Meeting Summary
The main objectives of this symposium were to review the importance of topical therapies in the treatment of psoriasis and the unmet clinical and patient quality of life (QoL) needs that still exist, to discuss the innovation seen with reformulations of existing active pharmaceutical ingredients (API), and to align changes in future dermatology practice with these topical treatment innovations. Mr Fernández introduced the topic of ‘looking to the future’, with a wide-ranging, big-picture view of the changing face of medical practice and the increasing role of technology, including specific examples of how these trends will affect dermatology practice. Prof Surber built on the theme of innovation to discuss how novel products and approaches can be pursued in dermatology, particularly in the area of topical psoriasis treatments. Prof Surber’s presentation and the subsequent talk by Dr Bewley described how innovations can translate into improved patient outcomes in key areas, including psoriasis control, itching, sleep, and overall health-related QoL. Prof Bonnekoh tied the various threads of the symposium together by showing how the new technological and pharmacological options could help clinicians evolve their overall approach to long-term topical management of psoriasis, moving from a more reactive mindset to safe and effective proactive control. Finally, the audience was given the opportunity to ask questions in a brief panel discussion.
The Future of Medicine Versus the Medicine of the Future: The Future is Already Here
Mister Jorge Juan Fernández Garcia
How the World is Changing
Although many commentators have attempted to anticipate ‘the future of medicine’, it is perhaps more relevant to turn the concept around and look towards ‘the medicine of the future’: the ways in which medical practice will be different from what we know today and the trends that are already being established. In order to provide optimal, patient-centred care, it is important to recognise how the opportunities that are available to physicians and patients are changing, particularly with regard to digital innovations and changes in the ways that people communicate with each other in the delivery of healthcare.
Broadly speaking, healthcare has experienced three major revolutions: the hygiene revolution of the 1800s, the pharmaceutical revolution of the mid-20th century, and the data revolution that is currently ongoing. As medicine becomes more of an information technology, the pace of change is growing exponentially. Although it could be possible to call this ‘progress’, the term carries the implication that everything will improve, but the relative importance of different institutions and processes will stay the same; what we are experiencing here is more accurately described as ‘disruption’, where there is more extensive change and some previously essential concepts and organisations may disappear altogether.
Trends in Healthcare
Among several key trends that physicians should track, virtual visits are on the rise. Indeed, most communications between patients and physicians will likely be digital. An analysis by the Kaiser Permanente company found that consultations by e-mail or through other online platforms have more than doubled in the past 5 years and are on track to outnumber in-person visits by 2018.1 Since office visits are not declining substantially, these virtual visits represent a complement to in-person care, not a substitution. In dermatology, several online services now exist for patients to receive a virtual consultation with a board-certified physician for a small fee; these services could represent an additional or alternative revenue source for interested dermatologists.
In addition, patient-to-patient interactions are beginning to outpace patient-to-physician interactions, as digital forums and other outlets allow patients to take more ownership of their own health and care. Patients are motivated to share what they have experienced so that they can help others, and physicians should be aware of this dynamic and be prepared to support it with their own clinical expert perspectives. The smartphone will continue to be crucial in providing healthcare. In particular, the development of peripheral devices, such as thermometers and glucometers, will revolutionise the way that patients manage their own monitoring and treatment.
The growth of big data in healthcare is inspiring, but it also presents significant challenges for interpreting the overwhelming quantities of information we are now able to collect. Healthcare is, therefore, becoming less of a science problem and more of an information problem. Since computer algorithms are often faster and more efficient at analysing large datasets than human researchers, our role then shifts towards transforming those data into insights.
Artificial intelligence systems are now being trained to assist in medical diagnosis and treatment. For example, neural networks can evaluate potentially malignant moles for melanoma, with an accuracy rate at least as high as that of experienced dermatologists.2 Physicians should not fear ‘being replaced by robots’, rather our focus should be on how clinicians can use their expertise to work most effectively with the strengths and abilities of digital tools in order to create algorithms that will optimise patient care.
Implications for Dermatologists
The digital revolution is less about healthcare becoming digital and more about shifting towards a patient-centric approach that is driven by digital tools. The overall role of the physician is changing, from that of a ‘sage’ who holds all the answers, to that of a ‘facilitator’ who helps co-ordinate the multiple facets of patient care. Dermatologists should reflect on how this could make them a better physician if they delegated certain portions of their role, either to computer algorithms or to the patients. With the rapid pace of change, we have the potential to change the way that healthcare is delivered within the next 2–3 years, as long as we recognise and work effectively with the opportunities that surround us.
Reasons to Apply Topical Formulation Innovation in Psoriasis
Professor Christian Surber
Topical Treatments for Psoriasis: A Long History of Innovation
For as long as psoriasis has been recognised as a clinical entity, clinicians and researchers have been striving towards better treatment outcomes through topical product innovation. From the early days of arsenic and tar-based topical products through to the development of corticosteroids, phototherapy, retinoids, and immunosuppressive regimens, innovators have aimed to maximise the clinical value of the API and simplify therapy to support patient adherence.3,4 In addition to new API, we will be able to further improve clinical outcomes by creating novel formulations and vehicle concepts, and by developing application strategies that maximise the impact of existing or new API. This presentation will focus on a recent case showing how a new and unique vehicle or formulation concept can further augment the clinical effect of the fixed-dose combination of calcipotriol and betamethasone dipropionate (cal/BD) in psoriasis.
What Are Formulations or Vehicles?
The conventional view of topical product formulations or vehicles tends to break products into categories based either on the effect of the vehicle itself (e.g. lubricants, moisturisers), a description of the vehicle format (e.g. ointments, lotions), or a mode of administration (e.g. roll-ons, sprays). The obvious phenomenon that a vehicle can have a significant impact on clinical outcomes led to the false, but widely held, view that for corticosteroids the ointment vehicle format is more potent than the cream vehicle format, and the cream vehicle format is more potent than the lotion vehicle format.5,6 The fact is, vehicles containing volatile ingredients (e.g. water, alcohol) will change their format once applied onto the skin. This process has been coined as a “metamorphosis of the vehicle”.7 The sum of the vehicle ingredients on the skin after evaporation of all volatile vehicle ingredients is decisive for the behaviour of an API within the vehicle and the impact of the vehicle on the skin barrier function.
How Can We Innovate with Vehicles?
The fixed-dose combination of cal/BD is available in a number of different vehicle formats, including gels (for the skin and scalp) and ointments. Recently, these API have been reformulated into a novel foam spray format containing volatile ingredients that instantly evaporate after the product is applied onto the skin, leaving the API and the non-volatile ingredients behind. This metamorphosis of the product affects the behaviour of the API in the vehicle on the skin and, hence, their effect. Once the volatile components have evaporated, the remaining ingredients provide a transient increase in skin permeability through occlusion. On the API side, evaporation of the volatile vehicle ingredients concentrates the API into a supersaturated state, in which there is more drug dissolved in the remaining vehicle ingredients than could be dissolved under normal conditions.8 Both these phenomena (occlusion and supersaturation) lead to an increase in percutaneous absorption of the API, since the skin becomes more permeable and the concentration gradient of API across the skin increases considerably.
Initial data from clinical trials of the cal/BD foam spray formulation suggest that the novel vehicle can improve patient outcomes relative to the same API in a different vehicle. Compared to the standard ointment formulation of cal/BD, the foam spray was associated with increased rates of treatment success after 4 weeks of treatment (Figure 1).9

Figure 1: Treatment success rates with the foam spray and ointment formulations of calcipotriol/ betamethasone dipropionate.
Treatment success: defined as ‘clear’ or ‘almost clear’ for patients with a baseline PGA of moderate or severe, and as ‘clear’ for patients with a baseline PGA of mild.
cal/BD: calcipotriol/betamethasone dipropionate; PGA: Physician’s Global Assessment.
Adapted from Koo et al.9
Can We Continue to Innovate?
Although the fixed-dose combination of a vitamin D analogue and a corticosteroid is currently the gold standard for topical management of psoriasis, in the future other novel API may demonstrate similar or even better effects. Regardless of the specific API used, the vehicle or formulation will also be key for treatment success through its effects on both the API itself and the barrier function of the skin. Novel formulations are also crucial for moving towards a patient-centred approach to treatment, since many of the factors that affect patient adherence to topical treatment are related to vehicles and application issues.10 Looking to the future, topical pharmacotherapy will be further improved through the development of products with improved cosmetic and pharmacologic properties, as well as intelligent digital applications that help patients feel empowered and supported at all stages of their psoriasis journey.
Why Managing Itch and Psychosocial Comorbidities Experienced by Patients With Psoriasis is so Important
Doctor Anthony Bewley
Impact of Psoriasis Symptoms and Comorbidities on Patient Wellbeing: Focus on Itch and Psychological Comorbidities
The most commonly recognised and appreciated symptoms of psoriasis (e.g. plaque cracking, flaking/ scaling, and erythema) have traditionally served as the clinical focus in psoriasis diagnosis and management. However, psoriasis has many additional symptoms and comorbidities that contribute to the patient’s overall wellbeing and are often underestimated.11 For example, psoriasis was historically thought of as a dermatosis that does not itch, but we now know that itch is a common symptom, present to some degree in 70% of people with psoriasis.12 Additional physical comorbidities, such as psoriatic arthritis, Crohn’s disease, and metabolic syndrome occur more frequently in psoriatic patients than in the general population, with subsequent effects on morbidity and mortality.13
Psoriasis is also associated with an increased risk of a number of psychological comorbidities. Depression is widespread in psoriasis patients14 and this population is twice as likely to have suicidal thoughts than the general public.15 If applied to the UK population, these statistics would correspond to roughly 300 people annually who choose to die rather than continue living with their psoriasis. Cumulatively, the various comorbidities, symptoms, and stigma of psoriasis significantly impair overall health, psychological state, and QoL over a patient’s lifetime.13 The impact of psoriasis and its comorbidities on patient wellbeing is on par with that of other serious chronic diseases such as cancer, heart disease, and diabetes.16
Focus on Itch and Sleep Disturbances as Determinants of Quality of Life
Itching is one of the five factors most closely associated with reduced mental and emotional wellbeing in people with psoriasis.16 Patients report that itch has a negative effect on specific elements of QoL, including mood, concentration, and sleep, and that psoriasis-related itch correlates with decreased QoL to a greater extent than pain or fatigue. Since stress, poor mood, and impaired sleep have in turn been identified as key aggravating factors of itch, many patients face a vicious cycle of inter-related deterioration of both itch and QoL.17 Insomnia is common in psoriasis patients and can have a major impact on overall QoL and psychological wellbeing. Itching and pain are two of the important factors linked to insomnia in people with psoriasis; effective management of psoriasis and its associated itch and pain, therefore, has the potential to improve sleep and overall QoL.18
The Impact of Effective Psoriasis Control on Itch, Sleep, and Quality of Life
Clinical trials of systemic biologic agents have demonstrated how controlling the cutaneous symptoms of psoriasis (e.g. Psoriasis Area Severity Index [PASI] improvement) can translate into improvements in itch, QoL, and sleep. A post-hoc analysis of the PRISTINE trial found that most patients with moderate-to-severe psoriasis experienced significant improvements in itch scores during 24 weeks of etanercept treatment; patients with the greatest reduction in itch also experienced the highest level of improvement in QoL.19 Quantity and quality of sleep were also improved with etanercept treatment and these changes translated into further QoL ameliorations.20
On the topical therapy side, the novel foam spray formulation of cal/BD holds the potential to provide itch relief, QoL improvements, and sleep amelioration for a broader population. In clinical trials, cal/BD foam spray provided a rapid and marked relief of itch within the first week of therapy.9 More than one-third (36.8%) of patients reported a 70% reduction in itch by Day 3 of treatment, with most patients (83.5%) achieving this level of itch reduction by the end of the 4-week study; at both time points, itch reduction was significantly greater with the cal/BD foam spray than with its vehicle alone (Figure 2).21 These improvements in itch also translated into significant reductions in itch-related sleep loss21 and improvements in overall health-related QoL as measured by the Dermatology Life Quality Index (DLQI).22
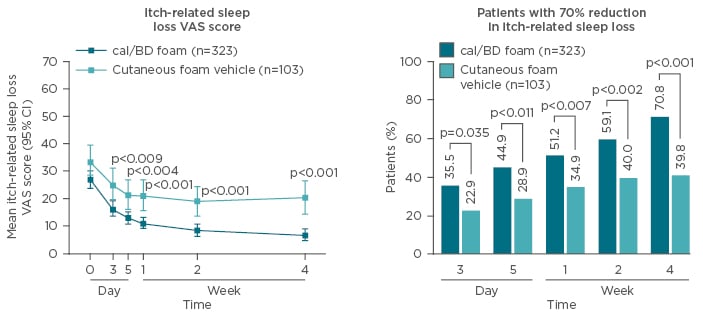
Figure 2: Improvements in overall itch VAS score and patients experiencing significant (70%) itch reduction with cal/BD foam spray versus vehicle alone.
cal/BD: calcipotriol/betamethasone dipropionate; CI: confidence interval; VAS: Visual Analogue Scale.
Adapted from Leonardi et al.21
Conclusions and Future Directions
With the advent of new data-mining tools and novel approaches to therapy, it is becoming easier for clinicians to provide care that is tailored not only to the patient’s clinical signs and symptoms but also to his or her personal experience of the disease. A recent study found that patients on topical psoriasis treatment could be broadly clustered into groups based on their perception of the holistic burden of all aspects of their disease (skin symptoms, comorbidities, psychosocial impact, and treatment experience).23 This type of patient profiling and the recognition of patients’ different treatment and educational needs is one promising strategy for moving towards more personalised, patient-centred care. Another key approach for optimising patients’ holistic wellbeing is the use of multidisciplinary teams that incorporate other facets of psoriasis such as rheumatology and gastroenterology. Finally, many new medications and approaches are under investigation for the management of itch, including antidepressants, hand-held phototherapies, and psychotherapeutic talk therapies.24 Together, these tools and strategies give dermatologists a wide range of choices for tailoring therapy to provide the greatest improvements in patients’ holistic QoL.
Taking Control Over Psoriasis: From Flare-up to Proactive Management
Professor Bernd Bonnekoh
The Current Topical Psoriasis Treatment Landscape
Since psoriasis is a chronic incurable disease, the treatment plan must consider how best to manage the condition over the course of a patient’s lifetime. The current management of psoriasis is extremely complex, with a wide variety of medication options available and a large number of patient factors for physicians to consider in their multi-parameter assessment of the disease (Figure 3). As the integration of big data into clinical practice becomes more widespread, clinicians’ reality is moving more towards a shared decision-making framework supported equally by the patient’s input, the available treatment and support choices, and the dermatologist’s experience and clinical judgement.
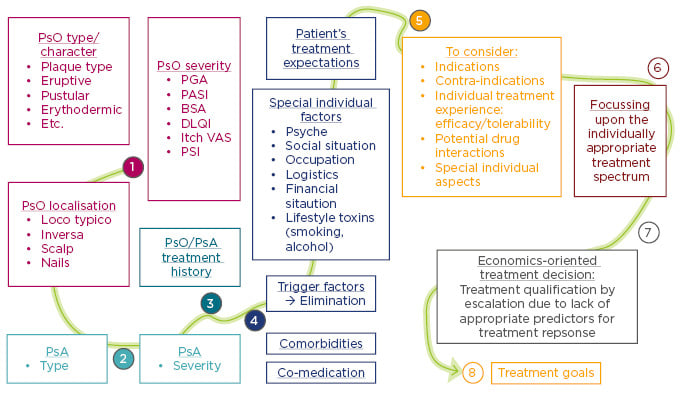
Figure 3: From multi-parameter psoriasis assessment (1–5), to the treatment decision (6–7), and treatment goals (8).
BSA: body surface area; DLQI: Dermatology Life Quality Index; PASI: Psoriasis Area Severity Index; PGA: Physician Global Assessment; PsA: psoriatic arthritis; PSI: Psoriasis Symptom Inventory; PsO: psoriasis; VAS: Visual Analogue Scale.
Currently, the overall approach to psoriasis tends to use topical products as initial monotherapy for mild-to-moderate disease, and considers adding them as an adjunct to ultraviolet and/or systemic therapy for moderate-to-severe disease. Combinations of topical ingredients can be either sequential or simultaneous (e.g. fixed-dose combinations). In general, a topical product should be applied daily in the initial induction and stabilisation period; however, the approach to longer-term maintenance is more loosely defined and usually relies on a reactive, on-demand approach to any flares that may occur.
Moving Towards Safe, Effective, and Proactive Long-Term Topical Use
Topicals will likely remain the cornerstone of treatment for many psoriasis patients; it is, therefore, essential to consider how to use them effectively and promote optimal patient adherence in the long term. Clinical practice guidelines from various national societies offer only indirect recommendations for long-term use of topical medications, and the clinical literature on long-term, proactive topical treatment of psoriasis is likewise very sparse. Given the lack of published material specific to psoriasis, it may be useful to look at the model of a proactive approach in another long-term skin condition: atopic dermatitis. Here, proactive maintenance treatment with tacrolimus ointment twice-weekly, plus additional twice-daily reactive treatment in case of a flare-up, is associated with a significantly delayed time to first flare, compared with standard reactive flare treatment in both children and adults.25,26
There appears to be an unmet need in the psoriasis community for this type of proactive approach. A recent survey of dermatologists in Germany indicated that more than half of respondents were using proactive treatment (e.g. once-weekly in nearly cleared lesions) in spite of products not being licenced for this type of use. This practice is supported by a meta-analysis of prospective trials that concluded that long-term maintenance treatment (1–2 times weekly) with two-compound formulations was effective in daily practice, had favourable tolerability and economic benefit, and promoted proactive patient involvement.27 Further support for the long-term safety and tolerability of fixed-dose combinations is anticipated from the currently ongoing PSO-LONG trial, which is evaluating a twice-weekly maintenance regimen of cal/BD foam spray over a period of ≤52 weeks.
Looking Towards the Future
Topical therapy is currently built on a solid foundation of effective, tolerable, and easy-to-use products, and the concept of proactive long-term management is starting to become established based on this foundation. In order to improve treatment success and long-term adherence, clinicians can support their patients by setting a clear schedule and empowering patients through knowledge and shared decision-making. As we continue to build this approach into the future, we may also benefit from new drugs, formulations, and modes of application, as well as new digital devices and strategies to keep patients on track and reward them for successfully following their treatment programme.
Question and Answer Session
Q: What advice would you give to dermatologists to help them make the most effective use of the huge amount of information available through big data?
A: Mr Fernández suggested that clinicians could focus their research by asking: “What kind of information, if I could find it, would change how I manage the patient?”. Dr Bewley added that there will always be a need for clinicians’ expertise, especially as more patients research their own conditions online; physicians’ expert input can help personalise that information and place it in the appropriate context. He also noted that it is important to recognise that in a consultation there are two experts in the room, the physician who is an expert in medicine, but also the patient who is an expert in his or her own experience of the disease.
Q: How can care of psoriasis patients be most effectively co-ordinated between general practitioners and specialists?
A: Dr Bewley replied that the ‘ownership’ of a patient’s care should rest with whichever physician is able to provide the most meaningful and appropriate management, whether that is a general practitioner or a specialist. He mentioned that one of the key aspects of psoriasis care is ensuring that the patient’s expectations of treatment are understood and that the physician is able to develop a plan to meet those expectations and evaluate treatment success.
Q: If a two-compound product containing a steroid is used proactively over the long term, how do we motivate patient adherence to treatment? In atopic dermatitis, this is less of a concern since treatment is non-steroidal.
A: Prof Bonnekoh replied that the data for longterm use of two-compound products show no important safety concerns over a period of use of ≤1 year and that anecdotally many dermatologists know of patients who have used topical corticosteroids for decades without any problems. Dr Bewley added that steroid phobia is still common among patients and that physicians should be careful not to simply dismiss these concerns, but rather to highlight their own experience using these products over the long term. Prof Bonnekoh also mentioned that patient counselling could include examples from other conditions, such as chronic obstructive pulmonary disease, where eroids are routinely used over many years and the safety profile has been well characterised.







