Abstract
Cutaneous squamous cell carcinoma of the hand with clinical perineural invasion is uncommon. This article describes a case of a 70-year-old female who presented with a small painful nodule on the dorsum of the left hand with minor skin surface changes who underwent excisional biopsy. A deep long subcutaneous cord was palpable extending proximally from the nodule. Intraoperative findings showed a tumour growing 2.5 cm along the dorsal cutaneous nerve of the hand, and histopathological examination revealed a primary well-differentiated squamous cell carcinoma with perineural invasion. This case highlights the importance of considering malignancy as a differential diagnosis when dealing with atypical lesions.
Key Points
1. Cutaneous squamous cell carcinoma of the hand with clinical perineural invasion is uncommon. Early detection and treatment of this malignant disease is vital to preserving the function of the hand, and hence quality of life.
2. This article describes a rare case of cutaneous squamous cell carcinoma of the hand presenting as a tender dermal nodule on the dorsum of the hand, with palpable extensive neural spread along an adjacent cutaneous nerve. It also discusses the different presentations of cutaneous squamous cell carcinoma, and the risk of perineural invasion and its implication.
3. Clinicians should be aware of the different possible presentations of cutaneous squamous cell carcinoma of the hand, and should have a high index of suspicion when dealing with atypical lesions of the hand.
INTRODUCTION
Cutaneous squamous cell carcinoma (SCC) contributes to 20% of non-melanoma skin cancers and early diagnosis is vital to reducing the risk of local and distant metastasis.1 Perineural invasion (PNI) is a well-established, high-risk feature in cutaneous SCC and is defined as the invasion of the space surrounding the nerve.2 Cutaneous SCC with PNI may present with neurological symptoms, including sensory changes, paraesthesia, pain, or paralysis.3 This article reports an atypical case of cutaneous SCC presenting as a tender dermal nodule on the dorsum of the hand, with palpable extensive neural spread along an adjacent cutaneous nerve.
CASE DESCRIPTION
A 70-year-old White female was referred by a dermatologist with a 6-month history of a painful and slow-growing nodule on the dorsum of their left hand. The patient had seen their general practitioner 2 months earlier, who performed an ultrasound scan of the lesion showing a hypoechoic structure that could be characterised as a neuroma. A shave biopsy of the skin overlying the nodule had been done; it was not sufficient to diagnose the nature of the lesion, showing only solar keratosis. The patient’s past medical history included previous surgical excision of a left medial forearm SCC and a chest wall basal cell carcinoma. They had Fitzpatrick skin Type II with no significant history of sun exposure.
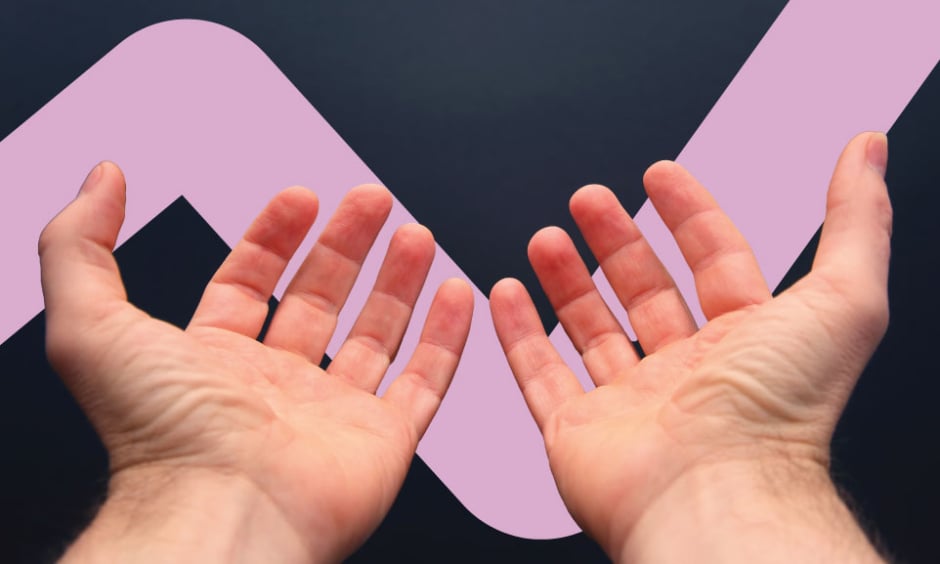
Physical examination revealed a tender 12 mm subcutaneous nodule on the dorsum of the left hand, associated with sensory loss in the fourth web space. There was no axillary lymphadenopathy. Based on the examination findings, the differential diagnoses included a neural lesion, glomus tumour and malignancy. The patient underwent excisional biopsy with flap repair surgery. The operative findings at surgery revealed a visible neural tumour growing along the dorsal cutaneous nerve over a distance of 2.5 cm (Figure 1 ) that was resected to the depth of bare extensor tendon. Histopathological examination demonstrated a primary well differentiated SCC involving the deep and transverse margins, with perineural invasion and probable complete intraneural obliteration by the SCC (Figure 2 ). A further wide excision of the lesion was considered; however, to avoid potential compromise of the extensor apparatus, the patient was referred for radiotherapy.

Figure 1: Intraoperative photograph of the tumour growing along the dorsal cutaneous nerve of the hand (yellow arrows), and macroscopically normal dorsal cutaneous nerve (blue arrows).
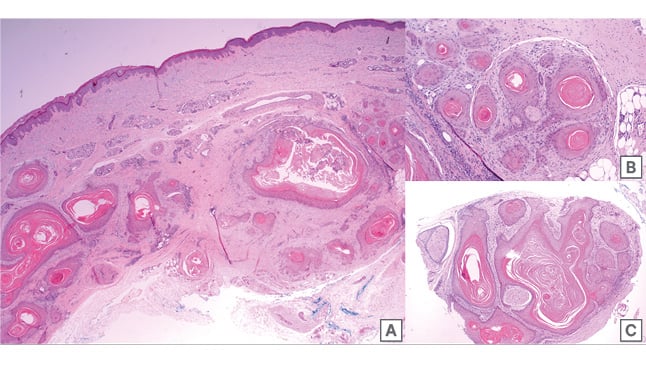
Figure 2: Histopathologic photographs of the left dorsal hand nodule using a haematoxylin and
eosin stain.
A) 2x: excisional skin biopsy showing SCC infiltrating through full thickness skin.
B) 10x: photograph at high magnification showing 0.1mm diameter nerve in centre surrounded by SCC.
C) 4x: photograph of the detached subcutaneous nerve (top left and centre left) showing complete intraneural obliteration by SCC.
SCC: squamous cell carcinoma.
At the 1-month follow up appointment, prior to radiotherapy, the patient noticed a small lump growing adjacent to the surgical site, with a punch biopsy revealing recurrence of the SCC. The patient then underwent wide local excision of the entire wound and large split skin graft repair. Histopathology confirmed no residual SCC, and the further excised segment of nerve showed no tumour proximally or distally. No post-operative radiotherapy was felt indicated at this stage due to adequate surgical clearance.
At follow-up, the graft healed well, and the hand returned to full normal function. There were no signs of local recurrence and no lymphadenopathy of the axilla at the 12-month interval. The patient will continue follow-up with their dermatologist for ongoing surveillance.
DISCUSSION AND CONCLUSION
Cutaneous SCC is the most common malignancy of the hand, and typically presents on its dorsal surface.4 One study has reported that cutaneous SCC affecting the hand bears a higher recurrence rate when compared to other body sites.5 Atypical presentations for hand SCCs have been previously reported in the literature. Both Fisher et al.6 and O’Sullivan et al.7 have reported cutaneous SCC of the hand presenting as a chronic wound infection on both the right index and left ring finger, which failed to respond to treatment in a 33-year-old and 43-year-old male, respectively. In both cases, histopathology showed well differentiated cutaneous SCC with no PNI reported. In addition, cutaneous SCC of the hand has been reported to disguise as an infected epidermal cyst.8
Cutaneous SCC with PNI is considered a high-risk skin cancer with a poorer prognosis. Leibovitch et al.2 has reported the incidence of PNI in cutaneous SCC to be 4.7% in primary lesions. The presence of PNI is associated with increased recurrence rate and increased lymph node metastasis rate.3,9 Furthermore, SCC with PNI have a 3-year disease-specific survival rate of 64% compared with 91% for SCC without PNI.10 There are certain tumour characteristics that increase the risk of PNI; these include tumour size greater than 2 cm, SCC in the head and neck region, male gender, recurrent disease, and immunosuppression.2,3
Cutaneous SCC with PNI can present with neurological symptoms with no obvious skin lesion resulting in misdiagnosis and delay in treatment. A case has been reported in a 75-year-old male who initially presented with nasal blockage, right-sided face pain, and right eye ptosis was misdiagnosed as sinus infection and Bell’s palsy. After multiple investigations, including MRI, histopathological confirmation was taken from a scaly skin patch on the right cheek, which showed a moderately differentiated cutaneous SCC with PNI.11
The location of the tumour in this case was unusual for cutaneous SCC presenting as clinical PNI; such lesions are commonly found in the head and neck region.2 Most cases described in the literature involved the trigeminal nerve, followed by the facial nerve.3 The authors are not aware of any previously reported case of cutaneous SCC of the hand presenting with neural dysfunction related to PNI. Karia et al.3 have demonstrated that the presence of clinical PNI increases the risk of local recurrence of cutaneous SCC compared to those with incidental PNI, as well as increasing the risk of death. Therefore, SCC of the hand with clinical PNI is considered high-risk skin cancer, and ongoing surveillance is recommended.
In conclusion, cutaneous SCC with clinical PNI of the hand is uncommon. In this case, the initial shave biopsy was inadequate to exclude a diagnosis of cutaneous malignancy and the lack of apparent cutaneous lesion may have been misleading. Notably, the cutaneous SCC was growing along the dorsal cutaneous nerve of the hand forming a subcutaneous cord. Early diagnosis was essential to achieve a positive outcome for the patient. Clinicians should be aware of the different possible presentations of cutaneous SCC of the hand and should have a high index of suspicion, especially when assessing a patient with a nodule associated with neurological symptoms.