Meeting Summary
The different wavelengths of the electromagnetic spectrum, including ultraviolet (UV) A and B, visible light (VL), and infrared radiation, can penetrate the skin to different depths according to wavelength. The degree of damage and/or pigmentation they cause can depend on factors such as the skin phototype and sun exposure. Sunscreen is essential for all skin types, but the need for protection from these wavelengths differs according to phototype and with the manifestation of a variety of dermatological conditions. At the 30th European Academy of Dermatology and Venereology (EADV) virtual congress, held from 29th September to 2nd October 2021, the industry presentation ‘Revolution in Photoprotection’ included sessions on skin phototypes, photoprotection, photoaging, photodermatoses, pigmentary disorders, skin inflammatory disorders, and skin cancer, which were presented by a number of leading dermatology experts. Here, the main points of these sessions are discussed, and data was presented regarding the UVA1 filtering agent methoxypropylamino cyclohexenylidene ethoxyethylcyanoacetate (MCE), known as Mexoryl 400.
Introduction
The solar spectrum is composed of various wavelengths of electromagnetic radiation that can penetrate the skin to different levels: the longer the wavelength, the deeper the skin penetration. For instance, while UVB and UVA2 penetrate superficial skin layers, down to the basal layer of the epidermis, long-wave UVA1 can penetrate deeper, into the dermis, and VL and infrared radiation deeper still, reaching the hypodermis.1,2
In the ‘Revolution in Photoprotection’ symposium presented at the EADV Congress, Sérgio Schalka, Henry Lim, Jean Krutmann, Thierry Passeron, Brigitte Dréno, and Jorge Ocampo Candiani, as well as Martin Josso, discussed skin phototypes and the photoprotection required to protect against skin cancer, alongside specific considerations for people with skin inflammatory disorders or pigmentary disorders.
Skin Phototypes and the Effects of Ultraviolet A, Ultraviolet B, and Visible Light
The profile and risk of actinic damage caused by UVA, UVB, and VL depends mainly on skin phototype, with influences of other factors, including geographic location, professional activity, and lifestyle. Dark skin is more prone to skin pigmentation, melasma, and post-inflammatory hyperpigmentation, while light skin is more prone to sunburn, DNA damage, skin cancer, photoaging, and solar lentigo.3
Fitzpatrick skin phototypes range from I to VI and are based around reaction to 45–60 minutes of unprotected sun exposure, according to erythema sensitivity (‘sunburn’) in the first 24 hours and tanning in the subsequent 7 days (Table 1).3,4
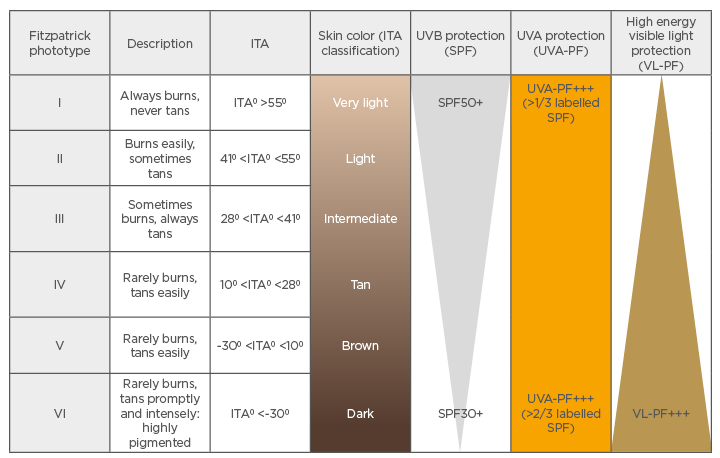
Table 1: Fitzpatrick skin phototypes, classification, and the need for ultraviolet A, ultraviolet B, and visible light protection from sunscreen.
Adapted from Passeron et al.5
ITA: individual typology angle; PF: protection factor; SPF: sun protection factor; UVA: Ultraviolet A; UVB: Ultraviolet B; VL: visible light.
While UVA1 is less energetic than UVB, importantly, pointed out Passeron, it represents a huge proportion of the UV light people receive, is constant throughout the day, regardless of the season, and can penetrate through windows, so people can be chronically exposed to it. Gene expression studies show that in fibroblasts and keratinocytes, a number of genes are modulated by UVA1 exposure, including the upregulation of genes linked to inflammation and the downregulation of genes linked to antiviral and antimicrobial defense.6In vivo studies also show a link between UVA1 and, to a lesser extent, UVB exposure and solar immune suppression,7 meaning, stressed Josso, that UVA1 exposure can be very impactful on the skin.
UVB induces a direct effect on melanocytes and leads to the activation of the p53 protein in keratinocytes.8 This protein binds to the pro-opiomelanocortin promoter, responsible for production of α-melanocyte-stimulating hormone, which in turn induces pigmentation.8
VL in the high energy blue/violet spectrum (around 415 nm)9 has a role in hyperpigmentation in darker skin (phototypes IV–VI). This occurs through the opsin-3 receptor and pathway, which leads to the induction of the melanogenesis enzymes tyrosinase and dopachrome tautomerase and a complex of tyrosinase/tyrosinase-related proteins that are involved in long-lasting hyperpigmentation.10 This pigmentation can be more intense and prolonged compared to that induced by UVA1.11,12
Photoprotection
According to Schalka, all skin types need a photoprotection strategy, including regular use of the right sunscreen. In such formulations, the UVB protection level is defined by the sun protection factor (SPF) number and UVA protection by the UVA-protection factor (UVA-PF) and critical wavelength. There is currently no standard method to commercially portray sunscreen efficacy against VL.5 Although there may be a ‘UVA’ logo on sunscreens, most people, reported Passeron, choose suncreen based on the SPF index only.
It is recommended that sunscreen use should be regular even on cloudy days, applied every 2–3 hours or after water immersion, and used at a volume of around 2 mg/cm2.5 The average time to experiencing enough sun to produce erythema sensitivity (the ‘minimum erythemal dose’) is 15 minutes for people with phototypes I and II and 45 minutes for those with phototype IV. Phototypes I and II need three times the amount of sun exposure to produce pigmentation rather than erythema, with phototype IV needing the same amount of time for both.13 This, according to Schalka, means phototypes I and II need three times more UVB-SPF protection than UVA-PF, and phototype IV skin needs approximately the same amount of UVB and UVA protection (Table 1).
VL is important in skin pigmentation development in phototypes IV−VI.5,14 As such, effective UVA1 and VL protection is particularly important for darker skin phototypes, stressed Krutmann. For this, there are now chemical filters available to screen out UVA1 and inorganic sunscreens containing iron oxides that screen out VL.6 For protection from infrared A radiation (IRA), topical application of antioxidants has been shown to be useful.14
There are a number of UV filters available in sunscreens, but while most screen out UVB, with some also blocking UVA2, currently only one screens the 380−400 nm spectrum of UVA1 (Figure 1): the filter MCE, often known as Mexoryl 400. MCE has received regulatory approval in Europe and several Latin American countries, with approval pending in Brazil and several southeast Asian countries. No risk of endocrine modulation or bioaccumulation has been shown with MCE and there is no environmental labelling.
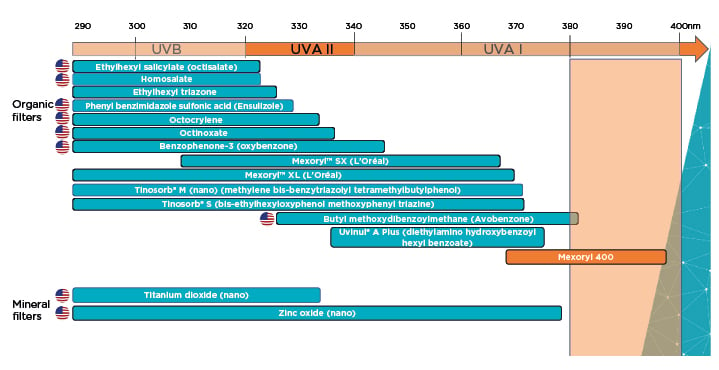
Figure 1: The main ultraviolet filters available worldwide.
Adapted from Josso
UVA: Ultraviolet A; UVB: Ultraviolet B.
Josso discussed a series of studies that were carried out to examine the effects of MCE. One in vitro study showed that the number of fibroblasts remaining following UVA1 exposure was significantly higher with an MCE-containing formulation compared with a classic sunscreen formulation that had no UVA1 protection, with almost no decrease even at high levels of UVA1. At the gene level, the number and intensity of gene modulation (increase or decrease) was significantly lower with the MCE formulation compared with the classic sunscreen formulation, including genes involved in oxidative stress, antiviral defence, inflammation, and proliferation. In some genes, modulation was similar to the control cells not exposed to UVA1.
In a study involving 19 participants with skin phototypes III and IV, 1.5% MCE-containing sunscreen application followed by UVA1 exposure led to lower levels of pigmentation at 2 and 24 hours compared with a vehicle cream control. A further study (n=20; phototypes III and IV) investigated 7 days repeated UVA1 and UVAB exposure. An SPF30 formulation with 2% MCE led to significantly lower pigmentation than the SPF30 formulation alone. Finally, a study over 14 days (n=22; phototypes III and IV) showed similar findings when an SPF50+ and 1% MCE sunscreen was compared to a commercial SPF50+ and UVA protection formulation, with the 1% MCE formulation being significantly better in terms of pigmentation from Day 3 onwards.
These studies, Josso discussed, point to the utility of including MCE in sunscreen formulations, as is currently becoming available commercially.
Photoprotection According to Skin Condition
UV rays are responsible for the majority of known photobiological effects of the sun on the skin, including: sunburn and tanning; photoimmunosuppression and viral reactivation; pigmentary disorders such as melasma; actinic lentigines and keratoses; wrinkles; and photocancers.5
Photodermatoses, Hyperpigmentation, and Photoaging
Photodermatoses include polymorphous light eruption, chronic actinic dermatitis, solar urticaria, drug-induced photosensitivity, and erythropoietic protoporphyria. Lim highlighted how for all of these conditions, it is advised to seek shade, wear photoprotective clothing, and apply a broad-spectrum sunscreen with SPF30+. In particular for those with solar urticaria and cutaneous porphyrias, a tinted or coloured sunscreen is recommended to help to protect against the sun’s effect.16
As pigmentation and hyperpigmentation may be induced by a synergistic combination of UVA and VL,17 along with UVB, protection against all three is mandatory to prevent this. It is, therefore, recommended to use a balanced SPF50+ and UVA-PF 21 sunscreen that is able to limit both UVA and UVB wavelengths.13 Protection against VL can occur through shielding with products containing titanium dioxide or red, black, or yellow iron oxides.18 While people with phototypes I–III usually do not need VL protection, Passeron discussed how this is needed by those who have a variety of dermatological conditions, including melasma, acne marks, actinic lentigo, post-inflammatory hyperpigmentation, or blue light sensitivity.
The pathogenesis of photoaging involves the range of solar spectra. Regular use of sunscreens, discussed Krutmann, protects against photoaging, as shown in a number of studies,19 such as one investigation in elderly Japanese people that showed a clear association between regular sunscreen use and a decrease in age spots.20
Skin Inflammatory Disorders
Candiani discussed several skin inflammatory disorders and the photoprotection required for these. Sun exposure can be beneficial to people with atopic dermatitis;21 however, photoaggravation, where the skin deteriorates following such exposure, can occur in some patients and, in individual case studies, has been linked to allergic reactions to an ingredient in sunscreen.22 As such, atopic dermatitis patients should avoid using sunscreen on lesions that are weeping, moist, or scarred through scratching.23
Psoriasis is another skin condition that can be improved by sun exposure; however, in some patients, especially those with light skin, photoaggravation can occur.24 All patients should avoid sunburn as it can cause Koebnerisation of psoriasis,24 and those with photoaggravation should use a broad-spectrum, SPF50+ sunscreen with high UVA protection.
For people with acne, it is known that blue and red waves of light can help to inhibit Cutibacterium acnes-associated inflammation.14 However, UVA and UVB can induce dysbiosis and UVA exposure can lead to epidermal thickening.25 Accordingly, a UVA/UVB sunscreen that is non-comedogenic and does not interfere with topical acne medication is recommended for those with acne.26 As rosacea can be triggered by UV light and heat via a number of different cell pathways, daily use of a broad-spectrum, SPF30+ sunscreen can help to protect against these triggers.
Skin Cancer
Skin cancer is one of the most common malignancies in the world and is an important public health concern as the incidence of both melanoma and non-melanoma skin cancer has increased over the past decades.27 Globally, around 325,000 melanomas and 1,198,000 new non-melanoma skin cancers occur each year, leading to approximately 121,000 deaths.28 It is not only direct sunlight that can be harmful; sunbed use is also associated with an increased risk of early onset melanoma, with the risk increasing with greater use and earlier age at first use.27
Clearly, discussed Dréno, in phototypes I and II, the risk of skin cancer is increased as fair skin has a higher mutational burden with UV signature.29 A recent systematic review suggested that UV exposure leading to skin cancer may not be as important in people with a darker skin colour.30
The challenge, highlighted Dréno, is to promote the use of sunscreen as a key component of public health campaigns for skin cancer prevention, as several trials have shown the utility of such. For instance, one randomised trial in Australia over 4.5 years with an 8-year follow-up period showed a reduction in the rate of melanoma in participants assigned to daily sunscreen use (hazard ratio [HR]: 0.50; 95% confidence interval [CI]: 0.24, 1.02; p=0.051). The reduction in invasive melanomas was substantial (HR: 0.27; 95% CI: 0.08, 0.97) compared with that for preinvasive melanomas (HR: 0.73; 95% CI: 0.29, 1.81).31
Another study found that after an 8-year follow-up, regular sunscreen use possibly reduced the number of cases of squamous cell cancers (SCC) (risk ratio: 0.65; 95% CI: 0.45, 0.94), but not basal cell cancers (BCC), though this may be due to the latter taking many years to develop.32 A randomised, controlled trial (n=1,621; follow-up 4.5 years) also provided some evidence that daily use of SPF15+ sunscreen plus betacarotene resulted in a small reduction of SCC and no difference in BCC incidence compared with the discretionary sunscreen group.33 Finally, a 24-month prospective, case-control study provided evidence that regular use of sunscreen (SPF>50, high UVA-protection factor) may help to prevent the development of further actinic keratoses and invasive SCC in immune-compromised organ transplant recipients.34 Overall, a recent systematic review supported the topical application of sunscreen to help to prevent skin cancer and precancerous skin lesions.35
Dréno concluded that, for melanoma, especially in fair-skinned individuals, sunscreens needed to have SPF50+ and a SPF and UVA-PF ratio close to 1. For the prevention of BCC, acitinic keratosis, and SCC, sunscreens with SPF50+ and a SPF/UVA-PF ratio <3 are recommended.5 Photoprotection is especially important in childhood for preventing sunburn as this is a high-risk factor for developing melanoma later in life.
Conclusion
Protection needs against UV, VL, and IRA electromagnetic radiation may vary by skin phototype, but the daily use of a sunscreen that covers the solar spectrum, including UVB, UVA, VL, and IRA, is recommended for most people, especially those with certain skin conditions. Advances in sunscreens containing MCE mean that longwave UVA1 can now be screened against using these commercially available formulations.







