Abstract
Background and aims: Human papillomavirus (HPV) is a sexually transmitted infection linked to genital, anal, and oral warts, as well as cervical and other cancers. Low- and middle-income countries, such as Nigeria, face heightened HPV-related disease risks. Vaccination is crucial for global burden reduction, especially in these regions. This study assessed the knowledge, attitudes, and preventive practices concerning HPV infection and vaccination among mothers of adolescent girls in Lagos, Nigeria.
Materials and methods: A descriptive cross-sectional study was conducted in Lagos. Using multi-stage sampling, 312 mothers of adolescent girls attending secondary schools were selected. Data was collected through self-administered questionnaires and analysed using SPSS Statistics.
Results: Most respondents were aged 40–49 (53.5%) and married (81.1%). Only 43.9% had heard of HPV, although the majority were aware of cervical cancer. A majority (59.0%) had not heard of HPV vaccines. Most respondents demonstrated poor HPV knowledge (61.9%), though many were willing to vaccinate their daughters if free (69.4%). However, fewer were willing to pay for vaccination (47.7%), and most daughters (85.6%) hadn’t been vaccinated. School-based vaccination programmes were the primary source of vaccination information (81.3%). Significant associations were found between respondents’ level of education and their HPV knowledge, as well as willingness to vaccinate their daughters (p<0.001, 0.008).
Conclusion: The study reveals significant knowledge gaps among respondents regarding HPV and cervical cancer, indicating poor HPV-related knowledge and practices in Nigeria. To address this, broad awareness programmes, health facility outreach, media campaigns, and improved vaccine accessibility through government support are recommended.
Key Points
1. Low- and middle-income countries like Nigeria bear the greatest burden of human papillomavirus (HPV)-related diseases, such as cervical cancer. Vaccination is a key prevention strategy, and maternal awareness is important for this.
2. A cross-sectional study of Nigerian mothers to assess their knowledge, attitudes, and preventive practices regarding HPV vaccination for adolescent girls.
3. Educating mothers and improving access to HPV vaccines through media campaigns, global health partnerships, and school-based vaccination programmes are ways to increase vaccine uptake and reduce the burden of HPV-related diseases in Nigeria.
INTRODUCTION
Human papillomavirus (HPV) is a sexually transmitted infection of the Papovaviridae family that infects humans, particularly the skin and mucous membrane of the genital, anal, or oral cavities. This infection can lead to warts (papillomas) and a variety of neoplasms, especially cancer of the uterine cervix in women, as well as a significant proportion of anogenital (vulvar, vaginal, penile, and anal) and oropharyngeal cancers.1 Most HPV infections resolve within 12–24 months of infection and do not result in symptoms or illness.2 The majority of people are infected through sexual contact.3 At some point in their lives, most individuals who are sexually active will be infected with HPV, and some may be repeatedly infected. About 90% of infections are cleared eventually, while they persist in the other 10% and put them at an increased risk of developing cancer. Of the 10%, half develop malignancy by the end of the 30th year of persistent high-risk HPV infections.4 HPV is the most common viral infection of the genital tract.5 Over 130 different HPV types have been identified, and they are divided into low- and high-risk categories based on their potential for oncogenesis in the presence of persistent infection.4 Of the several high-risk HPV types, two (16 and 18) are responsible for over 70% of all high-grade cervical pre-cancers.6,7 Among the more benign HPV-associated conditions, genital warts are unambiguously linked to HPV-6 and -11.6 Studies show the global prevalence of HPV infection to be about 11–12%, with the highest rates in sub-Saharan Africa, Eastern Europe, and Latin America.8 In Nigeria, cervical cancer, primarily caused by HPV, is the most common gynaecological cancer, with over 12,000 new cases annually and over 7,000 deaths each year.9 This contributes to approximately 11% of new cases diagnosed in sub-Saharan Africa.10 Nigeria also ranks fifth among countries with respect to death count from cervical cancer, after India, China, Brazil, and Bangladesh.11 This high burden underscores the critical need for effective HPV vaccination strategies.
Despite these figures, only 3% of 10–20-year-old females in low- and middle-income countries (LMIC) are vaccinated against HPV, compared to 34% in developed countries.12 Previous research in Nigeria shows varying HPV prevalence rates, with one study in the southwest reporting 18.6%,13 and another reporting 36.5% among women attending outpatient clinics in Lagos, Nigeria.14 The significant contribution of high-risk HPV types to overall cases, and the particularly high burden in LMICs that have low vaccination rates, is a cause for concern.15 These statistics reflect a significant public health challenge, particularly in developing countries like Nigeria.
Cervical cancer prevalence has declined in developed countries due to effective screening methods like DNA testing and cytology, which are largely unavailable in developing countries.16 Sub-Saharan countries also have the lowest proportion of screened women among LMICs.17 Vaccination against HPV is therefore a crucial primary prevention strategy and has showed significant reductions in the prevalence of high-risk HPV types, especially among young females.18
Vaccination uptake is influenced by parental knowledge and attitudes, especially mothers,19 yet studies indicate a low level of awareness about HPV and its vaccine among Nigerian women, including university students.20 This gap in knowledge contributes to low vaccination rates and high cervical cancer incidence.
Given that the WHO recommends HPV vaccination for girls aged 9–13 years,21 it is critical to understand the role of mothers, who primarily care for children in this age range, in vaccine uptake. This study seeks to assess the mothers’ knowledge, attitudes, and preventive practices concerning HPV infection and vaccination among adolescent girls in Lagos.
By identifying barriers and facilitators to vaccination, the study hopes to inform targeted interventions that can improve vaccine coverage and lower the burden of HPV-related diseases in this high-risk population, ultimately contributing to a reduction in cervical cancer incidence and mortality.
MATERIALS AND METHODS
Study Design
This is a descriptive cross-sectional study designed to assess the knowledge, attitudes, and preventive practices regarding HPV vaccination among mothers of adolescent girls in selected secondary schools in Lagos.
Setting
This study was carried out in Lagos, with an estimated population of 24.6 million people in 2015, making it the largest city in Africa. Ikeja, which lies at the centre, is the capital of Lagos State. Lagos State has six education districts, and Education District VI is divided into three administrative zones, which are Ikeja, Mushin, and Oshodi/Isolo, with a total of 106 secondary schools.22 Data collection was done in January 2024 in the selected schools. Ethical approval was obtained from the Health Research and Ethics Committee of Lagos State University College of Medicine.
Participants
- Eligibility criteria: participants included in the study were mothers of female secondary school students in the Ikeja Local Government Area aged 9–14 at the time of the study.
- Selection of participants: a multi-stage sampling technique was employed. Two secondary schools were chosen by simple random sampling from the list of secondary schools within Ikeja Local Government Area. One school is located in an urban area with a higher average household income, and it predominantly serves children from middle- to upper-income families. The second school, in a rural area, predominantly serves students from lower-income households. For each selected school, 8 classes were randomly chosen out of 20, and the mothers of all female students in these classes were invited to participate in the survey. Three hundred and twelve mothers accepted the invitation. Informed consent was obtained from all participants, and confidentiality and anonymity were ensured.
Variables
- Outcomes: the main outcomes of interest include knowledge, attitudes, and preventive practices related to HPV vaccination among mothers.
- Exposures: socio-demographic factors (age of respondents, level of education, occupation, marital status, ethnicity, religion), and overall HPV knowledge.
Data Sources/Measurement
- Sources of data: data were collected using a semi-structured, self-administered questionnaire. This questionnaire was pretested and adapted after reviewing existing literature on the subject.
- Methods of assessment: the questionnaire is comprised of four sections: socio-demographic data, knowledge on HPV infection and vaccination, attitude towards HPV vaccination, and HPV prevention practices.
Bias
To reduce courtesy bias, participants were assured of anonymity and confidentiality, ensuring their responses were genuine. Additionally, the questionnaire was refined after conducting a pilot test to minimise recall bias. This ensured that questionnaire items were clear, concise, and easy to interpret. A “don’t know” option was also included for questions where respondents might be unable to recall specific information, allowing them to accurately report their level of knowledge or experience.
Study Size
The calculated sample size for the study was 310 participants, determined using Cochran’s formula for descriptive studies, n=Z2Pq/d2.
Where n: sample size, Z: z-score at 95% confidence level, P: prevalence of attribute among the population, q: 1–P, d: desired level of precision (0.05), and P=28% (proportion of population who have knowledge on HPV).23
Quantitative Variables
Quantitative variables were handled in the analyses using descriptive statistics, including frequency tables, means, and standard deviations. Statistical Package for the Social Sciences software (SPSS Statistics version 26, IBM, Armonk, New York, USA) was utilised for data analysis.
Statistical Methods
The statistical relationship between categorical variables was examined using Chi-square test or Fisher’s exact test, as appropriate. Descriptive statistics were used to summarise the data. Nine questions from the knowledge section of the study questionnaire were scored and used to evaluate the participants’ overall knowledge about HPV infection and vaccination. Thus, respondents were classified based on how many questions were answered correctly, with poor knowledge being equal to a score of 0–3, 4–6 as fair knowledge, and 7–9 as good knowledge.
RESULTS
The socio-demographic data of the respondents is presented in Table 1. Three hundred and twelve mothers were surveyed, they had a mean age of 42.03±6.3, and most (81.1%) of the respondents were married. The knowledge of mothers on HPV infection and vaccination is also depicted in Table 1. Less than half (43.9%) of the respondents had heard about HPV, and the proportion of respondents aware of HPV vaccines (35.6%) was even smaller (Table 1).
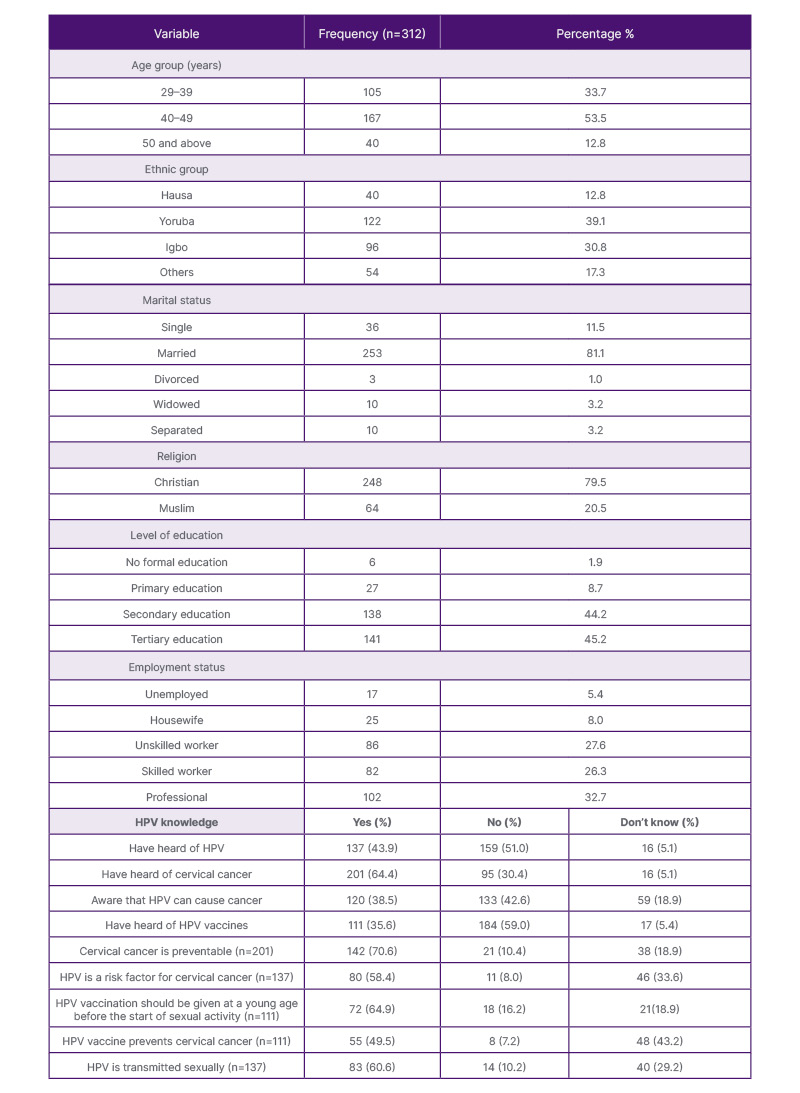
Table 1: Socio-demographic data and human papillomavirus knowledge of respondents.
HPV: human papillomavirus.
Table 2 contains the participants’ overall knowledge about HPV infection and vaccination, which was evaluated by scoring nine questions on HPV knowledge. Therefore, this article classified poor knowledge as having a score of 0–3, 4–6 as fair knowledge, and 7–9 as good knowledge. A significant percentage (61.9%) of respondents demonstrated poor overall knowledge of HPV. The attitudes of mothers towards HPV vaccination and their preventive practices are also presented (Table 2). Only 5.1% (16/312) of the daughters of respondents have been vaccinated. Most of the respondents with vaccinated daughters learned about and arranged for vaccination through school-based vaccination programmes (81.3%).
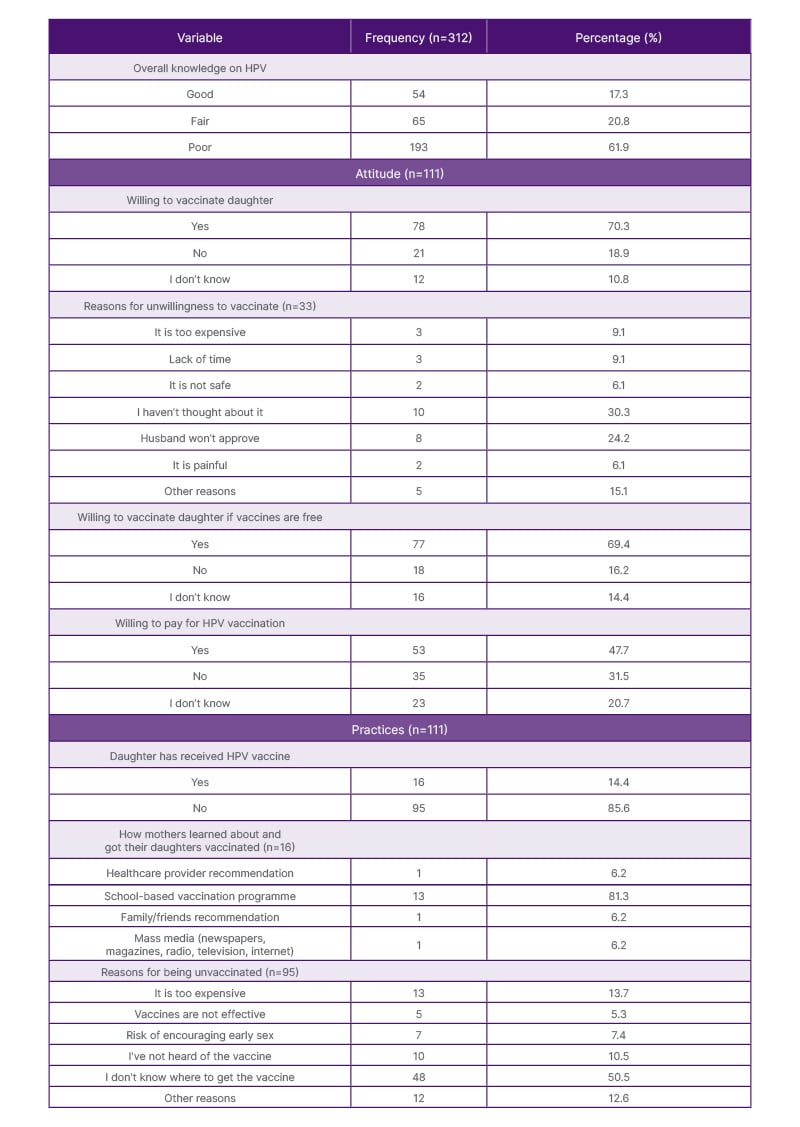
Table 2: Overall knowledge, attitudes, and practices of respondents regarding human papillomavirus vaccination.
HPV: human papillomavirus.
Table 3 shows that there was a statistically significant association between the level of education of respondents and their knowledge of HPV infection and vaccination (p<0.001), and also between occupation and knowledge of HPV infection and vaccination (p<0.001). A statistically significant relationship between respondents with vaccinated daughters and their ethnicity (p=0.042) was also found (Table 3).
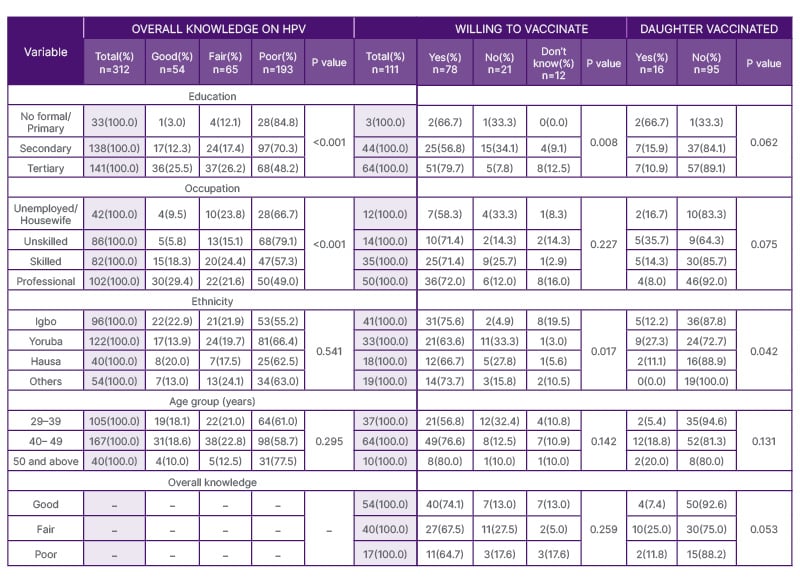
Table 3: Factors associated with mothers’ overall knowledge on human papillomavirus, willingness and vaccination status of their daughters.
HPV: human papillomavirus.
DISCUSSION
Public awareness of HPV and vaccinations is crucial to reducing the burden of cervical cancer in Nigeria. Therefore, this study aims to explore the knowledge, attitudes, and preventive practices regarding the virus. In this study, 64.4% of 312 participants surveyed were aware of cervical cancer, but only 43.9% had heard of HPV. This is consistent with findings from a community-based study assessing the HPV knowledge of mothers and their willingness to vaccinate their adolescent daughters in Shomolu, Lagos, that revealed a greater familiarity with cervical cancer compared to HPV.23 Similarly, a study assessing HPV awareness and uptake of cervical cancer screening among mothers of adolescentstudents in Abakaliki, Ebonyi State, reported only 42.8% awareness of HPV.24 This shows a gap in public knowledge concerning the virus despite a clear high level of awareness about cervical cancer.
Interestingly, 25.6% of participants recognised HPV infection as a risk factor for cervical cancer in this study. This is a slight decrease from the 29.1% awareness found in an earlier study investigating the level of knowledge and acceptability of HPV vaccination among women attending a gynaecology clinic at the Lagos University Teaching Hospital.25 This suggests that more efforts are needed to raise public awareness regarding HPV’s association with cervical cancer. Notably, respondents in that study and another conducted in Lagos selected mass media as their main source of information.23 The majority (32.1%) of respondents in this article cited health professionals as their singular primary source of information. However, mass media (print, broadcast, and internet) combined to surpass this with 44.5%, emphasising its crucial role in disseminating knowledge about HPV infection and vaccination.
In this study, 35.6% of participants were aware of the HPV vaccine, an almost two-fold increase from the study at a gynaecology clinic in Lagos, where awareness stood at 18.9%.25 This is an encouraging finding, as a study that reviewed the acceptability and readiness for introducing HPV vaccines in sub-Saharan Africa highlighted that increased knowledge is essential for the successful implementation of a widespread vaccine programme.26 While integrating the HPV vaccine into the National Programme for Immunisation schedule is a welcome development, previous research has shown that culturally appropriate health promotion efforts are necessary to enhance understanding and uptake.27
Encouragingly, 70.6% of mothers in this study who knew about cervical cancer recognised that it could be prevented and that vaccines were beneficial for this. This is similar to findings of a study in Western Nigeria evaluating the factors influencing parental willingness to vaccinate adolescent daughters against cervical cancer, where 62% of participants had the same awareness.28 In addition, 64.9% of the vaccine-aware population agreed that it should be given at a young age before the onset of sexual activity, which is much higher than the 48.1% found in another Lagos study.23 This increase could be due to the greater proportion of respondents with higher education, who likely possess a better understanding of cervical cancer prevention and the importance of early vaccination.
The proportion of respondents willing to have their daughters vaccinated was 25% in this study. A similar study among mothers in Southeast Nigeria reported a significantly larger proportion (84.6%) of mothers desiring vaccination for their daughters.29 Another study among medical and dental students in Benin City, Nigeria, also revealed that the majority had a positive attitude towards vaccination.30 The demographic differences between the participants in these studies may explain this. Among the respondents who expressed hesitation or unwillingness to vaccinate their daughters, the most common reason (30.3%) given was they had not previously considered vaccination.
The majority (69.4%) of the respondents expressed willingness to pursue vaccination if the vaccines were offered free of charge. However, this figure decreased to 47.7% with the option of payment, and this is likely to be similar in other parts of the country. This underscores the impact of vaccine cost on vaccination rates and echoes the findings of studies on HPV vaccination in Nigeria and sub-Saharan Africa, where the cost of the HPV vaccine emerged as a significant barrier.27,29 Global health partnerships between governments, international health organisations, and non-governmental bodies can help make HPV vaccines freely available or heavily subsidised, ensuring accessibility for all socio-economic groups.
This study revealed that only a minority of respondents’ daughters (5.1%) had received the HPV vaccine. A cross-sectional study among female undergraduates in Lagos found that a mere 1.1% of respondents had received the HPV vaccine.31 Similarly, findings among female secondary school students from Benin, Nigeria, show an extremely low vaccination rate (0.5%).32
Interestingly, a significant proportion (81.3%) of mothers with vaccinated daughters in this study reported learning about and facilitating their daughters’ vaccination through school-based programmes. This differs from research conducted in Beijing, China, where most recommendations came from family and friends, and only a few received recommendations from healthcare professionals.33 This exposes the potential of school-based programmes as an effective avenue to enhance HPV vaccination uptake and improve coverage in developing countries like Nigeria.
This study revealed that over half of the respondents with unvaccinated daughters (50.5%) cited a lack of awareness of where to get the vaccine as the primary reason for non-vaccination. This contrasts with a similar study conducted in Western Kenya among mothers of adolescent girls, where the high cost of vaccines and their non-availability were reported as the main hindrances.34 In a study among female public school teachers in Mushin, Lagos, a lack of awareness about the vaccine and its benefits was the primary reason cited by most (54.1%) for not vaccinating their children.35 This highlights the urgent need to disseminate information about HPV vaccines and provide accessible vaccination facilities for mothers to take their daughters. Policies and funding should be aimed at making vaccines as accessible to communities as possible, either through primary health care centres or secondary schools.
This study found significant associations between respondents’ level of education and their knowledge of HPV infection and vaccination, as well as between occupation and knowledge of HPV. Among those with tertiary education, over half (51.7%) demonstrated good or fair knowledge of HPV. This study also showed that respondents with professional occupations exhibited greater knowledge than others did. This greater HPV awareness is likely due to increased exposure to information sources during their education and better access to various sources of health information.
Factors such as age group and occupation did not significantly influence mothers’ attitudes towards vaccination. Instead, a statistically significant relationship was observed between respondents’ willingness to vaccinate their daughters and their ethnicity (p=0.017) and level of education (p=0.008). Specifically, a higher proportion of Igbo respondents and those with tertiary education expressed a willingness to vaccinate their daughters. This aligns with findings from a similar study in Lagos, which reported that mothers with a tertiary level of education had an almost 30-fold increased probability of vaccine acceptance.36 This highlights the pivotal role of increased female education in promoting vaccine acceptance.
Mothers’ education, occupation, and overall knowledge did not influence vaccination practices significantly. Notably, the number of respondents with secondary education who vaccinated their daughters was comparable to those with tertiary education. The lack of a significant difference between these two groups may indicate that awareness of vaccination does not always translate into action, possibly due to financial barriers. However, ethnicity also showed a significant association with vaccination status. These findings may reflect some innate cultural values, such as stronger health-seeking behaviour. The link between ethnicity and positive HPV attitudes and behaviours provides a basis for further research.
One limitation of this study is that there could have been some recall bias among respondents. Questions were pilot-tested, and a “don’t know” option was added to reduce guessing and inaccuracies. Mothers may have also shown some courtesy bias by providing responses they believe are socially acceptable. This was addressed by assuring respondents of anonymity and confidentiality to ensure genuine responses. Future studies may consider incorporating qualitative interviews to look into the reasons behind certain attitudes and practices, as the cross-sectional nature of this study limits the ability to establish a causal relationship between the variables examined.
CONCLUSION
Overall, this study highlights significant gaps in knowledge regarding HPV infection and its link to cervical cancer among respondents, as well as inadequate vaccination coverage in the country. It is therefore essential that initiatives focus on increasing HPV awareness, improving access to vaccination services, and prioritising HPV prevention efforts.







