Abstract
Tuberculosis is a well-known endemic disease in India; however extra-pulmonary tuberculosis in the form of single parotid gland involvement is exceptionally unusual. Nevertheless, in instances involving slow-growing, prominent parotid gland enlargement, where malignancy is our major speculation, it should never be eliminated as a differential. There have been very few previously reported cases of tuberculosis involving salivary glands, and at times imaging has proven it difficult to diagnose such a condition and differentiate it from a benign mass or a malignancy. With that in mind, the authors present a case of tuberculosis involving just a single parotid gland in a 49-year-old woman who had been experiencing unilateral infra-auricular swelling and pain for a month. Apart from evening rise in temperature and generalised weakness, the patient had no additional symptoms suggestive of tuberculosis infection. Ultrasound represents the initial imaging modality of choice for assessment of the parotid gland. A sonographic examination of the authors’ patient revealed a diffusely enlarged left parotid gland with peripherally vascular hypo-echoic areas within. On contrast-enhanced CT the left parotid gland was seen to be replaced by a heterogeneously enhancing lesion, with an abscess-like appearance. The tubercular aetiology was established after a USG-guided tru-cut biopsy from the infra-auricular region revealed numerous loose granulomas with few langhans-type multinucleate giant cells amidst foci of necrosis and a salivary duct. Anti-TB medication was initiated for the patient subsequent to the presence of acid-fast bacilli on Ziehl-Neelsen staining. The patient has now received 3 months of AKT and there has been complete resolution of the symptoms.
Key Points
1. Since tuberculosis is a prevalent endemic illness with a high incidence rate in India, the diagnosing clinician should be suspicious of unusual extrapulmonary tuberculosis cases such as salivary gland infections.2. The authors address one such uncommon instance of unilateral parotid involvement in this case report, which involved a patient without any other radiological features suggestive of tuberculous infection and a normal chest X-ray.
3. The case report highlights the value of imaging tests such as CT, ultrasound, and biopsy, as well as the need for pathologist involvement in the diagnosis of such uncommon illnesses.
INTRODUCTION
Tuberculosis is a well-known endemic disease in India; however, extra-pulmonary tuberculosis in the form of single parotid gland involvement is exceptionally unusual. Nevertheless, in instances involving slow-growing, prominent parotid gland enlargement, where malignancy is the major speculation, it should never be eliminated as a differential. Having a strong index of suspicion by the diagnosing physician is crucial for the ultimate diagnosis. Tuberculosis as a cause of parotitis is typically disregarded by otolaryngologists, and the majority of cases are unnecessarily operated.
CASE PRESENTATION
A 49-year-old female patient, a known case of hypertension and diabetes, was referred to the authors’ ear, nose, and throat department with suspicion of acute unilateral parotitis. The patient complained of gradually increasing swelling and associated pain in the left infra-auricular region for 1 month. Initially, the swelling was pea-sized and non-tender, without any secondary skin changes. The swelling gradually increased for 1 month and was associated with mild pain.
On inspection, the swelling was 5×4×2 cm in size, firm-to-hard in consistency, non-mobile, non-fluctuating, and with no local rise of temperature. There was no discharging sinus or fistula. There were no dental complaints, and the oral hygiene of the patient was also good. Apart from the evening rise in temperature and generalised weakness, the patient had no additional symptoms suggestive of tuberculosis infection. She denied any recent oro-dental surgical procedures, as well as any personal or contact history of tuberculosis. On investigation, the routine blood counts including the erythrocyte sedimentation rate, fasting blood sugar, liver and kidney function tests, urine analysis, electrocardiogram, and abdominal ultrasound revealed no abnormalities. HIV serology came up negative as well. The chest radiograph was also unremarkable (Figure 1A).
On ultrasonography of the left parotid region, the gland was enlarged, and a well-defined, heterogeneously hypo-echoic, oval mass lesion was noted within its architecture. It was approximately 4.7×2.1 cm in size (Figure 1B). No ductal dilatation, cystic degeneration, or intraparenchymal calcifications were observed. The colour doppler study revealed a notable degree of arterial vascularity with relatively high resistance in the periphery of the lesion (Figure 1C). In the left upper cervical area (Level II) and left sub-mental and submandibular region (Level I), a few enlarged sub-centimetric reactive lymph nodes were observed. There was noticeable vascularity and a retained fatty hilum in these lymph nodes. A tentative diagnosis of either neoplasm or granulomatous infection was made. Given the lesion’s accessibility, ultrasound-guided biopsy and contrast-enhanced CT were recommended to rule out the differentials.
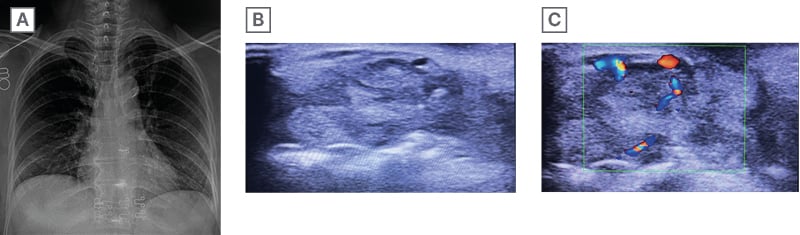
Figure 1: Chest radiography and ultrasonography of the left parotid region.
A) Chest radiograph posteroanterior view depicts no significant findings. B) Ultrasonography image shows a well-defined heterogeneously hypo-echoic oval lesion measuring 4.7×2.1 cm with no calcification or cystic areas within. C) On colour doppler, vascularity is noted in the periphery of the same lesion.
On contrast-enhanced CT, a distinct, lobulated mass lesion with heterogeneous enhancement was noted involving the left parotid gland’s superficial and deep lobes. The lesion measured 2.7×2.2×2.7 cm in the superficial lobe and 2.8×1.7×2.3 cm in the deep lobe of the gland (Figures 2A and 2B). There were no calcifications or cavitations within the lesions. The main parotid duct was normal in calibre. Sialolitiasis was absent. There were no signs of fistulisation or any sinus tracts. The underlying bones were normal without any signs of erosion. Left Levels I, II, and III showed few reactive lymph nodes. The right parotid gland was normal.
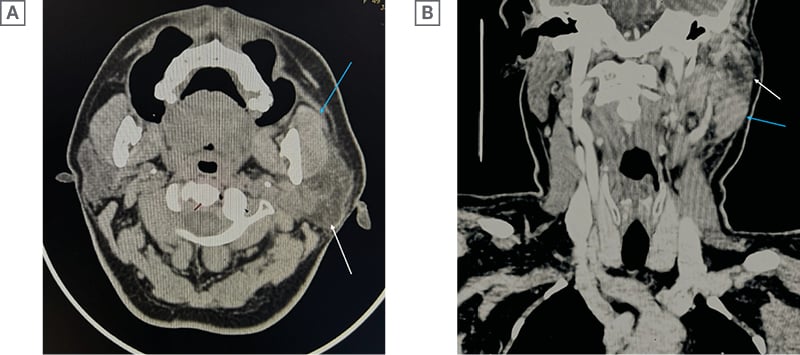
Figure 2: Contrast-enhanced CT of parotid and neck region.
A) Axial image and B) coronal image show a well-defined, heterogeneously enhancing, lobulated lesion involving the superficial and the deep lobe of the left parotid gland. The posterior and superior low attenuation peripherally enhancing region of the parotid gland s/o necrosis (white arrow). The anterior and inferior intensely enhancing portion of the lateral lobe is compressed due to inflammation (blue arrow). No focal areas of calcifications, cystic changes, or ductal dilatations can be seen within the lesion.
The fine needle aspiration cytology results were inconclusive; hence, an abdominal ultrasound-guided biopsy of the lesion was performed with an 18 g Bard biopsy needle, and histopathology revealed granulomatous inflammation with infiltrates of foamy and epithelioid lymphocytes with a focus on necrosis and salivary duct within. On high-power microscopy, occasionally Langhans and multi-nucleate giant cells of the foreign body type encircling a caseous form of necrosis were observed (Figure 3A and 3B). No cancerous cells were found. According to the histology report, the salivary gland had necrotising granulomatous inflammation that was suggestive of tuberculosis. A few acid-fast tubercle bacilli were seen on the Ziehl Neelsen stain (Figure 3C). Another sample from the lesion that was sent for Cartridge-Based Nucleic Acid Amplification Test came out to be positive for Mycobacterium tuberculosis.
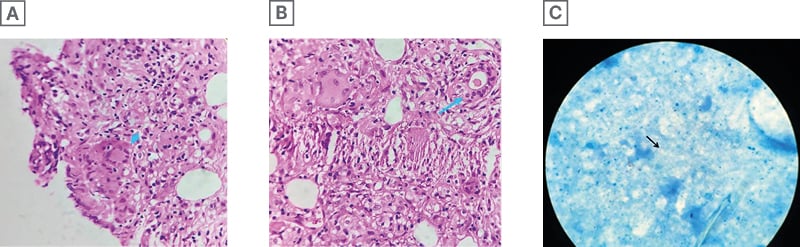
Figure 3: Histopathology image and Zeihl-Neelsen stain.
A) Histopathology image, haematoxylin and eosin, 400x, high power depicts an epithelioid granuloma containing a Langhans giant cell (blue arrow). B) Granulomatous inflammation with a focus of necrosis and a salivary duct seen in the upper right-hand corner (blue arrow). A) Zeihl-Neelsen stain of the samples taken from the same patient show acid-fast dye-positive tubercle bacilli (black arrowhead).
There have been very few previously reported cases of tuberculosis involving salivary glands, and at times imaging has proven it difficult to diagnose such a condition and differentiate it from a benign mass, granulomatous disease, or a malignancy.
DISCUSSION
Tuberculosis is a common endemic disease and a major cause of suffering in developing countries such as India. It is a necrotising granulomatous infection that affects several organs, exhibiting a wide range of clinical manifestations. The lungs are often the most frequently affected organ. Extra-pulmonary organs affected include cervical lymph nodes, ileocaecal junction, bones, meninges, brain, and numerous other organs;1 however, parotid gland involvement is extremely uncommon.2 In 1893, the first case of tubercular parotitis was diagnosed by C De Paoli.1,3,7
As with this case, parotid tuberculosis can develop either primarily in the absence of pulmonary tuberculosis or concurrently with pulmonary tuberculosis.3 The lymph nodes or parotid gland can become involved in either of the two ways. First, a mycobacterial infection in the oral cavity releases the bacilli, which then ascend through the salivary gland duct and enter the gland or the lymph nodes that are connected to it through lymphatic drainage. The second channel originates from a distant primary lung focus and is either haematogenous or lymphatic in nature.2-8 Latter is the more common pathway.3-5 Seventy percent of the time, the parotid gland is involved when the main afflicted glands are the salivary glands.5
Primary parotid tuberculosis is cumbersome to diagnose in the absence of clinical symptoms of lung involvement or any systemic findings due to the resemblance of the presentation to that of a tumour.2,9,10 The majority of these cases manifest as slowly growing masses that progressively get larger over months and are arduous to distinguish from neoplasm or other granulomatous diseases through imaging. Physical examination is usually unfruitful. It is only in cases of concomitant primary pulmonary tuberculosis that chest radiography can be beneficial. In this instance, there was no chest radiological indication of ongoing or past pulmonary tuberculosis. In his research, Maynard J.11 revealed that a histological investigation was the only way to differentiate between this infection and a gland tumour. Histopathology in parotid lesions has a 94–100% specificity and an 81–100% sensitivity.5 Thus, when evaluating a parotid tumour, fine needle aspiration cytology or biopsy should be done initially.
In this patient, the primary source of the infection could not be identified as there were no molar caries nor other tubercular focus anywhere else. The confirmation of the parotid tuberculosis diagnosis was made possible by ultrasonography-guided tru-cut biopsy of the intraparotid lesions. Though strong suspicion of the same was made on contrast-enhanced CT, histopathology gave the final diagnosis. This case is unique because, unlike the majority of tubercular parotitis cases that have been documented in the past, the patient’s diagnosis came before any kind of surgery. On the other hand, the diagnosis was previously verified on post-surgery parotidectomy tissues because early imaging and histology were unable to provide a diagnosis.7,10 In this case, since the biopsy was conclusive, surgical intervention was avoided, and early therapeutic management in the form of anti-tuberculosis treatment was initiated. After 3 months of medication, there was complete resolution of the symptoms.
CONCLUSION
The patient was diagnosed with unilateral tubercular parotitis, and since then, treatment has been going well. A recent follow-up scan revealed only a few reactive cervical lymph nodes, and the infection in the gland had receded. The patient has been put on regular anti-tubercular medication for 6 months and has been advised a repeat chest X-ray after 3 months to look for signs of pulmonary tuberculosis. There has been constant monitoring of her health condition. The goal is to maintain or improve patient wellbeing. The authors’ wish to highlight the vital role and diligence of a radiologist and the use of imaging investigations like ultrasonography, CT, and biopsy, as well as the involvement of a pathologist in diagnosing such unusual conditions. Furthermore, saving time and accurately diagnosing the ailment ensures that the patient receives suitable treatment at an appropriate time.
Take-Home Message
Even though tuberculosis has historically been a prevalent cause of a wide range of medical disorders in India, recognising such a rare entity as tubercular parotitis requires a high level of clinical suspicion, expertise, and understanding.







