BACKGROUND AND AIMS
Functional gastrointestinal disorders are often associated with changes in the psycho-emotional sphere. The urgency of the problem is determined by the fact that functional diseases mainly affect young people of working age. This makes the problem not only medical but also social.
The aims of this study were to evaluate the clinical characteristics of anxiety and depression in different subtypes of functional dyspepsia (FD) group in comparison to a control group and to establish the presence of a possible correlation between anxiety/depression and quality of life (QoL).
MATERIALS AND METHODS
In total, 125 patients with FD (Rome IV criteria) and 70 healthy volunteers were included in this cross-sectional study. All participants filled out the Hospital Anxiety and Depression Scale (HADS) to identify anxiety and depression, the Short Form-8 (SF-8) questionnaire (standard 4-week form) to assess QoL, and the Leuven Postprandial Distress Scale (LPDS) to rate the severity of epigastric pain (burning) or abdominal discomfort. Linear regression analysis was performed in the case of functional relationships between two groups of random variables. Results obtained with p<0.05 and 95% confidence intervals were considered statistically significant.
RESULTS
Anxiety and depression were observed in 50.4% and 42.4% of patients with FD, respectively, and in 13.3% and 6.66% of healthy volunteers (p<0.001). The average anxiety score in patients with FD was higher than in controls (7.93 versus 4.17; p<0.001), with a maximum score of 17. The average score of depression in patients with FD was also higher (6.94 versus 3.40; p<0.001), with a maximum score of 15. All patients with FD had a low level of QoL, both due to physical health and emotional and psychological components compared with controls (p<0.001). A positive correlation was found between the levels of anxiety and depression and the severity of clinical manifestations of the disease (r=0.353 and r=0.291; p<0.05). A negative correlation was observed between the severity of dyspepsia and the QoL of patients (r=-0.264; p<0.05). The linear correlation was found between the QoL (physical health) and depression (r=-0.311; p=0.004). The results are summarised in Table 1.
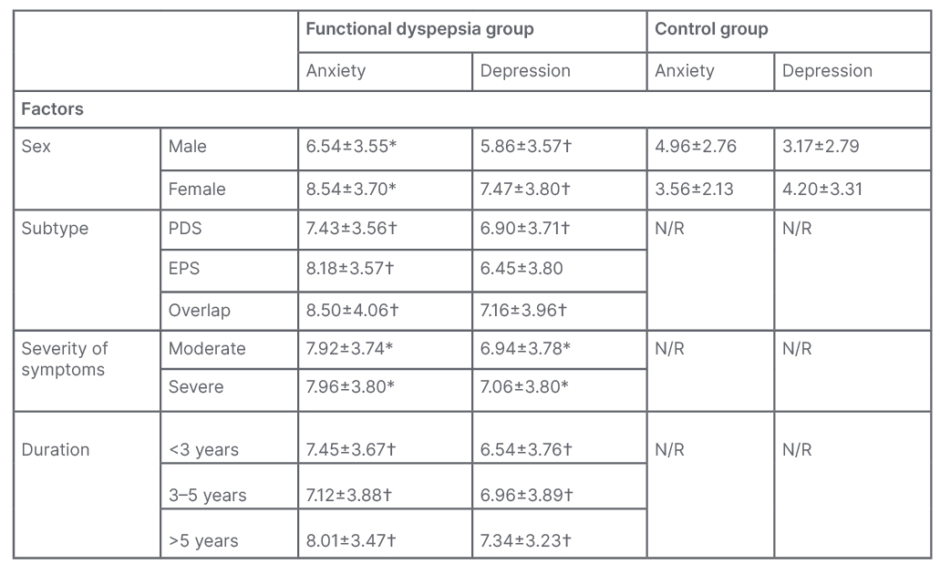
Table 1: Hospital Anxiety and Depression Scale (HADS) indicators of functional dyspepsia and control groups.
*p<0.05 in comparison with the control group and intragroup indicators.
†p<0.05 in comparison with the control group.
EPS: epigastric pain syndrome; N/R: not reported; PDS: postprandial distress syndrome.
CONCLUSION
Mental disorders are associated with changes in visceral sensitivity in patients with FD, who perceive pain impulses as aggravated. The HADS assessment showed that anxiety outweighed depression. The most significant factors influencing the level of anxiety and depressive disorders in the FD group were the patient’s gender and the severity of clinical symptoms. Self-reported symptom severity, anxiety, and depression were clearly and independently associated with QoL.








