TYPE 2 diabetes has been shown to alter cognition and mood, meaning it has often been considered to be an early risk factor for Alzheimer’s disease and vascular dementia. Epidemiologic studies have shown that Type 2 diabetes increases the risk of cognitive deficits and mood disorders by 1.5- and 2-fold, respectively. Whole-brain diffusion tensor imaging permits the imaging of the brain’s microstructural organisation in grey and white matter, and the measurement of mean diffusivity (MD), a measure of the movement of water particles, reveals the nature of brain tissue injury.
The present study included 68 patients with Type 2 diabetes receiving medication from the Gonda Diabetes Centre, University of California, Los Angeles, USA, and 101 healthy, non-diabetic controls. All participants were aged between 40–65. The Diabetes Complications Severity Index of each patient was determined using clinical records, and anxiety and depression symptoms were evaluated using the Beck Anxiety Inventory and Beck Depression Inventory, with values of >9 indicating a positive result.
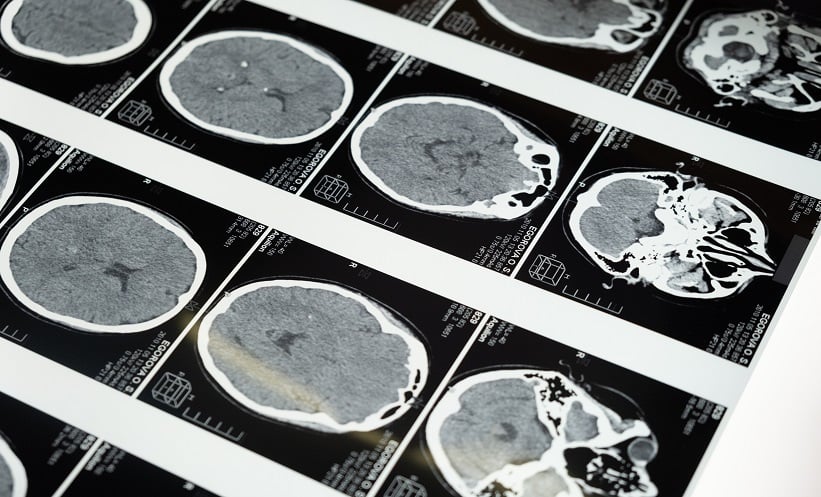
Cognitive impairment was assessed using the Montreal Cognitive Assessment, with scores of >26 considered a positive result. Diffusion tensor imaging data were collected using a single-shot echo planar imaging technique, generalised auto-calibrating partially parallel acquisition (GRAPPA), with an acceleration factor of 2. Regions of interest values were obtained for regions associated with mood and cognition values in all participants. Whole-brain MD maps were also correlated with mood and cognition scores.
Analysis revealed widespread microstructural disruption in brain regions controlling cognitive and mood functions in people with Type 2 diabetes compared to controls. Most of these changes were identified during the chronic stages, with only a few sites in the acute stages. Furthermore, patients with Type 2 diabetes exhibited impairments in visuospatial, attention cognitive, and language sub-domains, as well as greater depression and anxiety scores. Extensive microstructural tissue changes in these areas play a unique role in cognitive and mood deficits in patients with Type 2 diabetes, as these networks are spread over a large area in the human brain.
In conclusion, these findings provide important insight into the microstructural neuropathological changes that can contribute to mood and cognitive dysfunction in patients with Type 2 diabetes. This highlights how MD can facilitate the early detection of microstructural brain tissue changes in the cognitive and mood regulatory regions of patients with Type 2 diabetes, leading to altered mood and cognition deficits.