high-quality scientific evidence. Organisations like the IBD-ENC can play a crucial role in this by fostering a network for research collaboration and improving outcomes of patients with IBD in this challenging scenario.53







