Women’s health remains chronically underfunded, yet closing the gap could unlock a trillion-dollar economic opportunity. It’s time for the healthcare industry to act
Words by Jade Williams
Women spend 25% more time in poor health than men. That’s a quarter more time battling pain, fatigue and often misdiagnosed health issues – while at the same time juggling careers, caregiving and everything else life throws at them. This isn’t just a moral issue, however – it’s an economic one.
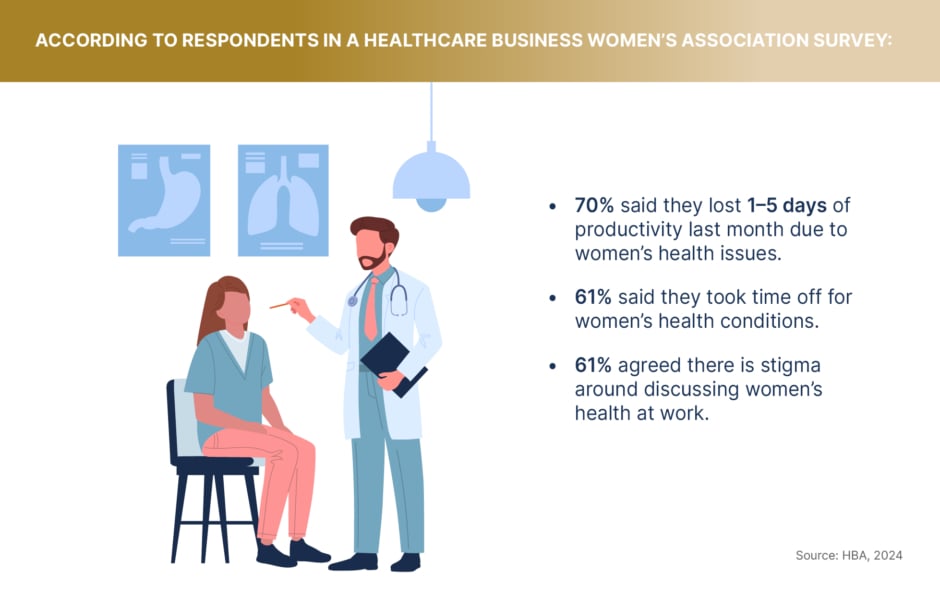
When the health of half the population is systematically neglected by the systems designed to protect it, the consequences ripple through society. Productivity declines, healthcare costs rise and entire economies suffer. The Healthcare Businesswomen’s Association (HBA) recently found that 70% of women working in the healthcare sector said they lost 1–5 days of productivity in the past month due to women’s health issues. When disparities like this exist, the entire healthcare sector strains under the pressure.
Fixing this issue isn’t just about fairness or morality – it’s a trillion-dollar opportunity waiting to be seized. The question is not whether investing in women’s health is important, but rather, could closing the gender health gap unlock a new driver of global economic growth?
Closing the gender gap in health is going to take a lot of effort and change
The cost of neglect
For decades, medicine has been designed for men, with women’s health concerns either dismissed, misdiagnosed, or simply under-researched. The result? A healthcare system that routinely fails half the world’s population.
“Women experience diseases differently and may show different symptoms for the same diseases,” notes Robyn Widenmaier, Global Medical Strategy Lead, GSK, in a roundtable interview with EMJ GOLD. “On top of this, the prevalence, course and severity of many common diseases, and how women metabolise drugs, can be different.” Cardiovascular disease, for example, the leading cause of death in women, has been studied primarily in men – leading to critical gaps in understanding how symptoms manifest differently in women, with dire consequences.
“The challenge is that [much] of the research that has been done has been done on men,” agrees Mary Stutts, CEO, HBA, speaking in a recent EMJ GOLD Podcast interview. “Only about 10% of the anatomies in medical school textbooks are based on women, and less than 3% is based on the anatomies of people of colour.” This fundamental bias in medical education means that HCPs are often set up to fail, lacking the knowledge and resources needed to recognise and address sex- and race-based disparities.
This lack of education has very real consequences. In another HBA survey, HCPs reported to that they felt underprepared to treat female patients, particularly when it comes to conditions related to hormonal changes such as menopause. Until medical education evolves to reflect the reality of the patients’ doctors are treating, women’s health will continue to be sidelined.
The impact of this neglect is particularly evident in conditions like endometriosis, which affects one in ten women of reproductive age yet remains severely under-researched. According to the NHS, it currently takes an average of eight years for women with endometriosis to receive a diagnosis, leaving them in prolonged pain without effective treatment options – delays that are often even longer for women of colour. But the problem goes beyond delays in diagnosis itself.
The financial disparity in research funding is staggering. In the US, McKinsey found that only 11% of health research and innovation funding from the National Institutes of Health is dedicated to female-specific health conditions. This is also behind gaps medical knowledge, limited treatment options and the long delays women experience in diagnosis. Without meaningful investment in research and education, the cycle of neglect will continue.
Why ignoring women’s health costs everyone
Beyond the human cost, the neglect of women’s health is severely impacting global economies. Poorly managed women’s health conditions lead to reduced workforce participation, lower productivity and an increasing burden on healthcare systems.
Stutts reinforces this point by stating that women make up most of the healthcare workforce and are reported to be up to 90% of the world’s caregivers – both paid and unpaid. “If these women are not healthy themselves, this puts all of our society at risk of not being healthy.” When people responsible for delivering care are unable to access the medical support they need, the entire healthcare system suffers.
A healthier workforce means fewer sick days, higher productivity and lower long-term healthcare costs – yet the investment in women’s health remains insufficient. Addressing this gap isn’t just about improving individual health outcomes; it’s about securing economic stability. McKinsey estimates that closing the women’s health gap could add $1tn to the global economy annually by 2040. The question isn’t whether the world can afford to prioritise women’s health – it’s whether it can afford not to.
The challenge is that all of the research that has been done has been done on men
Where change begins
So how do we get there? Despite decades of neglect, there is a growing recognition that women’s health is not just a social issue, but a business imperative. One of the most important shifts is one of perception – for too long, women’s health has been considered a niche market rather than a fundamental pillar of healthcare – but that seems to be slowly changing.
Institutions such as the UK’s NHS have begun to prioritise prevention for women’s health issues, including a recent cervical cancer campaign to increase uptake of screening after it was found that a third of women under 50 were not attending appointments. While perceptions around women’s health are shifting, significant gaps persist across all age groups.
Menopause, a universal transition for women, remains particularly underfunded and overlooked despite its profound impact on health, work and quality of life. NHS data reveals that menopause symptoms lead to unemployment for approximately 60,000 women in the UK annually, costing the economy £1.5 billion.
The financial toll of neglecting women’s health is undeniable. Closing these gaps isn’t just about better healthcare – it’s about economic resilience, ensuring that women can effectively participate and thrive in the workforce, ultimately contributing to the global economy.
The window of opportunity
The momentum for change has never been greater. For World Health Day 2025, the theme is improving maternal and newborn health, signalling a global shift toward prioritising women’s healthcare. As research continues to show the scale of the economic losses associated with poor health outcomes for 50% of the population, the world is waking up to the need for action.
“Closing the gender gap in health is going to take a lot of effort and change in a lot of parts of the healthcare system,” notes Widenmaier. “But as R&D organisations in the industry, we have a role to play.” Investing in women’s health is no longer a question of ‘if’ – it’s a question of ‘when’ and ‘who’. The companies who take action today will be the ones shaping the trillion-dollar future of healthcare.









