Barrett’s surveillance currently involves untargeted mapping biopsies; however, this procedure can still miss certain pathologies.1 Acetic acid (AA) can be used to identify neoplasia for targeted biopsy2 but has not previously been studied in a surveillance population.
We performed a multicentre, randomised, crossover feasibility study to compare neoplasia detection with AA-targeted biopsies and untargeted mapping biopsies in a Barrett’s surveillance population with no history of dysplasia or cancer. All patients underwent two gastroscopies 8 weeks apart, one with AA-guided biopsy of abnormal areas only (Portsmouth protocol) and one using the Seattle protocol for mapping biopsies. The neoplasia yield (low-grade dysplasia [LGD], high-grade dysplasia [HGD], and cancer) and number of biopsies taken with each strategy were evaluated. Recruitment and retention were assessed and qualitative telephone interviews were conducted. Qualitative sampling continued until data saturation was attained; thematic analysis was used.
Recruitment comprised six UK centres and 200 patients, with a mean age of 66 years (standard deviation: 11.1). A total of 145 participants were male and the mean Barrett’s length was C4M6; 192 participants completed at least one procedure, with 175 completing both. The neoplasia prevalence was 11 out of 192 (5.8%). All cases of HGD and cancer were found with both protocols, with a full breakdown shown in Table 1. All LGD patients underwent further gastroscopy, with no neoplastic changes found in any of the cases during follow-up. Using the Seattle protocol, 2,139 biopsies were taken, with a pathology cost of £125,987 (306 biopsies per neoplasia, with a cost of £18,023). In contrast, 226 biopsies were taken with the Portsmouth protocol, equating to a total cost of £13,311 (75 biopsies per neoplasia, with a cost of £6,656). This represented a 4-fold difference in the number of biopsies per neoplasia. On restricting analysis to HGD and cancer, 1,070 biopsies were required per lesion found using the Seattle protocol and 113 biopsies per lesion found using the Portsmouth protocol, which represented a 9.5-fold difference.
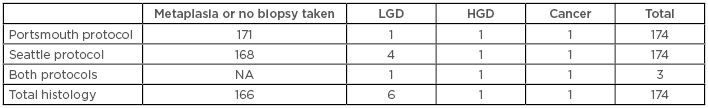
Table 1: Breakdown of diagnoses by protocol.
HGD: high-grade dysplasia; LGD: low-grade dysplasia; NA: not applicable.
For the qualitative study, we interviewed 21 participants to achieve data saturation, 6 non-participants, and 6 clinicians (1 per UK centre). Participants found the AA procedure simple and quick, with less pain and soreness experienced post-procedure. They felt the technique could potentially give more immediate results, providing reassurance or leading to more rapid treatment. Clinicians found the technique easy to implement following training3 and noted decreased discomfort for patients.
This was the first randomised controlled trial to compare these two techniques and it was reassuring that no cases of HGD or cancer were missed with either technique. LGD remains controversial4 and we believe inflammation could have resulted in a false–positive LGD result within this cohort, since subsequent gastroscopy and biopsies did not reveal LGD in any of the cases. A huge reduction in the number of biopsies can reduce the cost and time required for the procedure; therefore, these feasibility data support a definitive trial of AA-targeted biopsies in Barrett’s surveillance.
This UEG Week presentation generated considerable discussion. Delegates were surprised at the high level of retention in the study, with 88% of patients completing both endoscopies. It was questioned whether a randomised trial rather than a crossover design could have been used, but the qualitative data supported this design because it is the safest way of avoiding missed pathologies. It was questioned whether advances in endoscope resolution and advanced imaging technologies would render AA chromoendoscopy obsolete. However, it was recognised that, to date, there have been no studies comparing effectiveness of these techniques in Barrett’s surveillance, and from an international perspective, it will be some time before there is universal adoption of new equipment, which is currently very expensive. AA can be used with any endoscope, making the technology universally available.








