Interview Summary
Hyperpigmentation disorders, a group of common skin conditions characterised by darkened patches due to excess melanin production, affect a significant portion of the global population, with women more frequently impacted than men. They are a leading reason for dermatology visits, particularly among people with skin of colour. Risk factors include genetic predisposition, medication use, and sun exposure, with visible light (VL) playing a significant role. While not physically harmful, the conditions, which include post-inflammatory hyperpigmentation (PIH), melasma, and solar lentigines (age spots) can lead to psychological distress and social stigmatisation. As such, they can have a significant impact on patients’ self-esteem and quality of life (QoL). Hyperpigmentation disorders are challenging to manage. Current treatments include over-the-counter and prescription oral and topical treatments, sunscreen, chemical peels, and laser therapy. However, all these treatments have limitations, and many are associated with side effects and complications, especially in darker skin tones. Hydroquinone, the gold standard of hyperpigmentation management for decades, for example, can cause erythema, desquamation, and a burning sensation, and longterm use of high-concentration hydroquinone can result in exogenous ochronosis. In addition, chemical peels and laser therapy can trigger both irritation and PIH. Isobutylamido-thiazolyl-resorcinol (Thiamidol), a tyrosinase inhibitor identified using recombinant human tyrosinase, is a promising addition to traditional treatments. It has shown efficacy in reducing hyperpigmentation with a good safety profile. As such, it has potential to enhance a holistic approach to hyperpigmentation disorder management. Here, Thierry Passeron, University Hospital of Nice, France; Ncoza Dlova, University of KwaZulu-Natal, Durban, South Africa; and Vasanop Vachiramon, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand, talk about the evolving hyperpigmentation management landscape. They outline the impact, aetiology, pathophysiology, and current treatment approaches for hyperpigmentation disorders. They summarise the evidence base for Thiamidol and, reflecting on their own research and experience, they also explain how and why they are using the ingredient to enhance the management of hyperpigmentation in routine practice.INTRODUCTION
Pigmentation disorders (PD) are common. A global survey of 48,000 people across 34 countries conducted between December 2022–February 2023 found that as many as 50% of the global population reported suffering from at least one pigmentation disorder. Women, the survey reported, were affected more frequently than men.1
While hypopigmentation refers to lightened areas of skin, hyperpigmentation describes darkened patches or lesions caused by the excess production, distribution, or transport of melanin.2 “Hyperpigmentation is one of the most common causes of dermatology visits, particularly in patients with skin of colour,” said Dlova.
Common hyperpigmentation disorders include PIH, melasma, solar lentigines, and ephelides (freckles).2 These conditions vary in appearance, have varying aetiologies, and their frequency depends on skin type (see Table 1), which is usually defined as per the Fitzpatrick scale of response to ultraviolet (UV) exposure:2
- Fitzpatrick skin Type I: white, very fair skin; red or blonde hair; blue eyes; freckles
- Fitzpatrick skin Type II: white, fair skin; red or blonde hair; blue, hazel, or green eyes
- Fitzpatrick skin Type III: cream white, fair skin; any eye or hair colour
- Fitzpatrick skin Type IV: brown skin (typical of Mediterranean descent)
- Fitzpatrick skin Type V: dark brown skin (typical of Middle Eastern descent)
- Fitzpatrick skin Type VI: black skin
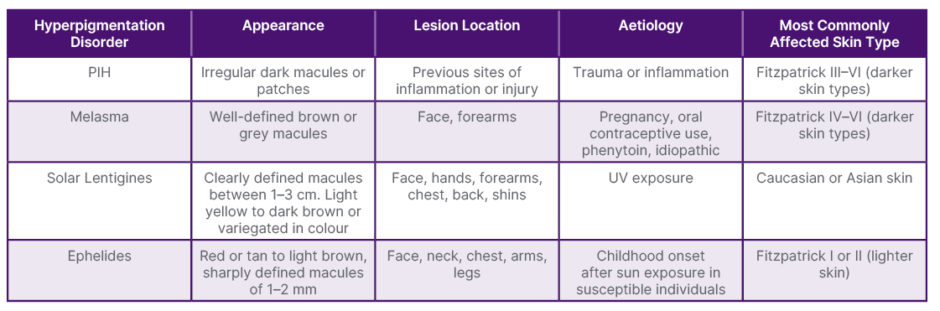
Table 1: Types of hyperpigmentation disorder and susceptible populations.2
PIH: post-inflammatory hyperpigmentation; UV: ultraviolet.
PDs can have a significantly negative impact on QoL.1 Almost a third (28%) of the 48,000 people who responded to the global survey described above reported a Dermatology Life Quality Index (DLQI) score of >10 out of 30, indicating their lives were severely affected by their skin disease, with 44% saying they felt they had to conceal visible areas of affected skin.1 Passeron, who was part of the study team, said that melasma was the hyperpigmentation disorder with the highest impact on QoL. “The impact is highly dependent on culture and background,” he said, explaining that the impact can vary a lot depending on the patient. “It can be stigmatising. People say they feel dirty, and that their friends and family like them less because of the lesions,” he added. Dlova said people living with PIH and melasma often felt frustrated, stressed, or embarrassed. “They do not like having to wear makeup on a daily basis to camouflage melasma,” she said. “Some avoid taking pictures when they are with friends or sharing pictures on social media because they are very conscious of pigmentation disorders.” Vachiramon said such disorders could be particularly impactful for people in public-facing occupations. “While it is not harmful to your general health, it can lead to a loss of confidence. I have one patient with melasma who is an actor, and he has to conceal his affected skin. He has to wear make up every day, which is very difficult for him,” he explained.
HYPERPIGMENTATION: RISK FACTORS, AETIOLOGY, AND PATHOPHYSIOLOGY
The leading risk factors for hyperpigmentation disorders are genetic predisposition; medication side effects, such as antibiotics, oral contraceptives, antimalarials, and tricyclic antidepressants; and sun exposure.3 Importantly, blue light, or VL, plays a key role in the development of melasma and PIH by worsening lesions.4
Hyperpigmentation disorders have varying aetiologies and pathophysiologies. In those who are genetically predisposed to PIH, for example, dark patches can develop following skin inflammation or injury.3 Typical triggers of excess melanin production that lead to PIH include burns, wounds, acne, and other inflammatory dermatoses.3 Solar lentigines (age spots) and ephelides develop after sun exposure.2 Melasma, a chronic condition that can last for 10–20 years, with regular relapses during this time,5 has a very complex, multifaceted pathophysiology. Traditionally, it was thought to be closely related to pregnancy and oral contraceptives. However, only around 20% of cases start during pregnancy, and the impact of oral contraceptives appears to have only a weak influence on disease evolution,5 said Passeron. Onset is earlier in lighter skin types, and may occur later, sometimes post-menopausal, in Types V and VI.5 “The darker the skin, the later the melasma starts,” Passeron said, adding that vascularisation also plays a role, and there is increasing evidence to show that melanocytes are not the only cells involved in the development and relapse of the condition.5. Fibroblasts and sebocytes, he explained, play a key role. “Pregnancy is far from being the only thing at play here,” he added.
CURRENT TREATMENT LANDSCAPE AND UNMET NEEDS
Hyperpigmentation treatment “can be a challenge”, said Dlova. “It takes time, and treatment may be ineffective in some individuals. Sometimes there is only partial reduction of the pigmentation; however, patients are looking for complete clearance, and sometimes that is impossible.”
The first step is accurate diagnosis and an understanding of the individual patient, she went on. “You need to know what is causing the pigmentation. Is an underlying disease causing inflammation, and therefore pigmentation? Is it a pigment disorder, like melasma? How deep is the pigmentation? Look at the occupation of the patient and where they live: are they exposed to the sun a lot?” Vachiramon reiterated the patient-centric approach. “When you deal with a person who has this condition, you have to really understand what the exact cause of the hyperpigmentation is, because we approach treatment in different ways,” he said, going on to explain that the appearance of the lesions will guide diagnosis (see Table 1).
In most cases, advising the use of over-the-counter topical treatments, or cosmeceuticals, and protective sunscreen will be the first course of action. All three doctors emphasised the importance of products that block VL as well as UV light. “Sunscreens are used to minimise the pigmentation and enhance the efficacy of other topical creams,” said Dlova. “VL has been shown in the literature to trigger or exacerbate pigmentation in patients,3 so we need to make sure the product has protection against VL, yet most sunscreens do not.” When choosing a sunscreen, then, patients cannot rely solely on sun protection factor (SPF), which is a measure of how well it will protect the skin from UVB rays, said Passeron. “So far, the only way to protect against VL is to use a tinted product e.g., that contains iron oxide,” he said. His recommendation was to use a tinted sunscreen with high UVA and UVB protection, at the equivalent of a teaspoon’s worth on the face. He did, however, recognise the limitations of this approach. “That’s fine if you have an intermediate skin tone, but not if you have very light, Asian, or darker skin,” he said, explaining that appropriately-coloured tinted sunscreens were lacking for these patient groups. Wearing a tinted cosmetic over the top of a high-protection UVA/UVB product can be a useful solution for some people with darker skin tones. However, the regimen can be time-consuming and burdensome. “People have to do it every day, and reapply during the day,” Passeron added.
Patients also need to be prepared for what lies ahead, particularly in melasma, said both Passeron and Vachiramon. “In the case of melasma, we need to remind people that this is a chronic disease that we cannot cure, and that can last 10–20 years,”5 said Passeron. “We need to really explain the crucial role of predisposing factors, especially sun exposure, in worsening melasma, and we need to tell them that they must apply sunscreen all year round.” Vachiramon added: “You have to tell your patient to be very patient, and that the use of sunscreen is very important for the prevention of future relapses.” While a number of cosmeceuticals are available for melasma, cost can also be an important factor, particularly in under-resourced countries, Dlova went on. Many cosmeceuticals are marketed in small packs, which can be impractical for people with larger areas of hyperpigmentation, compounding a lack of affordability, she added. “You need to make sure they can afford the treatment.”
Medical Interventions
When people do not respond, or have an inadequate response, to cosmeceuticals and preventative interventions, dermatologists will tend to consider prescription approaches. There are a number of available treatments, many of which are often used in combination to target the cause of the hyperpigmentation, said Dlova. “We have a whole range of treatments for melasma and PIH. Some work together and have a synergistic effect,” she said. “You cannot only use one treatment. Depending on the pathogenesis of the disease, you have to target multiple pathways,” she went on. “In melasma, for example, you have to target the inflammation and inhibit the tyrosinase (the rate-limiting enzyme of melanin production), and there’s a whole vascular element to it as well. We have to use multiple treatments that target different pathogenic aetiologies.” Triple combination therapy (hydroquinone, retinoic acid, and corticosteroid) is the recommended treatment for melasma.2 Passeron explained that for melasma, the combination, often called the Kligman’s Trio, would usually be delivered for 3–4 months. The patient would be advised to use cosmetic agents and sunscreen as maintenance therapy for the rest of the year, with annual administration of the combination being advised if necessary. For those who do not respond well to combination therapy, chemical peels, as well as light or laser therapy, may be options.2
Unmet Needs
The range of unmet needs in hyperpigmentation management stretches right the way along the treatment pathway. Passeron pointed to the lack of tinted, VL-protecting sunscreen products that are suitable for people with very light, Asian, or black skin, and Dlova highlighted that in many parts of the world, hyperpigmentation treatments were considered cosmetic, and therefore not covered by health insurance policies.
There are also important safety concerns around triple combination therapy. It has been associated with side effects, including erythema, desquamation, and a burning sensation, and long-term use of high-concentration hydroquinone can result in exogenous ochronosis, which is a blue-black hyperpigmentation.6 Furthermore, the use of hydroquinone has been linked to a potential risk of drug-induced carcinogenesis, leading to the compound being banned as a cosmetic ingredient in Europe.6
Both chemical peels and laser therapy also have their limitations. Passeron said peeling agents should only be advised during the winter months and should be used “with great care” in darker skin tones as they can worsen or trigger PIH.7 In terms of laser therapy, Vachiramon said there was no standard guidance on its use, with clinicians being guided instead by best practice advice. In his practice, he would usually suggest the approach if topical therapies yielded inadequate results after 2–4 months, or in patients who were unhappy to wait for them to take effect. However, it “can make the condition worse”, he said, adding it can remove hyperpigmentation caused by conditions such as melasma and solar lentigines, but leave dark spots of PIH on the skin.8 “This is common, especially among darker-skinned patients,” Vachiramon said.
Enhancing the treatment of hyperpigmentation disorders, then, is a priority for many dermatologists.
OPTIMISING HYPERPIGMENTATION MANAGEMENT WITH THIAMIDOL
Inhibiting the activity of tyrosinase, the rate-limiting enzyme of melanin, has been described as the safest and most effective way to treat hyperpigmentation.9 Despite the safety concerns, hydroquinone has been a mainstay of this approach for decades. Other tyrosinase inhibitors, such as kojic acid and arbutin, have been developed, but, as Passeron pointed out, they have not been compared to hydroquinone in a clinical trial. According to Mann et al.,9 the compounds’ “unsatisfactory efficacy” is largely due to them being tested on the only commercially available active tyrosinase, which is isolated from the mushroom Agaricus bisporus. The differences between the mushroom tyrosinase and mammalian enzyme both in terms of catalytic activities and substrate specificities, are significant.9 Thiamidol, however, is the first tyrosinase inhibitor that has been identified using a recombinant human tyrosinase construct.9
Thiamidol has been shown to be safe and effective in various forms of hyperpigmentation.9,10 Data show it can visibly reduce the appearance of solar lentigines within 4 weeks, with some being indistinguishable from the normal adjacent skin at 12 weeks, for example.9 One study asked women with mild-to-moderate melasma to treat one side of their face with a formulation containing 2% hydroquinone, and the other with a formulation containing Thiamidol.10 At 12 weeks, modified Melasma Area and Severity Index (MASI) scores significantly improved on both sides, though by a significantly higher margin on the Thiamidol-treated side.10 The study also recorded that 79% of patients improved following treatment with Thiamidol, compared to 61% with hydroquinone.10 During treatment, no patients reported worsening of MASI on the Thiamidol side, while approximately 10% of patients saw worsening on the hydroquinone-treated side.10 Numerous studies have found Thiamidol to be well tolerated,9-11 and it has also been associated with QoL improvements.6,11 Vachiramon said: “I think this is one of the things we have been waiting for. We wanted something that worked very well, with fewer side effects, and I think that is what we get with this ingredient.”
Optimising Triple Therapy
In some studies conducted by independent researchers, Passeron said, Thiamidol has been shown to have similar efficacy as hydroquinone,6 but with a strong tolerance.9-11 As such, it has the potential to enhance existing hyperpigmentation treatment approaches. To investigate this hypothesis, his team carried out a 24-week, double-blind prospective randomised trial, comparing traditional triple therapy (the gold standard of melasma treatment since 1974) to a new trio that replaced hydroquinone with Thiamidol.6
A total of 40 participants living with melasma were randomised to receive either the new trio (0.1% Thiamidol, 0.1% retinoic acid, and 0.1% dexamethasone acetate) or traditional triple therapy (5% hydroquinone, 0.1% retinoic acid, 0.1% dexamethasone acetate). They applied the formulations, which were both prepared in the hospital pharmacy and had an identical appearance, to the whole face except the eye area, every evening for 12 weeks. Subjects in both arms were given the same volume of topical cream, in identical packaging, as well as SPF 50+ topical sunscreens to be applied until Week 24. The primary endpoint was a change in modified MASI (mMASI) score between baseline and Week 12. QoL, as measured by the Melasma Quality of Life scale (MelasQoL) score, was also assessed.
At Week 12, analysis included 20 patients in the traditional triple therapy group and 19 in the new trio group.6
At Week 12, there was an adjusted mean improvement in mMASI score of 63% from baseline in the new trio group. This compared to an improvement of 39% in the traditional triple therapy group. The adjusted mean difference between the groups was -1.49. While this did not reach statistical significance, as Passeron’s paper highlighted, the difference was clinically relevant. The adjusted mean improvement in the MelasQoL score at Week 12 compared with baseline was -12.57. This compared to a change of -6.66 in the traditional triple therapy group. Only the new trio group recorded a statically significant improvement of the MelasQoL.6
Passeron said: “We demonstrated that there was no statistical difference between the traditional trio and the new trio after 3 months. While there was a progressive worsening after cessation, there was no rebound, and this was similar in both groups.” Turning to tolerance, he said there was some irritation in both groups, but added that this was likely linked to the high concentration of retinoic acid.6
Based on these findings, Passeron’s department has removed the traditional trio from practice. Instead, the team is using the new trio, with a reduced 0.05% concentration of retinoic acid to improve tolerance, on the same basis as the traditional trio, i.e., 3 or 4 months a year, during the winter months, with recommendations for continuous use of sunscreen.
Asked why they had made the decision, he said the efficacy was at least as good as traditional triple therapy, but he found the tolerance to be much better. He also pointed to the QoL improvements seen in the study. “I think this really is an advance for the care of melasma,” he added.
The main limitation of Passeron’s study, the authors wrote, was that the majority of participants had lighter skin types. Only three participants had Type V skin, all of whom were randomised to the traditional trio group, and none had Type VI.6
Managing Hyperpigmentation in Skin of Colour
Hyperpigmentation can be particularly challenging to manage in skin of colour. Many common treatments, including hydroquinone, chemical peels, and laser therapy, can all induce PIH, particularly in Fitzpatrick skin Types IV–VI. 11 A review of trials of Thiamidol in melasma and acne-related PIH in skin of colour, published in 2024, concluded it was safe, effective, and a “reliable hyperpigmentation management option in this patient group”.11
A total of 234 participants, 232 of whom had skin of colour, took part in the four studies (three randomised controlled trials and one observational real-world study) reviewed in the paper. Of these, 141 had melasma, and 93 had acne-related PIH. All studies demonstrated that Thiamidol effectively reduced hyperpigmentation in both melasma and PIH, without “causing sensitivities which bear the risk of PIH”. One, an observational study of participants with skin Types V and VI, found that the treatment significantly lightened hyperpigmentation in the affected areas, without lightening the surrounding skin. This, wrote the authors, underlined that Thiamidol’s mode of action was gentle, without bleaching properties.11
Dlova, who conducted the observational study included in the review, said she had found the treatment to be especially effective in acne-related PIH. In the study, 32 participants with skin Types V (n=24) and VI (n=5) used the study skincare regimen of three Thiamidol-containing products (day cream SPF 30 and dual serum in the morning, and night cream before bed) every day for 12 weeks. They were asked to refrain from using any other skin products, except cleanser and sunscreen. Clinical grading of efficacy and irritation, as well as patient-reported assessments, were carried out at baseline and Weeks 4, 8, and 12. At 4 weeks, melanin index score of lesions was lower than at baseline (654.1 versus 733.4). At Week 8, researchers recorded a score of 656.7, and at the end of the treatment period, a score of 632.7. In addition, melanin index only significantly lowered in lesional, not peri-lesional skin, resulting in a more even skin tone, rather than undesired lightening of dark skin tone. Improvements were statistically significant for all points in time when compared to baseline (p<0.001). Skin evenness, as assessed by the investigator, improved by 13.8% at 4 weeks, 51.7% at 8 weeks, and 89.7% at 12 weeks. In addition, the proportion of participants agreeing with the statement ‘my dark spots appear less pronounced’ was 86.2% at 4 weeks, 89.7% at 8 weeks, and by the end of the study, 100%. In addition, overall tolerability was graded as excellent.12
Based on these and previous efficacy and safety data, Dlova said she now recommends Thiamidol in routine practice, particularly for acne-induced PIH, and explained that she had seen similar results in the clinic as those she observed during the trial.
In melasma, she feels it has potential to be used in combination with other available agents. “Thiamidol inhibits tyrosinase, but melasma is not just about that. There is an inflammatory component and there are other issues in the pathogeneses,” she said. “If I give it to patients with melasma, I combine it with retinoids, because they act in a different way, or with topical or oral tranexamic acid to address the vascular component.” Avoiding sun exposure and broad spectrum sunscreen with VL cover, she added, is a vital part of the treatment armamentarium.
Enhancing the Efficacy of Laser Treatment
The 2024 review of Thiamidol studies discussed earlier recommended future research should explore the potential benefits of combining Thiamidol with laser treatment to reduce the risk of laser-induced PIH.11 Vachiramon, who has examined this question in relation to solar lentigines, explained that PIH is a common complication of laser therapy, particularly in people with darker skin types. Laser-induced PIH affects between 10–47% of people.8
“Although there are several therapeutic options available for PIH, prevention is still the best method,” he wrote in his 2023 paper, ‘Efficacy of isobutylamido thiazolyl resorcinol for prevention of laser-induced post-inflammatory hyperpigmentation: A randomized, controlled trial’. “For laser-induced PIH, few options exist regarding the prevention of this condition. Recently, isobutylamido thiazolyl resorcinol (ITR/ Thiamidol) has been reported as an effective tool for the prevention of UVB-induced hyperpigmentation. Therefore, we hypothesised that ITR might be able to prevent PIH due to other modalities as well.”8
The study included 24 people, and researchers selected three solar lentigines of a similar size and colour on each. The lesions were then randomised into three groups: twice-daily Thiamidol application, once-daily Thiamidol application, and no application, all for 2 weeks. Next, the patients underwent 532-nm QS Nd:YAG laser therapy. The primary outcome measure was incidence of laser-induced PIH, defined by worsening of the pigmented lesion compared to 2 weeks post-laser, at 4 and 8 weeks after laser treatment. At Week 4, the incidence of PIH was significantly lower in the twice-daily Thiamidol group, compared to the no-application group (20.83% versus 50.0%; p=0.028). Incidence in the once-daily treatment group at Week 4 was 29.17%. At Week 8, there was a higher incidence of PIH in the treated groups (twice daily: 16.67%; once daily: 8.33%) than the non-treated group (4.16%) though the difference between groups was not statistically significant. The authors hypothesised that the increase could be related to the reversible tyrosinase inhibitory effect of Thiamidol. No serious adverse events or stinging, burning, or contact dermatitis were reported in the Thiamidol-treated groups. The paper also recommended Thiamidol be continued, after laser therapy, to further inhibit tyrosinase. “Longer duration of application, including continuous application after the laser treatment and co-administration with other anti-inflammatory agents may result in more effective prevention of laser-indued PIH”, they concluded.8
In another study, he examined the use of Thiamidol in combination with laser therapy in people with symmetrical facial hyperpigmentation. Twenty-four patients were treated with five weekly sessions of low-fluence Q-switched Nd:YAG 1064-nm laser (LFQS). Afterwards, one side of the face was treated with Thiamidol and the other side received a placebo cream for 12 weeks. Patients were followed for 8 weeks after the last laser treatment, and relative lightness index (RL*I), Facial Hyperpigmentation Severity Score on the malar area (FHSSm), patient satisfaction, recurrence, and adverse events were all recorded. At Week 4, there was a higher mean RL*I improvement on the Thiamidol-treated side than the placebo-treated side (62.5% versus 47.3% improvement; p<0.05). The mean FHSSm reduced at a significantly higher percentage on the ITR-treated side than the placebo-treated side (54.4% versus 40.2% reduction; p<0.05). Partial recurrence was observed on both sides, and no serious side effects were noted. The paper concluded that combined Thiamidol and LFQS therapy was superior to LFQS monotherapy in the treatment of facial hyperpigmentation, and that Thiamidol “may serve as adjuvant” in this cohort.13
Reflecting on the results of his solar lentigines, Vachiramon said: “When we applied the cream for 2 weeks before the laser therapy, the number of patients with darkened skin 4 weeks after treatment was less. I think this shows that this is a good idea. The ingredient’s mechanism of action is to inhibit tyrosinase activity at the site, so even if the skin is burned during laser therapy, it cannot produce melanin.”
He went on to say that he is increasingly using Thiamidol in clinic, as it has been shown to be effective and well tolerated. “I think it should be one of the preventative tools that we offer our patients. It helps to reduce the volume of prescription medicine they use because patients can go and buy it themselves,” he said.
Prevention
There is also emerging evidence to suggest that Thiamidol could prevent hyperpigmentation. Vachiramon’s team has conducted a randomised, single-blinded, pilot study to evaluate the efficacy and safety of ITR in the prevention of UV-induced hyperpigmentation. Each of the 20 healthy participants applied a product containing ITR to one arm for 3 weeks, before researchers induced UVB irradiation on both arms. Compared to the control, ITR-treated arms showed a statistically significant lower mean lightness index. In addition, the ITR-treated arms improved rapidly, with normal skin colour being observed at 3 weeks after the UVB induction. Clinical evaluation by a blinded, non-treating physician and by subjects was more favourable on the ITR-treated side than the control side (p<0.05). No significant side effects were noted. “ITR is an effective agent in the prevention of pigmentary change from UVB irradiation and may serve as a promising agent for preventing other hyperpigmentary conditions,” concluded the paper.14
FUTURE DIRECTIONS
Looking to the future, Passeron said he expected a deeper understanding of the pathophysiology of hyperpigmentation disorders to lead to topical treatments that target the underlying mechanisms of disease, particularly in melasma. “I do hope that one day we will be able to cure, or at least reduce relapses, in melasma,” he said. Dlova’s hopes for the future of hyperpigmentation management focused on increasing access to what can sometimes be expensive treatments, particularly in less resourced parts of the world. She also hopes for a wider recognition of the impact of these conditions, in order for their treatment to be covered by medical insurance.
Asked the same question, Vachiramon said he hoped the community would continue to build on its recent successes. “We are moving to options that have good efficacy with a high safety profile. It is great that we have the ingredients we have nowadays, but I hope that we will have many more ingredients that target different steps of the melanin synthesis in future. That would allow us to combine each of them, and further enhance the result of treatment.”
Summing up, Vachiramon added: “Most hyperpigmentation issues are cosmetic. They may not be harmful, but they can still have a negative impact on patients’ QoL, and they can lose their self-confidence. Yet, with the tools that we have nowadays, we can combat it, we can treat it, and we can improve our patients’ QoL.”






