Abstract
Background and Aims: Chronic pelvic pain (CPP) is a persistent pelvic pain that leads to reduced work performance and impaired quality of life in females. Nearly 15% of females report time off from paid work and around 45% report reduced work productivity. There is a paucity of studies to address the issue, especially with a multidisciplinary and multifactorial view. Various gynaecological disorders are associated with CPP such as endometriosis, adenomyosis, adhesions, chronic pelvic inflammatory disease, and pelvic congestion syndrome. The objective is to determine the frequency of CPP in females attending gynaecologic outpatient departments.
Materials and Methods: A total of 201 patients aged 14–48 years attending the gynaecologic outpatient department for gynaecological disorders with complaints of lower abdominal pain were included in this study. Patients enrolled in the study were assessed by a detailed history and pelvic examination, and a structured questionnaire was filled out. Data were analysed using the statistical package for social sciences version 23.0 (International Business Machines Corporation, Armonk, New York, USA).
Results: The mean age of the patients was 32.39±6.98 years. The frequency of CPP in females was observed as 95.52% (95% confidence interval: 91.67–97.93%) The rate of CPP was significantly high in females with parity ≤5 and those who had a duration of pain lower than 36 months. In multivariate analysis, adjusted odds ratio by stepwise logistic regression model showed that parity (parity 0–1) and duration of pain (≤36 months) were significantly associated with CPP in females.
Conclusion: The study indicates that the most common gynaecological causes of CPP in females attending the outpatient department were those with endometriosis followed by adenomyosis. The management of CPP needs patient-centred care with a multidisciplinary approach. This will lead to early and effective management.
Key points
1. Chronic pelvic pain (CPP) is an often ignored complaint that plagues females for years before a diagnosis is made. Patients are advised of many unnecessary investigations and treatments, which hinder proper care.
2. The authors’ research shows that most causes of CPP can be managed with a thorough and complete history. A multi-disciplinary approach is the best for such patients.
3. Physicians must have an open mind when patients present with CPP. Their concerns and fears should be validated and all-out efforts should be made to ease symptoms from this disregarded complaint.
INTRODUCTION
Chronic pelvic pain (CPP) affects up to 25% of females of reproductive age, and 15% of all females worldwide.1 It is a common complaint of females visiting the gynaecology outpatient department. The annual prevalence of CPP was found to be 38/1,000, a rate comparable to asthma (37/1,000) and back pain (41/1,000).2 Among sparse population-based studies, the prevalence of CPP was found to be 25.4% in New Zealand and 21.5% in Australia.3 Among South East Asian countries, a 44.2% prevalence of CPP was reported in Thailand.4 CPP is also one of the most frequent indications for gynaecological laparoscopies, accounting for approximately 40% of cases.5
CPP is defined by the Royal College of Obstetrics & Gynaecology (RCOG) as an intermittent or constant lower abdominal pain of greater than 6 months’ duration, not occurring exclusively with menstruation or intercourse and not associated with pregnancy.6 It arises from structures within the pelvis. The differential diagnoses of CPP include gynaecological causes (endometriosis, adenomyosis, adhesions, chronic pelvic inflammatory diseases, remnant ovary syndrome, trapped ovary syndrome, or pelvic congestion syndrome), gastrointestinal causes (irritable bowel syndrome, inflammatory bowel disease, or coeliac disease), urinary causes (interstitial cystitis or urethral syndrome), neurological causes (pudendal neuralgia, trigger points, or nerve entrapment), and musculoskeletal causes.7 The pain is caused by a single, or often a combination of different disorders with overlapping symptomatology, making it difficult to diagnose.
Patients with CPP have a long history of pain, marked psychiatric effects, work and physical impairment, and distrust of treatment,8 leading to a burden on healthcare expenditure and work productivity loss. Every year, 881.5 million USD is spent on outpatient department management in the USA, and an estimated 158 million EUR is spent on the UK National Health Service.5 In total, 550 million USD is lost each year in the USA due to absence from work.8 In the United Kingdom in 2001, 15% of affected females reported lost working days and 45% reported reduced working capacity. A study showed that 43% of individuals with CPP reported that their activities were restricted by pain.
Without a medical prescription, 58.4% of females use analgesics or nonsteroidal anti-inflammatory drugs weekly or daily for pain relief.5 Females who have had pelvic pain for longer develop strong associations with disability, distress, poor general health, low satisfaction levels, a sense of helplessness, and negative coping responses.9,10 The purpose of this study is to obtain insight into the scope of a problem that leaves many females crippled with an often misunderstood diagnosis.
MATERIALS AND METHODS
This descriptive cross-sectional study was conducted at the Department of Obstetrics and Gynecology Unit-2 of Dr Ruth K.M. Pfau Civil Hospital Karachi, Pakistan, from March 2019 to January 2020. Data were collected from females attending the gynaecology outpatient department who fulfilled inclusion criteria, after taking their informed consent. Females aged 14–48 years with complaints of lower abdominal pain greater than or equal to 6 months’ duration were enrolled in the study. Menopausal females and those with a history of hysterectomy were excluded from the study. Age, parity, duration of pelvic pain, history of past sexual abuse, family history of CPP, education, marital status, employment status, use of pain-relieving medications, diagnosed gynaecological cause, and pain analysis on the visual analogue scale were recorded in a structured questionnaire.
Females who met the inclusion criteria were asked detailed questions to ascertain whether pain was of pelvic origin or due to other causes. Data were analysed using the statistical package for social sciences (SPSS) version 23.0 (International Business Machines Corporation, Armonk, New York, USA). The quantitative variables of age, parity, duration of pelvic pain, and pain score on visual analogue scale were represented by mean and standard deviation. The qualitative variables of ethnicity, history of past sexual abuse, family history of CPP, education, marital status, employment status, pain-relieving medications, and diagnosed gynaecological cause were represented as frequency and percentage.
Effect modifiers such as ethnicity, history of past sexual abuse, family history of CPP, education, marital status, employment status, pain relief, and diagnosed gynaecological cause were addressed through data stratification. A post-stratification chi-square test was applied, and a p-value ≤0.05 was considered significant.
RESULTS
A total of 201 patients with lower abdominal pain were included in the study. The mean age of the patients was 32.39±6.98 years. More than two thirds of these females were married (81.6%), 25 (12.4%) were single, 8 females were separated and 4 females were widows. Almost 55% of the females had multiparity. More than half (109; 54.2%) of the females were illiterate, 62 (30.8%) had attended primary education and 30 (14.9%) had attended secondary education.
Out of 201 patients, 192 (95.5%; 95% confidence interval: 91.67%–97.93%) had experienced CPP. Ten (5%) females reported sexual abuse and 65 (32.3%) patients had a history of pelvic pain complaints in the family. There were 128 (63.7%) females who used analgesics or nonsteroidal anti-inflammatory drugs for relief of pain, 44 (21.9%) females used hormonal methods for pain relief and 29 (14.4%) were taking other forms of medications and therapies for symptom control. Endometriosis (60; 29.9%) and adenomyosis (56; 27.9%) were the top two most common diagnoses in females.
Parity (parity ≤5) and duration of pain for less than 36 months were significantly associated with CPP in females, yet was not statistically significant with age groups, marital status, education, employment, past sexual abuse, family history of pelvic pain, use of pain-relieving medicine, and diagnosis, as shown in Table 1. In a multivariate analysis, adjusted odds ratio by stepwise logistic regression model showed that parity (parity 0–1) and duration of pain (≤36 months) were significantly associated with CPP in females, as shown in Table 2.
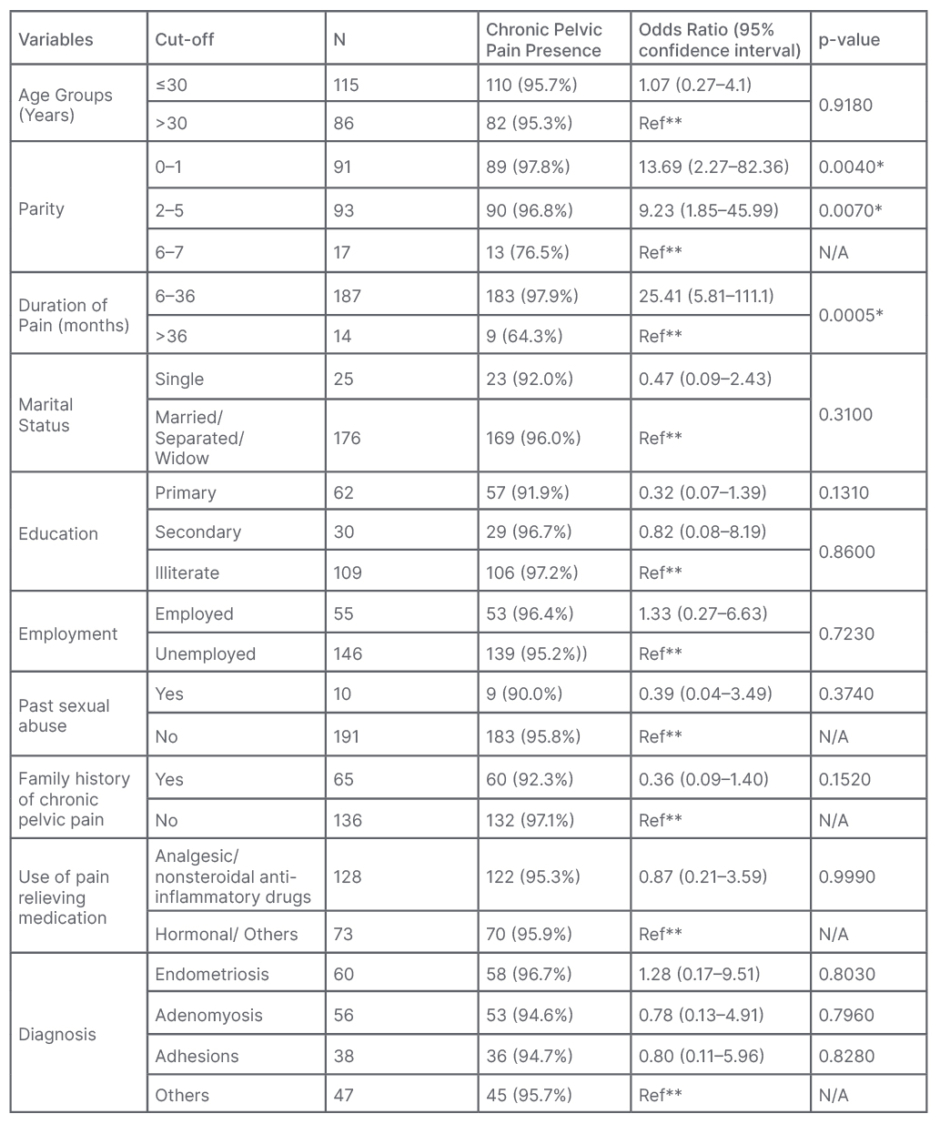
Table 1: Univariate analysis showing factors associated with chronic pelvic pain in females (n=201).
N/A: not applicable.
* Significant <0.01
** Reference group: comparison category equal to 1
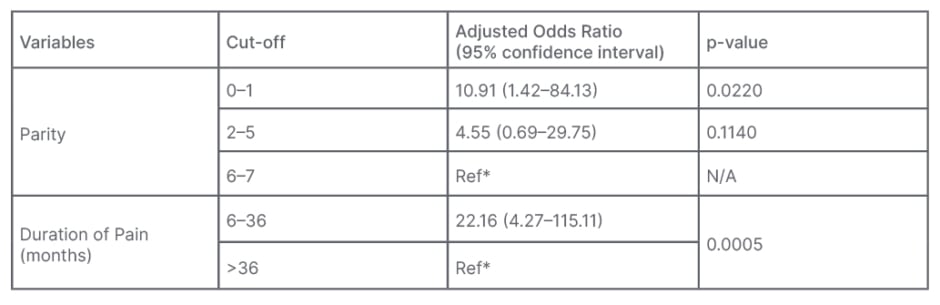
Table 2: Multivariate stepwise logistic regression model showing factors associated with chronic pelvic pain in females.
Model Accuracy: 96.5%
Nagelkerke R Squared: 0.341
Hosmer–Lemeshow Test: p=0.951
Age, education, marital status, employment, past sexual abuse, family history of chronic pelvic pain, use of pain-relieving medication, and diagnosis were excluded from the model. Stepwise Forward Wald logistic regression model was applied.
*Reference group: comparison category equal to 1
DISCUSSION
The quality of life of patients with CPP is severely affected, and current known therapies are adopted for relief from pain and an aetiological diagnosis. This imparts a huge burden on the healthcare system, as patients experience repeated hospital admissions, surgical procedures, and emergency and general physician visits to obtain a definitive diagnosis, as well as to relieve CPP symptoms causing distress, disability, and affecting daily activities.11-12 This also develops a strain in relationships and often requires absence from work.13,14
CPP has a multifactorial aetiology; therefore, a multidisciplinary approach is advised to reach a diagnosis. Treating patients with medical and surgical therapies, as well as reassuring them, gaining trust and providing psychological support for pain relief results in better cure rates compared to pharmaceutical and interventional options alone.15 One of the main causes of CPP is endometriosis, which can make management even more challenging. Illness imparted to the affected individual by pain intensity is ignored by many clinicians and endometriotic foci are put into consideration.16,17
Mood disorders such as anxiety and depression accompanying such a diagnosis have a negative impact on the perception of pain. These concurrent diagnoses of CPP, endometriosis, and mood disorders disrupt pain inhibitory pathways, which makes the patient more sensitive to nociceptive stimuli.17-19 These have a profound impact on the severity of pain, which is directly proportional to low output and absent days from work.20,21 Diagnostic delay is a significant factor and fatigue is a major complaint in direct correlation with the severity of pain, leading eventually to absenteeism from education, academics, and work. Social and sexual relations are impaired and patients live a socially isolated life.22 The miscommunication, inadequate treatment for relief of pain, and negative attitude by doctors can further aggravate detrimental psychological effects.23-25
In their study, Yasmin et al.26 demonstrated that 40% of laparoscopies performed for evaluation of CPP aetiology remained inconclusive. In such patients, other factors such as childhood sexual abuse and non-gynaecological pathologies should be considered. However, the reassuring effect of negative laparoscopy improved their quality of life. The authors did not perform any laparoscopies for the patients, which was a limitation of the study.26 Facchin et al.27 demonstrated in their study that mood dysfunction, anxiety, depression, and stress all negatively influence the immune system. The resulting imbalance between pro- and anti-inflammatory cytokines flares inflammatory response. A vicious cycle is started with increased disease severity and increased mental upset and depression. Therefore, the author insists upon psychological therapy along with medical and surgical treatment for better outcomes.27 The study conducted by Centini et al.28 suggests that when patients are reassured and made to understand their disease, they are found to get positive improvement in quality of life. Cognitive therapy is an integral part of CPP treatment. Reduced stress, reduced mental anxiety, improved quality of life, and feeling of well-being indirectly reduce ongoing stress response within their body and inflammatory process, and therefore the disease. Centini et al.28 divided patients with CPP into two groups, with and without endometriosis. They found that those with endometriosis generally had a poorer prognosis and a more severe disease overall. The authors made a similar observation intheir study.28
Petrelluzi et al.29 reported altered metabolism of cortisol, hypothalamic pituitary adrenal axis malfunctioning, and hypocortisolism in patients affected with chronic fatigue syndrome.29 Tripoli et al.30 stated that surgical and medical treatment for CPP is not sufficient. Other aspects should also be addressed to improve patient quality of life. Patients with CPP are frustrated and socially isolated, with disrupted marital and sexual life because of long intervals in achieving a definitive diagnosis. Sexual, social, psychological, emotional, and mental well-being is entirely neglected by physicians while treating underlying disorders, which is why optimal therapeutic results are not achieved.30
A significant amount of healthcare costs are borne by insurance companies and governments due to the extensive workup and continuous doctor’s visits needed for CPP.31,32 It also requires more frequent visits to the psychiatrist, and sometimes surgery such as a hysterectomy does not improve pain.33-35
If the underlying cause is endometriosis, it results in even more workup and reproductive challenges.36 There is a complex and altered interplay between the central and peripheral nervous systems for the generation, transmission, and aggravation of pain in endometriosis.37,38 The pain of endometriosis is resolved with hormonal treatment, but can recur as soon as therapy is stopped.39-42 Another significant cause of CPP is adenomyosis, which affects around 30% of females in their late reproductive years.43 Adenomyosis presents with abnormal uterine bleeding and chronic pelvic, but is not routinely diagnosed clinically or even radiographically. The diagnosis is mostly concluded from hysterectomy specimens.44,45
Mathias et al.46 reported that females older than 35 years of age are slightly less prone to the risk of developing CPP when compared to females of a younger age group. Females separated from their partners and widowed females were found to have an increased prevalence of CPP compared to single females.46 In the study conducted by the authors, over two thirds of females were married (81.6%). This raises the association of CPP with marital status. Mathias et al.46 found no significant relationship between the educational level of patients and CPP frequency in their study.
Facchin et al.,47 when observing an association between CPP impact on the employment status of affected females, found a potential connection between the severity of pain of endometriosis and unemployment and absence from work. Symptomatic patients with endometriosis were more likely to be unemployed compared to asymptomatic patients. The author concluded that severe incapacitating CPP caused by endometriosis disrupts patients’ professional life and career, and renders them helpless.47
Mackey et al.48 studied 262 participants with CPP. Compared to the control group, patients affected with CPP had lower literacy levels, lower monthly income due to unemployment, an inability to perform work, days off from work, and expenses on frequent physician’s visits. Associated co-morbidities were also more common in disease affected group.48
The highest pain intensity reported in the authors’ study was a visual analogue score of 8 (4% of patients) leading to an inability to perform at work, the feeling of helplessness about pain relief, and unemployment, as well as patients feeling unable to take care of family and to do household chores. Roth et al.49 studied the correlation between the level of educational achievement and pain perception, quality of life disruption, and disability. The study included a total of 187 participants. Educational achievement was grouped into five categories ranging from primary school to graduation level. A direct relationship was observed between higher educational levels and the severity of pain. The author concluded that greater educational status makes patients susceptible to perceiving the increased intensity of pain sensation, disability, and distress. The level of education was also found to be inversely related to favourable treatment outcomes. Roth et al.49 emphasised the importance of treating chronic pain with a bio-psychosocial approach that considers multidimensional aspects of clinical factors together with socio-economic parameters, which are beyond physiological impairment.49
Day et al.50 examined the association between demographics and psychosocial variables with chronic pain in 115 patients. The study illustrated that race and ethnicity could be potentially linked to pain severity and disability. Pain intensity score found was far greater in African-American patients compared to White Americans. The author reported satisfaction with living as a contributing factor to favourable pain tolerability and favourable treatment outcome scores in White Americans, whereas African-American patients were living in rural areas with low monthly income, poor socio-economic status, low literacy level, and poor access to appropriate treatment. All these factors played part in contributing to further aggravating their pain perception and associated illness. Life satisfaction plays a protective role against negative mindset and affectivity.50
The main limitation of this study was a limited sample size and sample collection from a single centre, which was a government-run hospital. The population presenting to the hospital belonged to the lower socio-economic class, hence some bias may be expected in the extrapolation of the results.
CONCLUSION
In conclusion, CPP is an important but overlooked health morbidity that has been disregarded for a long time. It has a huge impact and burden on healthcare economics, patient quality of life, and almost every aspect of the affected individual’s life. There is a need to emphasise effective management protocols, multidisciplinary and multi-dimensional approaches, and to aim every effort to obtain an accurate diagnosis for pelvic pain from the first day of presentation. This would avoid unending referrals, investigations, and procedures, and the trial of different and inappropriate therapies which often do not address the pathology for symptom relief. There is a need to allocate healthcare resources and address the disease in future research for better treatment and care of females with from debilitating diseases such as CPP.







