Abstract
Background: The prostate gland is anterior to the rectum. There are different positions for digital rectal examination, and 95% of individuals are right-handed. This study aimed to determine the suitability and efficacy of right lateral digital rectal examination (RLDRE).
Methods: A prospective cross-sectional study was conducted in a tertiary hospital on men with lower urinary tract symptoms due to benign prostate enlargement or prostate cancer. The perceptions of patients, surgical trainees, and medical students during RLDRE was assessed using the Likert scale questionnaire. The age and clinical presentation were documented. The ability to appreciate abnormal prostate disease was evaluated. The data was analysed using Statistical Package for Social Sciences (SPSS) version 24 (IBM, Armonk, New York, USA). Pearson’s correlation coefficient for non-categorical variables was performed and the level of significance was p<0.001. Ethical approval was obtained.
Results: A total of 203 patients were recruited, of which surgical trainees and medical students assessed 130 and 73 patients, respectively. The patients’ mean age was 69.5±9.1 years. The main presentations were urethral catheter in situ due to acute urinary retention in 77 patients (37.9%) and moderate lower urinary tract symptoms in 62 patients (30.5%). The number of patients with the RLDRE perception of well-tolerated, less awkward, and less painful were 161 (79.7%), 121 (59.9%), and 130 (64.4%), respectively. The perceptions of surgical trainees and medical students for ease of RLDRE were 77.7% and 74%, respectively, and for detection of abnormality were 57% and 68.5%, respectively. Detection rates for prostate cancer by surgical trainees and medical students were 87.5% and 75%, respectively, and for benign prostatic hyperplasia were 87.5% and 62.5%, respectively.
Conclusion: RLDRE was well tolerated by patients. Surgical trainees and medical students were comfortable with RLDRE with reasonable detection of benign prostatic hyperplasia and prostate cancer.
Key Points
1. There is variation in the preference for digital rectal examination (DRE) position by urologists and patients. It is difficult to teach and assess DRE skills.2. This is a case-control prospective clinical study of right lateral DRE by surgical trainees and medical students, including their perceptions as well as patients’ perceptions.
3. Right lateral DRE is simple, based on the anterior relation of the prostate and right-handedness in 95% of individuals. Left lateral DRE for left-handed individuals.
INTRODUCTION
The worldwide prevalence of benign prostatic hyperplasia (BPH) varies between 20–60% in men over 50 years. Similarly, about 50% of men over 60 years in South Africa had BPH. In Nigeria, the incidence of BPH was 23.7% among community-dwelling men.1,2 Digital rectal examination (DRE) is important in the clinical diagnosis of BPH based on a smooth and enlarged prostate.2-8 The presence of suspicious findings doubles the risk of clinically significant prostate cancer.3 David R.H. et al,9 in a systematic review of the accuracy of DRE to measure prostate volume, reported that DRE was weak at estimating size but is good at detecting enlargement of the prostate. Studies corroborated the ability of DRE to estimate prostate size when the volume is greater than 30 mL.10 DRE was reported to detect prostate cancer in 63.4% of men in a study by Ying Y et al.11 The usefulness of DRE is well captured by the saying that: “By far your greatest aide will be the finger. The majority of diseases which affect the rectum can be made out by the educated finger.”12
Be that as it may, there are several debates as to the use of DRE as a screening tool for prostate cancer. DRE was not useful in detecting prostate cancer in men with prostate-specific antigen (PSA) 3.0–3.9 ng/mL.13 A systematic review and meta-analysis of primary care providers did not show any evidence to support the efficacy of DRE in screening for prostate cancer.14 It was argued that with the advent of a multiparametric MRI study, DRE did not fulfil the World Health Organization (WHO) criteria for screening. In the primary health care setting, DRE was not recommended as a routine for prostate cancer screening.15 On the contrary, digital anal rectal examinations in the public health screening programme for anal cancer satisfied most of the WHO criteria as a screening examination.16
From the general practice point of view, DRE is accurate and abnormal DRE carries a 42.3% risk of prostate cancer, which is above the 3% risk threshold of the UK National Institute for Health and Care Excellence (NICE) guidelines.17 Walsh AL et al.,18 in the primary health care setting, reported that DRE alone had sensitivity, specificity, and positive predictive values of 81%, 40%, and 42%, respectively, in detecting prostate cancer in a retrospective cohort analysis. DRE is important from a contemporary cohort of patients undergoing an initial 12–18 core prostate needle biopsy.19
DRE played a limited role in the era of COVID-19 and post-COVID-19, where there was rapid adoption of virtual consultation in the form of telephone or video consultation, making DRE difficult. PSA measurement and MRI were available and were the preferred choices. DRE may detect prostate cancer in individuals who are Black. Abnormal DRE in a symptomatic patient has a positive predictive value for prostate cancer above the current NICE threshold requiring urgent referral. Therefore, DRE is important in individuals of African descent with lower urinary tract symptoms (LUTS).1,17-22
In order to increase the chances of detecting prostate cancer in men, DRE rectal examination has been combined with serum PSA and MRI with a reasonable higher cancer detection rate.23-32
The under-utilisation of DRE alone when screening for prostate cancer has been attributed to the 61.1% of medical doctors who never performed DRE despite screening with PSA. Prostate cancer was only detected in 3–5% of the population screened with a combination of DRE, PSA, and transrectal ultrasound (TRUS).33 In a study by Teoh M et al.,34 doctors in training had a low level of confidence and comfort in performing DRE, limiting the utilisation of DRE as a critical diagnostic tool. In 2012, the United States Preventive Service Task Force (USPSTF) recommended against routine PSA screening. This led to a significant drop in the utilisation of DRE and PSA by primary physicians from 16.0% to 5.8% for DRE and 27.3% to 24.5% for PSA.35 DRE is often an overlooked part of physical examination that is informative in the hands of skilled physicians, particularly in revealing some rectal diseases.36 The preference for performing DRE on men with health insurance compared to patients who attended public hospitals in Brazil may increase overdiagnosis and overtreatment of prostate cancer.37
DRE is an essential requirement for medical practitioners, as well as a necessary skill for medical students before their exit from university. It was found across several studies that 25% of the medical students had no experience with performing DRE.38-40 The diagnostic test accuracy of DRE for prostate cancer in symptomatic patients among general practitioners in the UK was 42.3%, above the NICE 3% risk threshold.17 Of note is the observation that abnormality on DRE is not easily picked in patients who are obese, but when detected it improves the predictive value of prostate cancer, and this is significantly higher among men who are obese compared to those of a normal weight.9
Up to 50% of men with abnormal DRE before prostate needle biopsy were eventually confirmed to be prostate adenocarcinoma. The DRE features suggestive of benign prostate enlargement (BPE) include non-tender, smooth, and firm prostate gland, while in patients with malignant prostate enlargement includes hard, irregular prostates with or without obliteration of the median groove.19
During the left lateral position, the medical student is taught to rotate their index finger in the rectum to appreciate the characteristic features of a diseased prostate. This technique is not easily learnt but improves with the status of the clinician from residents to consultants.11
With increasing desire to further improve the diagnostic test accuracy of DRE, researchers and clinicians have conducted studies to standardise the ability to interpret the findings of DRE. One fingertip surface area is equivalent to 1 g of prostate tissue, which is equal to 1 cm3 volume, and this correlated well with prostate volume when assessed by ultrasound.41 Sinam LB et al.,6 also corroborated the correlation DRE estimate of prostate volume with TRUS measurement. Although there was some degree of overestimation of prostate volume by DRE, the coefficient of internal consistency was 0.851. The first attempt at standardisation of DRE in inexperienced hands established a linear correlation between DRE and ultrasound prostate volume.41 Muangpoon T et al.,42 designed the augmented reality system for digital rectal examination training and assessment to improve teaching and learning of DRE skills by providing visualisation of the finger and internal organs. The initial user study proved the applicability and usefulness. They proposed improvement of this device by using the HoloLens, which will offer a larger field of view and resolution or haptic based instead of the standard benchtop model, which is expected to generate a variety of abnormalities of prostate diseases.
In the 1990’s, the preferred position for DRE was the proctologic referred to as knee-chest or prone jackknife position. However, lateral decubitus or Sim’s position is better in very ill patients.4 As R.H. Major said: “A wag once remarked, with considerable truth, that a consultant is a doctor who makes a rectal examination.”4
In the USA, the best position for DRE is the standing position or the knee-chest position.7,43 A randomised controlled study in France, analysed the lower and middle rectum and sphincter function in a DRE.44 The study concluded that the left lateral position, compared to the dorsal position, allowed the complete examination of the circumference of the rectum.44
According to a study among urologists in Brazil about their preferred position for DRE, four positions were performed in decreasing order, including lithotomy (64.3%), left or right lateral (17%), standing up (14.2%), and squatting down with elbows on the table (3.4%). However, 42.7% of the patients preferred the left lateral DRE (LLDRE) position.45 In another study in India, the cross-leg lithotomy position (78.3%) was preferred by the patient compared to the left lateral position (21.75%). It afforded the urologist to completely examine the prostate (cross-leg11.15±1.96/12 versus left lateral 9.25±2.50/12; p<0.001).46
Considering the various positions for the DRE, most individuals (95%) are right-handed, and the prostate gland is anterior to the rectum.47,48 In addition to the perceptions of patients, and medical students and doctors-in-training ability to perform DRE. 34 This study determined the patient’s perception of RLDRE compared to the LLDRE, as well as the urology trainees’ and medical students’ perceptions and ability to appreciate abnormalities of prostate diseases with the RLDRE position.
MATERIAL AND METHODS
Setting
Urology surgery outpatient clinic at the University College Hospital, Ibadan.
Study Design
The RLDRE position and LLDRE position were explained to patients who presented with LUTS. The patients were asked to compare their experience between both positions of examination. They picked a simple ballot of “R” for right or “L” for left to determine which position was performed first. Both examinations were done on the same day.
The senior registrars (surgical trainees) and final-year medical students (medical students) were taught how to perform the RLDRE though they were quite conversant with the LLDRE. A proforma was designed and prospectively administered by surgical trainees and medical students to the patients. Two hundred and three men who voluntarily consented were enrolled in the study. The patients, urology surgical trainees, and medical perceptions on the Likert scale 1 (strongly agree) to 5 (strongly disagree) were assessed, as well as the rectal examination findings.
The Likert scale was further regrouped as Likert scores 1 and 2 were in favour, score 3 was undecided, and scores 4 and 5 were against tolerating RLDRE rather than LLDRE. In favour of RLDRE versus LLDRE, perceptions of not awkward, not more painful, and patient did not mind facing the examiner were 4 and 5, undecided was 3, and against was 1 and 2, respectively.
The regrouping of the surgical trainees and medical students’ perception using the Likert responses, RLDRE easier to perform and appreciated abnormal DRE findings was 1 and 2, undecided was 3, and did not mind facing patient scale 4 and 5, respectively.
Study Type
Cross-sectional prospective hospital-based study.
Inclusion Criteria
Men with LUTS due to suspected BPE or prostate cancer.
Exclusion Criteria
Men with urethral strictures, neurogenic bladder, and acute prostatitis.
Participants
The study included 203 patients, of which 130 and 73 were assessed by surgical trainees and medical students, respectively.
Variables
Patients’ perception; age in years; international prostate symptom score (IPSS); quality of life or bordersome score; serum PSA; prostate volume in cubic centimetres and post void in millilitres, both assessed by transrectal/abdominal ultrasound; urology trainee perception.
Data Analysis
The results of the perceptions were represented in tables. The data was analysed using SPSS version 24. The Pearson’s correlation coefficient was determined for the perceptions of the surgical trainees and medical students regarding RLDRE and LLDRE and the level of significance was p<0.01 or p<0.05, respectively. The p<0.01 and 0<0.05 corresponds to 99% and 95% CI, respectively.
Techniques of Digital Rectal Examinations
Right lateral digital rectal examination.
The patient is positioned horizontal lying on his right side on the examination couche facing the examiner. The hips are flexed at 90 degrees to the body and knees flexed at a right angle to the thigh. The examiner introduces the gloved, lubricated right index finger through the anal sphincter into the rectum and performs the examination of the prostate. The examiner appreciates the prostate that is anterior to the rectum. Then palpates the size of the prostate, the presence of a median groove, and whether the capsule is smooth, irregular, or hard. They check for tenderness and whether the rectal mucosa was fixed to the prostate or freely mobile. At the end of the examination the patient is cleaned.
Left Lateral Digital Rectal Examination
The patient lies on the left side of his body on the examination couche with back towards the examiner. The trunk is diagonal, both hip and knees are flexed, and the thigh and legs both parallel to the trunk. With the examiner standing and facing the buttocks, the right index finger is lubricated with K-Y-jelly and introduced through the anal sphincter into the rectum. The examiner then rotates his index finger anti-clockwise 180 degrees, bending down parallel to the examination couche and facing the head of the couche. The characteristics of prostate features suggestive of benign or malignancy are noted. Then they stand up, rotate their finger 180 degrees clockwise and remove their index finger. At the end of the examination the patient is cleaned.
Outcome Measures
The patients, surgical residents and medical student’s perceptions are represented by a table. The correlations between the perceptions of surgical residents and medical students as well as the correlations on the ability to appreciate abnormal DRE using the right lateral position.
Limitation
For a left-handed examiner, the patient will lay on the left side of the body with the body horizontal facing the examiner. The hips are flexed at 90 degrees to the body and knees flexed at right angle to the thigh. The examiner stands in front of the flexed knees and examines the prostate as described for the right lateral digital examination. However, there were no left-handed surgical trainees or medical students.
Ethical Issues
The patients were identified with numerical serial numbers that do not reveal their identity in compliance with the Helsinki declaration on human rights. Thereafter, a signed informed consent or fingerprint from illiterate patients was obtained. There was no malevolence with the patient. The institutional research board ethical approval was obtained UI/UCH EC registration number: NHREC/05/01/2008a.
RESULTS
A total of 203 patients were recruited into the study, of which surgical residents and medical students assessed 130 (64%) and 73 (36%) patients respectively. The mean age of the patients was 69.5±9.1 years (range: 38–99 years). The mean, standard deviation, and range for PSA, PSA density, and prostate volume were 355±1928 (0.5–20,870.0) ng/mL, 3.5±19.6 (0.01–216.00) ng/mL/mL, and 90.4±68.8 (14.6–477.0) mL, respectively. Seventy-seven (37.9%) patients presented with urethral catheter in situ and three (1.5%) had suprapubic catheter due to acute urinary retention. The others were mild, moderate, and severe LUTS were 16.3%, 30.5%, and 13.8%, respectively.
Regarding the perception of DRE positions, the patients felt that the right lateral position, compared to the left lateral position, was well tolerated, less awkward, less painful, and caused less worry about facing the examiner in 161 (79.7%), 121 (59.9%), 130 (64.4%), and 122 (60.4%) patients, respectively (Table 1).
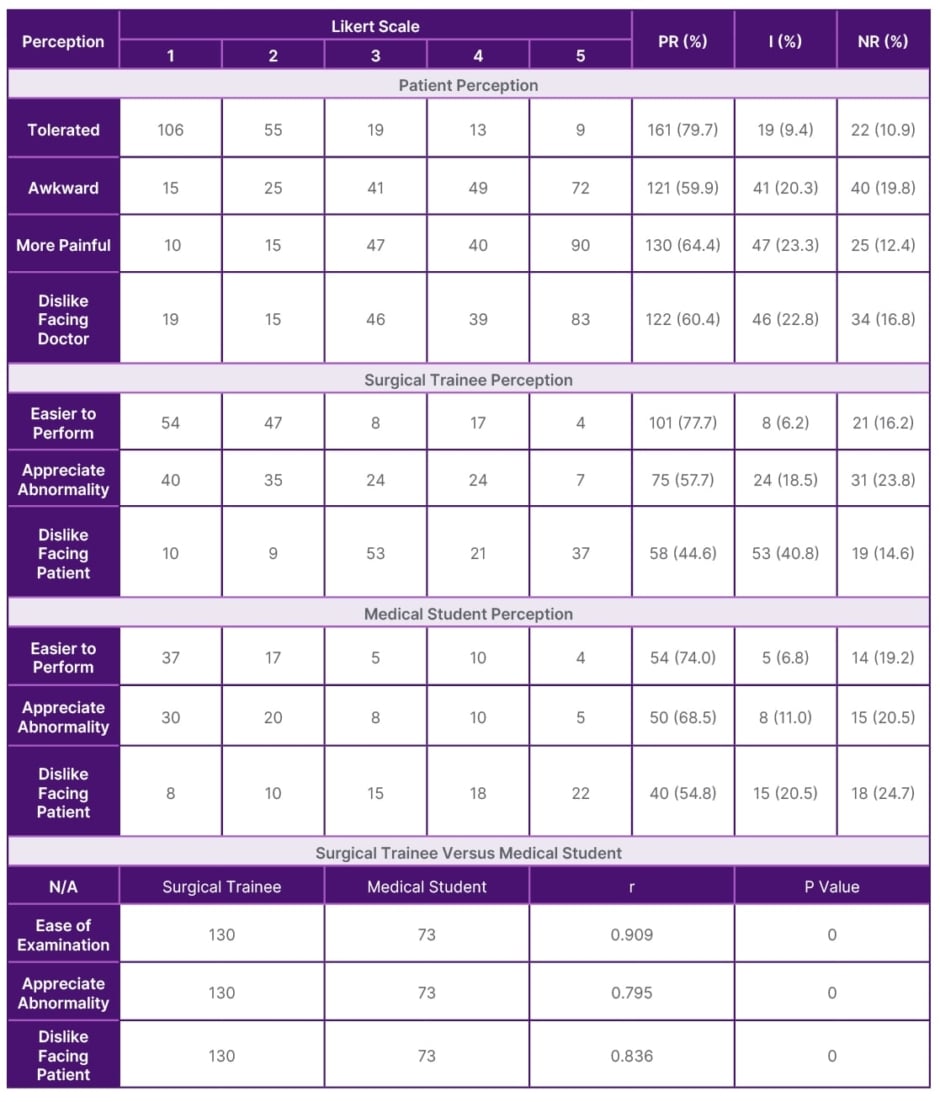
Table 1: Patients, surgical trainee, and medical student perception of right lateral versus left lateral positions for digital rectal examinations.
I: undecided response; NR: negative response; PR: positive response; r: Pearson’s correlation coefficient.
The percentage of surgical trainees and medical students with the perception RLDRE has a higher ease of performing compared to LLDRE was 77.7% and 74%, respectively. Similarly, prostate abnormality was better appreciated in the right lateral position in 101 (57%) patients by surgical trainees and 50 (68.5%) patients by medical students. The surgical trainees and medical students were not bothered about facing the patients during RLDRE in 44.6% and 54.8% of DRE examinations, respectively (Table 1).
Table 1 also shows the statistical significance and positive correlation of the perceptions by both surgical trainees and medical students to the ease of performing RLDRE (r=0.909; p=0.000), appreciation of prostate abnormality (r=0.795; p=0.000), and that they were not bothered about facing the patients during RLDRE (r=0.836; p=0.000).
The DRE findings suggestive of prostate cancers are absent median groove, irregular prostate gland (not smooth), and attachment of rectal mucosa to the prostate gland depending on the stage of the cancer. The chances of correctly palpating the clinical features of prostate cancer during RLDRE by surgical trainees and medical students were 87.5% and 75%, respectively (Table 2). While feeling features on RLDRE suggestive of BPE between the two groups were 87.5% and 62.5%, respectively (Table 2).
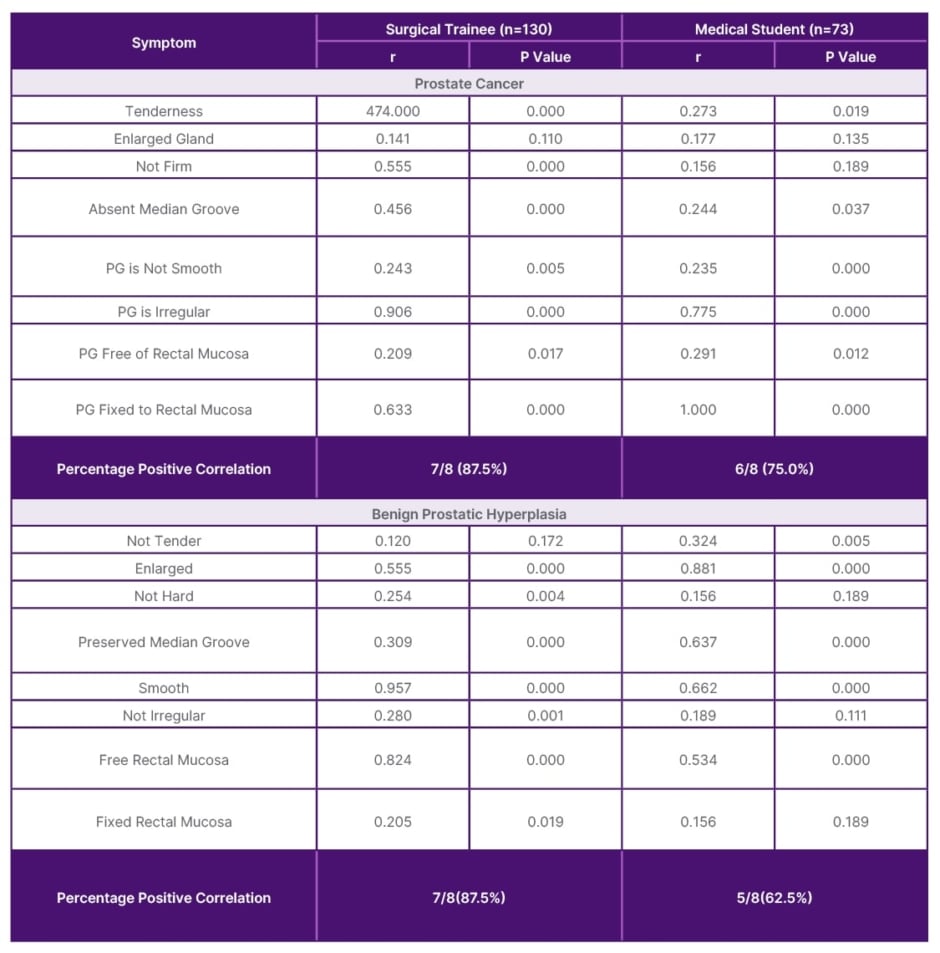
Table 2: Correlations of features of prostate cancer and benign prostatic hyperplasia with right lateral digital rectal examination by surgical trainees and medical students.
PG: prostate gland; r: Pearson’s correlation coefficient.
DISCUSSION
Digital rectal examination is always indicated in men with LUTS but is not recommended as a screening test for prostate cancer because 80% of those who had a biopsy done based on DRE were negative for prostate cancer.17,49 DRE is not useful in screening for prostate cancer as it is poor as a stand-alone test.50 In Prostate Research on Behavior and Education (PROBE) Survey in Europe, most urologists performed DRE on patients with LUTS due to BPH.51 The Canadian Family Physician 2019, Canadian Urological Association (CUA), American Urological Association (AUA), and European Association of Urology (EAU) guidelines all include DRE in the workup of men with LUTS due to suspected BPH.52,53,54,55 This is consistent with this study where we investigated the perception of the patients with LUTS, medical students, and surgical trainees to RLDRE. We assessed the ability of the medical students and surgical trainees to appreciate abnormalities of the prostate using the RLDRE technique compared to the left lateral position.
DRE is valuable in establishing that the prostate gland is enlarged. 9 Despite some degree of overestimation, the DRE prostate size correlated well with the TRUS volume.6,10 The European Association of Urology stated that DRE can estimate prostate volume but is less accurate compared to ultrasound. In China, patients who had a prior PSA and multiparametric MRI were sent for prostate biopsy. Experienced urologists and residents who performed the DRE before TRUS biopsy were blind to this information. The diagnostic accuracy of DRE in patients with suspected prostate cancer referred for biopsy was 63.45%.11 Stephan et al.,3 reported that, according to rounded data without considering DRE, the risk of clinically significant prostate cancer within 10 years is about 1%, 5%, and 20% for men with PSA levels of <2 ng/mL, 2–3 ng/mL, and >3 ng/mL, respectively. The presence of suspicious DRE doubles the risk of prostate cancer from 0.7% to 1.5%, from 3.5% to 6.5%, and from 13.7% to 23%, respectively. Thus, supporting the importance of DRE.3 However, students (33%) were less likely to accurately assess abnormalities in DRE compared to residents (64%) and clinicians (76%), with a p<0.05.56 The emphasis is for the medical students and surgical trainees to acquire this clinical skill of performing DRE as emphasised by Lass et al.52 To increase the chances of picking prostate cancer, DRE rectal examination should be combined with serum PSA, transrectal prostate ultrasound, multiparametric MRI, and prostate biopsy when the patient is fit for this last procedure.20,21,26,30,57-60
Romero et al.,45 a questionnaire-based study in Brazil, reported that the majority of the urologist preferred the lithotomy position (63.4%) for DRE, among others such as left lateral (17%), standing-up position (14.2%), and squatting down with elbow on table (3.4%). However, 42.7% of the patients preferred the left lateral position for DRE at their first visit.45 Nagathan DS et al.,46 reported that in India patients preferred the cross-leg lithotomy position, and the urologists were able to more completely examine the prostate than in the left lateral position. In the authors’ practice, all the men with LUTS routinely underwent DRE in the left lateral position at the surgical outpatient clinic. The exceptions to DRE were patients with acute prostatitis or those who were severely ill at the time of presentation.11 Furlan et al.61 reported that the majority of the patients in their study preferred a supine position for DRE. In the USA, the standing position or knee-chest position is preffered.7,43
Most patients in this study tolerated RLDRE, felt it was not awkward, less painful, and were not bothered facing the physician. This was unlike studies that reported moderate-to-high discomfort and pain during LLDRE.46,57 Despite these shortcomings of DRE, more men would subject themselves to a repeat DRE for fear of late identification of clinical prostate cancer.60 Frank J et al.,61 in a randomised study comparing the knee-elbow and left lateral position, patients were 1.9 times more comfortable with the knee-elbow position than the left lateral position. The patients also felt the knee-elbow position was twice as embarrassing as the left lateral position.60
This study demonstrated that both surgical trainees and medical students felt the RLDRE position was much easier (77.7% and 74%, respectively). This is not unrelated to the anatomic position of the prostate gland that is anterior to the rectum.48 Both surgical trainees and medical students were right-handed, consistent with Frayer D et al.,47 and both appreciated abnormalities of the prostate during RLDRE (57% and 68.5%, respectively).47 Therefore, a right-handed surgical practitioner would pick abnormal prostate features with the RLDRE position. The implication is that for left-handed surgical trainee or medical students, the patient should be placed in the LLDRE position.
Studies have shown the deficiency in the exposure of medical students to DRE in their undergraduate days. In Australia, 92% of medical students were taught, and 55% were not confident in interpreting findings of DRE because of a lack of supervision by senior colleagues.38 However, half of the medical students who studied in Pakistan and 8% in India performed DRE on mannequins. In India, 92% of medical students were taught DRE, with two-thirds performing less than five DREs before graduation due to inadequate supervision.39,40 In Ireland 24%, 20%, and 56% had no experience with DRE, did rectal examination on mannequins, and performed at least one DRE, respectively.62 It was also shown that inadequate supervision of doctors-in-training resulted in the underutilisation of DRE and that the ability to identify abnormality on rectal examination increases with experience and status. 34 This study showed that medical students were better than the surgical trainees in appreciating prostate abnormalities during RLDRE. Simulators, standardisation techniques, and augmented reality systems have been introduced to improve medical students’ skill acquisition for DRE.41,42,56 Interestingly, in this study there were significant correlations with the perceptions of both surgical trainees and medical students regarding ease of examination, appreciation of prostate abnormalities, and not being bothered with facing the patients during RLDRE.
DRE alone detected 55.8% of prostate cancer in the screening arms of the Rotterdam, the Netherlands section of the European Randomized Study of Screening for Prostate Cancer.43 DRE was quite sensitive in identifying prostate cancer in men with a PSA value greater than or equal to 10 ng/mL. This study revealed a much higher detection rate for prostate cancer by both surgical trainees (87.5%) and medical students (75.0%). This might be related to the mean PSA of 355 ng/mL in this study, which is much higher than in the Netherlands study (52 ng/mL).43 Debansu S et al.,63 found that suspicious DRE irrespective of the serum PSA level, detected 52.18% prostate cancer compared to 45.46% using a PSA cut-off of greater than 4 ng/mL.
Increase in BMI and abnormal DRE is a strong predictor for overall prostate cancer in men who are obese, and is associated with high-grade prostate cancer.9 However, BMI was not measured in this study, which is a limitation, though subsequent studies will address this issue.
Koulikov D et al,64 documented the inability of the examining finger to reach and examine the apex, half, three quarter, and whole prostate in 93.7%, 66.3%, 23.2%, and 3.2% of cases, respectively. The limitation of this current study is that both surgical trainees and medical students were all right-handed. There is a need to investigate the perception of the LLDRE position in left-handed medical personnel, which is different from the traditional digital rectal examination position. Another limitation was that the authors did not determine the sample size before the study. This will be addressed in a future validation of a comparative study between RLDRE and traditional LLDRE.
What this study has shown is that patients better tolerated RLDRE than left lateral DRE, and that a significant percentage of senior surgical trainees and final year medical students were able to identify abnormalities of BPH and prostate cancer. However, the long-term impact of using RLDRE on patient outcomes and generalisability to different healthcare settings will become obvious with further study.
In conclusion, the RLDRE position is well tolerated, less awkward, and less painful to the patients. Both the surgical trainees and medical students felt RLDRE was easier, and they appreciated abnormal prostate features better. There were positive correlations of RLDRE perceptions and the ability to detect BPH and prostate cancer by surgical trainees and medical students. The RLDRE position is a scientifically logical paradigm shift from the traditional DRE position.







