Meeting Summary
This Blue-Ribbon poster presentation, ranking among the top five abstracts at this year’s National Comprehensive Cancer Network (NCCN) Annual Conference, highlighted research in cutaneous squamous cell carcinoma (cSCC) risk evaluation using gene expression profiling. cSCC affects approximately 1.8 million Americans annually; however, identifying high-risk individuals who require more frequent monitoring and other treatment interventions has been challenging. Shlomo A. Koyfman, Director of the Precision Oncology Program and Radiation Oncologist at Cleveland Clinic, Ohio, USA, presented data from 1,412 high-risk patients with cSCC, making this study the most extensive analysis of high-risk patients stratified by gene expression profiling. Researchers integrated a 40-gene expression profile (40-GEP) test with established clinical staging methods (Brigham and Women’s Hospital [BWH] staging), achieving enhanced precision in predicting the risk of metastasis compared to clinical staging alone. This integration of molecular and clinicopathological information addresses the shortcomings of current risk assessment approaches that rely solely on clinicopathological characteristics. By offering a more accurate risk assessment model, this work could assist healthcare providers in customizing treatment plans and surveillance approaches based on the risk of metastasis, ultimately enhancing outcomes in high-risk cSCC management.
Introduction
cSCC is a common type of skin cancer, with approximately 1.8 million cases diagnosed annually in the USA.1 Although most patients are successfully treated with complete surgical excision, which is the standard-of-care treatment for cSCC, a subset of patients remain at high risk of metastasis despite receiving treatment.2,3 Studies have shown that metastasis rates after surgery range from 1.9–2.6% in the general population of patients with cSCC, increasing to 14–20% in high-risk patients.4-7
The BWH staging system is the standard tool used to risk-stratify patients with cSCC based on tumor diameter, depth of invasion, perineural invasion, and poor differentiation.8 Moreover, the NCCN guidelines are commonly used to stratify patients with cSCC into low-risk, high-risk, and very high-risk groups based on clinicopathological features that are associated with local recurrence and metastasis, including tumor location, diameter, and clinical borders.9 However, these risk assessment criteria often fail to capture the underlying biology driving metastasis in cSCC.1,10,11 Thus, there is a need for new tools to accurately identify patients who are most likely to develop metastases and would, therefore, benefit from adjuvant therapies and intensified surveillance.1,11
Investigating the Role of Molecular Profiling in Enhancing Risk Assessment
The 40-GEP test was developed as a prognostic tool to improve risk stratification in patients with cSCC.12 The test analyzes the expression of 40 genes associated with tumor progression and metastasis.13,14 Validation studies have shown that the test provides additional prognostic information beyond traditional clinicopathological factors.12
To investigate the role of 40-GEP testing in enhancing risk assessment in cSCC, Koyfman and colleagues integrated molecular information from the 40-GEP test with BWH staging to risk-stratify 1,412 patients with cSCC who had clinical or histologic risk factors.15 The researchers combined data from a previously published retrospective study (n=897)16 with a retrospective cohort from two academic centers (n=515), making this the largest high-risk cSCC cohort ever stratified based on gene expression profiling (Figure 1).
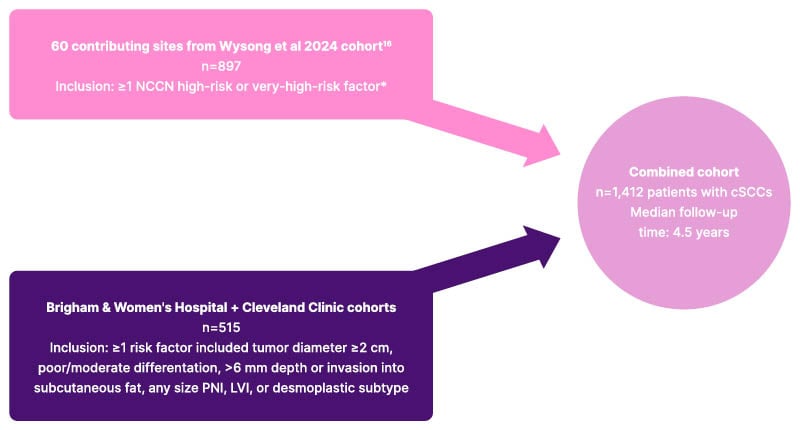
Figure 1: Consort diagram.15
*Also enrolled limited patients (n=14) with non-NCCN high-risk features: tumor diameter = 2 cm or infiltrative histologic type.
cSCC: cutaneous squamous cell carcinoma; LVI: lymphovascular invasion; NCCN: National Comprehensive Cancer Network; PNI: perineural invasion.
Patients who received adjuvant radiation therapy were excluded to focus on the prognostic value of the 40-GEP test in the context of surgical management. NCCN guidelines were used for initial risk stratification,9 categorizing patients into low-risk (4.5%), high-risk (59.6%), and very high-risk (35.8%) groups (Table 1).
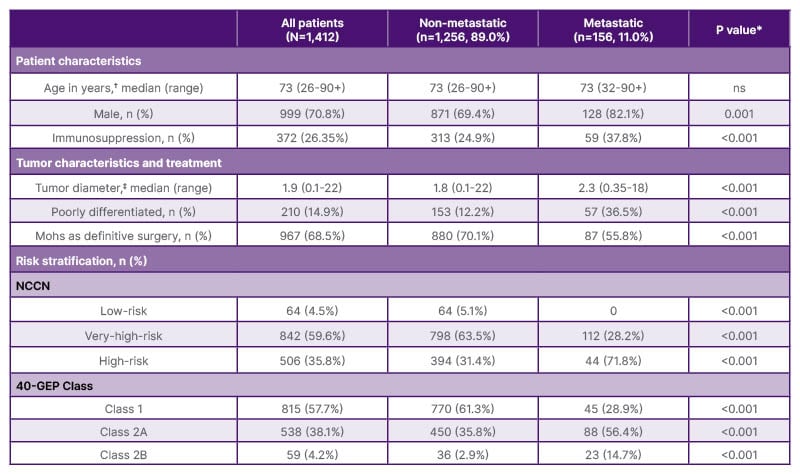
Table 1: Demographic characteristics of the study participants (N=1,412).15
Percentages shown were calculated as a fraction of the total n of each respective column header.
*P-values reported for Person Chi-squared or Wilcoxon F test, as appropriate.
?Ages over 90 years reported as 90+ for privacy.
‡n=85 cases without tumor diameter available.
40-GEP: 40-gene expression profile; NCCN: National Comprehensive Cancer Network; ns: not significant.
40-Gene Expression Profile Classification Improves Risk Stratification
The primary outcome of the study was 3-year metastasis-free survival (MFS), which was estimated using Kaplan-Meier survival analysis at a median follow-up of 4.5 years. According to the study findings, the 40-GEP test demonstrated significant prognostic value in patients with high-risk and very high-risk cSCC. Among patients who were classified as high-risk according to the NCCN guidelines, 3-year MFS rates were 97.4% (95% CI: 96.0–98.7%) in 40-GEP Class 1, 91.2% (95% CI: 87.9–94.6%) in 40-GEP Class 2A, and 71.4% (95% CI: 53.1–96.2%) in 40-GEP Class 2B (p<0.001; Figure 2).15
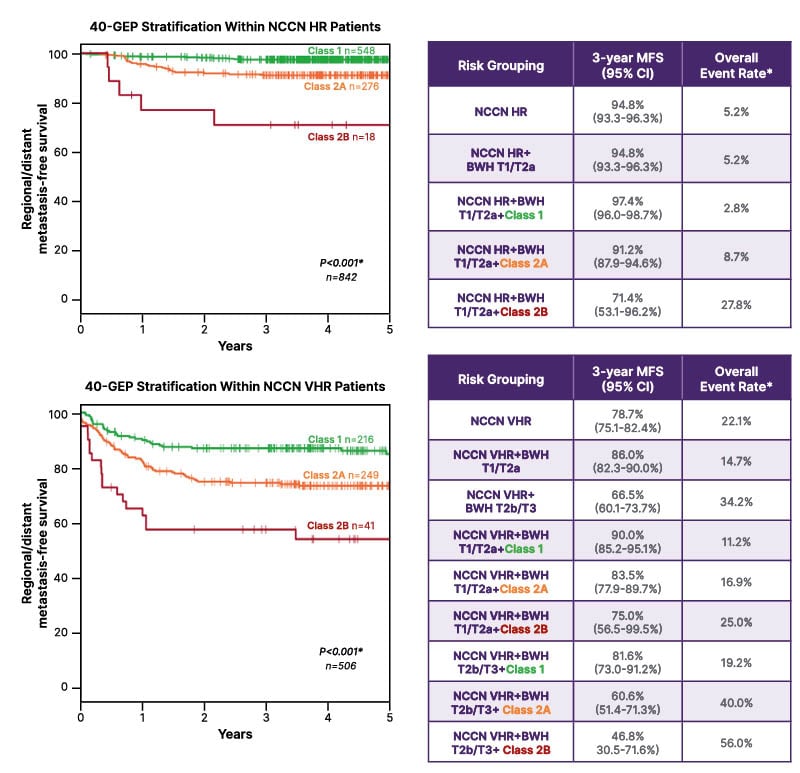
Figure 2: The 40-gene expression profile provides significant metastatic risk stratification in National Comprehensive Cancer Network high-risk and very-high-risk patients.15
*Overall event rate and log-rank test for statistical significance include total events occurring at any time point during study follow-up, including patients who were followed longer or had metastatic events later than the 5 years displayed.
40-GEP: 40-gene expression profile; BWH: Brigham and Women’s Hospital; HR: high-risk; MFS: metastasis-free survival; NCCN: National Comprehensive Cancer Network; VHR: very-high-risk.
Similarly, the 3-year MFS rates among patients who were classified as very high-risk according to the NCCN guidelines differed significantly when patients were classified based on the 40-GEP class. Among patients who were classified as very high-risk, the 3-year MFS rates were 90.0% (95% CI: 85.2–95.1%), 83.5% (95% CI: 77.9–89.7%), and 75.0% (95% CI: 56.5–99.5%) for 40-GEP Classes 1, 2A, and 2B, respectively (p<0.001; Figure 2).15 These findings highlight the ability of the 40-GEP test to further stratify patients within existing NCCN risk categories and identify patients with substantially different metastatic risks, even among those already considered very high-risk by the NCCN criteria.
Combining 40-Gene Expression Profile Classification with Brigham and Women’s Hospital Staging Enhances Risk Prediction
Cox regression models were used to compare the predictive performance of BWH staging alone versus BWH staging plus 40-GEP within NCCN risk groups. Combining 40-GEP classification with BWH staging (using a binary T1/T2a versus T2b/T3 classification) provided statistically significant improvements in model performance compared to BWH staging alone, both in NCCN very high-risk (χ2=17.32; p<0.001) and NCCN high-risk (χ2=26.62; p<0.001) patient populations.15 These findings suggest that integrating prognostic information from molecular testing and traditional clinicopathological factors enhances patient stratification based on the risk of metastasis compared to using clinicopathological factors alone.
Implications
Koyfman concluded that the enhanced risk stratification provided by combining molecular and clinical criteria allows for the identification of patients who might benefit from more intensive surveillance or adjuvant therapy, while sparing lower-risk patients from unnecessary treatment-related toxicities. This is particularly relevant for the large proportion of patients with cSCC over 65 years of age,17 many of whom are Medicare beneficiaries.
The recognition of this poster at the NCCN 2025 Annual Conference as one of the top five Blue Ribbon abstracts emphasizes its possible influence on clinical guidelines and treatment decision-making. By integrating the 40-GEP test with BWH staging, clinicians can achieve a more refined risk stratification of NCCN high-risk and very high-risk groups, leading to more personalized treatment plans.






