INTRODUCTION
Meal timing is a crucial factor influencing metabolic health, which can be explained by the tight interaction between circadian clocks and metabolic homeostasis.1 Recent evidence suggests that meal timing pattern might contribute to obesity and diabetes risk,2 but this topic is still insufficiently studied. This work aimed to investigate the link between individual meal timing pattern and glucose metabolism as well as explore the contribution of genetic and environmental factors to the meal timing architecture.
METHODS
The research was conducted in a German NUtriGenomic Analysis in Twins (NUGAT) cohort (NCT01631123; n=89) comprising 32 monozygotic and 12 dizygotic twin pairs with a BMI of 22.8±2.8 kg/m² and median age of 25.0 years (interquartile range: 22.0).3 Glucose metabolism was assessed using the oral glucose tolerance test. Parameters of meal timing pattern (meal timing itself, daily calorie distribution, and meal number) were extracted from 5-day food records. Circadian timing of the caloric midpoint of the first and last eating events was determined as the time differences relative to the individual chronotype (MSFsc) assessed by the Munich chronotype questionnaire. Heritability of meal timing components was estimated by the ACE model, and bivariate correlation analyses were performed to assess their relation to metabolic traits.
RESULTS
Correlation analysis revealed a number of associations between meal timing components and glucose metabolism parameters. Most associations were found for the calorie midpoint, defined as the time point at which 50% of daily calories were consumed. Indices of insulin sensitivity, Stumvoll Insulin Sensitivity Index (β=0.334; p=2.9×10-4) and Homeostatic Model Assessment for Insulin Resistance (HOMA-IR; β=-0.276; p=0.007), as well as fasting insulin levels (β=-0.278; p=0.008), were significantly associated with the circadian caloric midpoint even after the model adjustment for gender, age, energy intake, and sleep duration (Table 1).
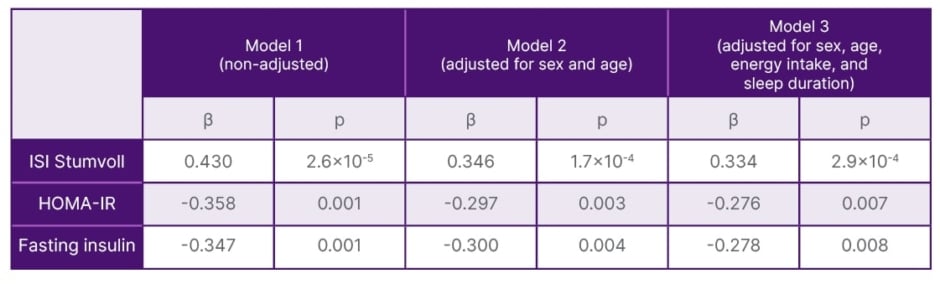
Table 1: Associations of circadian caloric midpoint with insulin sensitivity and fasting insulin.
Linear regression analyses were performed to estimate the strength of association between variables. β are the standardised coefficients; p are the p-values.
HOMA-IR: Homeostatic Model Assessment for Insulin Resistance; ISI: Insulin Sensitivity Index.
The association with the Matsuda Insulin Sensitivity Index was lost after the adjustment for energy intake and sleep duration. BMI and waist circumference also demonstrated robust associations with the circadian caloric midpoint in adjusted models (β=-0.263; p=0.005; and β=-0.194; p=0.014, respectively). All meal timing components showed high or moderate heritability. Meal timing components demonstrated the strong relation to the individual sleep-wake timing and chronotype, both of which also showed a marked genetic impact.
CONCLUSION
Circadian meal timing is associated with insulin sensitivity and shows significant genetic influences, sharing a common genetic architecture with sleep behaviour. These findings help to differentiate (none-)modifiable factors driving individual meal timing, which is important for the development of effective nutritional strategies to combat obesity and diabetes.







