BACKGROUND AND AIMS
Several studies have shown that image enhancement technologies like narrow-band imaging (NBI) and blue-light imaging (BLI) in expert hands can meet the Preservation and Incorporation of Valuable endoscopic Innovations (PIVI) criteria. However, attempts at more widespread generalisation of optical diagnosis have failed due to the inability of general endoscopists to meet the established standards.1,2 CAD-EYE (Fujifilm, Tokyo, Japan) is a novel AI-driven optical diagnosis system (CADx) that has shown encouraging preliminary results in expert hands or in single centre studies.
METHODS
This is a multicentre prospective observational study comparing the performance of CAD-EYE with that of endoscopists. A total of four centres from Europe (Portsmouth, UK; London, UK; Eindhoven, the Netherlands; and Llubjana, Slovenia) were involved in the recruitment of both patients and endoscopists for this study. A total of 10 endoscopists were involved in the study from four European centres. The participating endoscopists were categorised into two groups: five experts and five non-experts. The CAD-EYE system is a real-time convolutional neural network-based image analysis system that can detect and characterise polyps in real time.
RESULTS
The overall sensitivity, negative predictive value (NPV), and accuracy by all endoscopists were 84.4%, 74.1%, and 86.2% respectively. CAD-EYE diagnosis was recorded in 85.9% of polyps. The overall sensitivity, NPV, and accuracy of CAD-EYE were 83.0%, 72.8%, and 85.9%, respectively (p>0.05; Table 1).
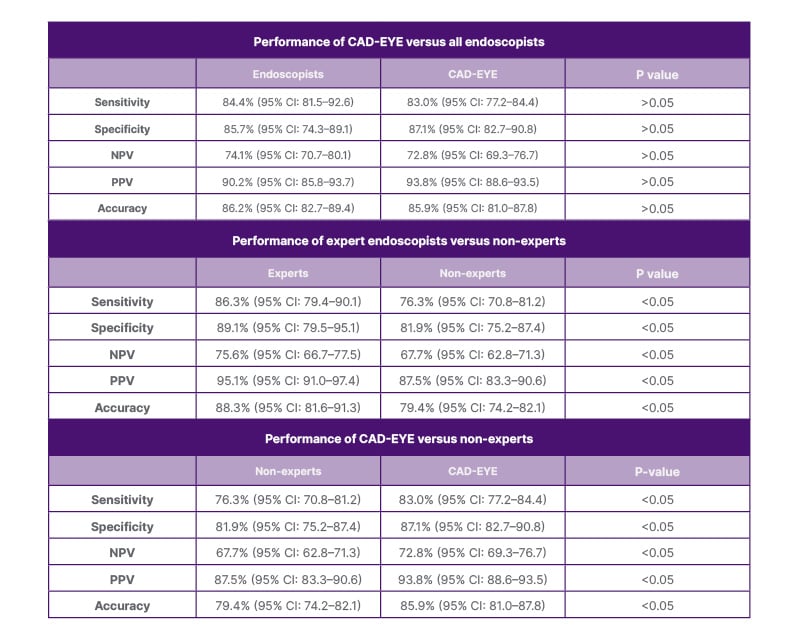
Table 1: Performance of CAD-EYE compared with expert endoscopists and non-experts.
NPV: negative predictive value; PPV: positive predictive value.
Optical diagnosis was performed with high confidence by the endoscopists in 84.9% of diminutive polyps (≤5 mm), with an overall sensitivity, NPV, and accuracy of 84.6%, 74.5%, and 84.9%, respectively. CAD-EYE diagnosis was recorded in 84.2% of diminutive polyps, with an overall sensitivity, NPV, and accuracy of 83.4%, 73.2%, and 84.2%, respectively (p>0.05).
The endoscopists’ optical diagnosis-based post-polypectomy surveillance interval was calculated in all patients and compared with histology-based surveillance, and it achieved a 90.7% (95% CI: 84.6–93.8%) and 92.9% (95% CI: 89.4–95.0%) concordance with British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guidelines, respectively. The post-polypectomy surveillance interval based on CAD-EYE diagnosis was calculated and compared with histology-based surveillance, and it achieved 91.9% (95% CI: 88.7–93.2%) and 93.4% (95% CI: 90.2–96.8%) concordance with BSG and ESGE guidelines, respectively.
An improvement in the performance of non-experts during the study was noted, with an improvement in accuracy from 63% for the first 50 polyps to 85% for the last 50 polyps, with an associated increase in sensitivity (65% and 82%), specificity (50% and 91%), NPV (55% and 79%), and also degree of confidence (65% and 90%; p<0.05).
CONCLUSION
CAD-EYE-based diagnosis can meet PIVI criteria and help introduce a ‘resect and discard’ approach, and leave in situ strategies even in the hands of non-experts. The authors have also demonstrated an improvement in performance of non-expert endoscopists over the course of the study.







