Held in the city of Paris, France, on the 12th–16th September 2018, the 27th European Academy of Dermatology and Venereology (EADV) Congress lived up to the enormous expectations preceding it. With a programme peppered with 180 scientific sessions to bring the audience up to speed with the latest movements in the dermatology world, the stage was set for a truly spectacular 5-day event.
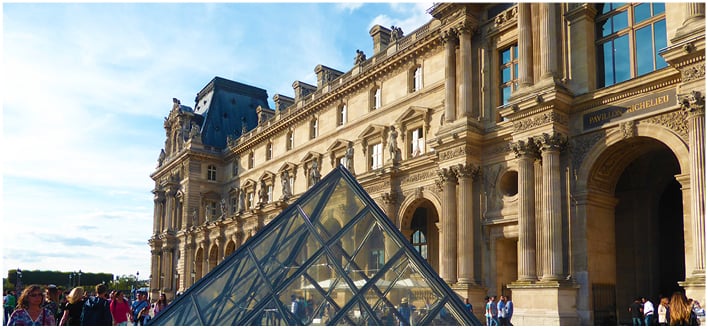
Home to the iconic Eiffel Tower and draped in years’ worth of iconic history, Paris was the perfect backdrop for this year’s EADV Congress focussing on clinical oncology. Topics throughout the event ranged from genetic predisposition and targeting the tumour environment to rare skin tumours and the effects of chemotherapy and targeted therapy. Prof Luca Borradori took to the stage for the opening address to a rousing applause from the audience. In his final presidential opening of a EADV Congress, Prof Borradori spoke of his fondness for Paris and how privileged he felt to be able to host his final EADV Congress as EADV President in the city that he trained in. Alongside urging the EADV attendees to explore the wonderful city, Prof Borradori also incited excitement for the forthcoming event by highlighting the astonishing array of scientific sessions, with 700 speakers from 60 countries, and the much-anticipated 2,500 abstracts on display.
The scientific programme also included three plenary lectures, including presentations from six of the most prominent and prolific dermatology specialists from across Europe and the USA. Beginning on the first day of the congress, Dr Warren Piette, Chicago, Illinois, USA, presented on the consequences of differential diagnosis on the treatment of vasculitis and vasculopathies, shortly followed by a presentation on atopic dermatitis and skin infection by Dr Tilo Biedermann, Munich, Germany. The following day’s plenary lecture presentation saw Dr Christian Blank, Amsterdam, Netherlands, ask the poignant question of whether we can cure metastatic melanoma. Concluding the plenary lectures on Saturday, Dr Elisabeth Grice, Philadelphia, Pennsylvania, USA, presented on the skin microbiome and its link to health and disease, while Dr Veronica Kinsler, London, UK, took the audience through the diagnosis, spectrum, and therapy of congenital nevi, and, finally, Dr Leena Bruckner-Tuderman, Freiburg, Germany, presented on a variety of skin fragility syndromes.
Prof Borradori encouraged all attendees to visit the patient society village, which was open for the duration of the congress where clinicians and medical professionals can speak to patients, patient associations, and societies to understand patient expectations, wishes, and needs; after all, patients are at the centre and the reason of all that the medical community do.
Concluding the 5-day event, ‘Aesthetic Sunday’ was a day much-anticipated by all. Set up in response to requests for further training in aesthetics and cosmetic dermatology, the event included sessions at both basic and advanced levels of cosmetic dermatology understanding. Topics covered by 10 of the most renowned specialists in cosmetic and aesthetic dermatology included fillers; botulinum toxin; peels; scars; energy-based devices, such as lasers; as well as the associated complications with the aforementioned topics.
For a further comprehensive review of the thought-provoking EADV Congress 2018, please read on to find out more about the call for greater sharing of information regarding HPV vaccinations, strategies and programmes to improve psoriasis patient quality of life by reducing stigmatisation, the risks associated with sun exposure for outdoor workers, and the debate surrounding tattoo regulations coming into line with those for cosmetic procedures.
The EMJ team thoroughly enjoyed attending this year’s EADV Congress and is already looking forward to and preparing for the already much-anticipated EADV Congress 2019, which is to be held in the magnificent city of Madrid, Spain.
Improving Social Acceptance for Psoriasis Patients
APPROXIMATELY 125 million people across the globe are affected by psoriasis, with 2 million in Germany alone. Although not curable, the skin disease is managed through the implementation of multidisciplinary therapeutic strategies that can improve patient quality of life. However, >60% of patients experience episodes of depression and negative effects on their quality of life, especially if the psoriasis plaques affect their face, hairline, or hands. New strategies and programmes with the aim of improving patient quality of life by reducing stigmatisation were outlined in a EADV press release dated 12th September 2018.
Alongside the physical symptoms associated with the disease, psoriasis patients often face rejection, disgust, fear of contagion, and exclusion. According to a recent FORSA survey of >2,000 people, 10% believed that psoriasis might be infectious and 20% stated that they would not enter a swimming pool with an individual with psoriasis. In 2014, the World Health Organization (WHO) adopted a resolution that elevated psoriasis to a serious non-communicable disease. The long-term aim of this WHO resolution, and the 2016 Report on Psoriasis penned by field experts, is to sensitise the public to the disease and remove the stigma associated with the condition. “One of the main demands of the WHO was therefore to disseminate knowledge about psoriasis among the population and to show clearly that these people do not deserve to be stigmatised,” explained Prof Dr Swen Malte John, University of Osnabrueck, Neuer Graben, Germany.
In 2018, the ongoing ECHT EVAL study was initiated. The study aims to gather information and generate strategies to educate the general public about skin disease. Additionally, the Action Network Against Stigmatisation group has developed a 2018–2020 programme. Similarly to the ECHT EVAL study, the programme aims to improve social acceptance of the disease and drive the implantation of the WHO recommendations. Although a cure for the disease is not available, the work of the WHO, Action Network Against Stigmatisation, and the ECHT EVAL study will hopefully improve the quality of life for the millions of people living with the disease.
Sun Exposure Risks for Outdoor Workers
THE STANDARD erythemal dose (SED) was developed as an erythemally weighted measure of sun exposure, independent of skin type. The World Health Organization (WHO) set a daily limit of 130 SED; however, new data collated by the GENESIS-UV project, and reported in a EADV press release dated 12th September 2018, has highlighted that this daily limit is regularly exceeded 5-fold by outdoor workers in Germany.
Statistics from 2017 revealed that regular SED exposure 5-fold higher than the WHO recommended limit was associated with an increased incidence of occupational skin cancer. It was further noted that the summer of 2017 was not as sunny as this year’s record-breaking summer in Europe. “A further increase in the future can be expected because of the sunniest summer in a century,” explained Prof Dr Swen Malte John, University of Osnabrueck, Neuer Graben, Germany.
The majority of skin cancer cases involve non-melanoma skin cancer, such as basal cell carcinoma, squamous cell carcinoma, and actinic keratoses, and outdoor workers are at particular risk. It is widely reported that this proportion of the population has a 43% increased risk of developing basal cell carcinoma, while their risk of squamous cell carcinoma is doubled. Furthermore, people that have worked outdoors for ≥5 years have a 3-fold higher risk of developing basal cell carcinoma, squamous cell carcinoma, and actinic keratoses compared with their indoor working counterparts. Furthermore, one study has shown that outdoor workers are also at an even greater risk of developing particularly aggressive forms of non-melanoma skin cancer.
An additional problem across Europe is the lack of consistency in the recording and reporting of non-melanoma skin cancer cases; for example, in Italy only 96 cases of occupational-related cancer between 2010 and 2014 were recorded, despite the actual estimates being much higher. In response to this, the EADV is promoting the standardised registration of all cases of white skin cancer.
The risk of developing non-melanoma occupational skin cancer is clear and the EADV has encouraged the implantation of simple sun protection strategies for those working outdoors, including mounting sun shields, avoiding work during the hottest part of the day, and providing sun protection factor 50+ sunblocks.

Call for Increased Regulations Around Tattoo Inks
“Tattoo inks should at least meet the same safety standards as cosmetic products,” declared Dr Christa De Cuyper, a EADV Board Member. As reported in a EADV press release dated 12th September 2018, Dr De Cuyper reiterated the EADV’s call for proper safety testing of tattoo inks and for tattoos to be held to higher safety standards than they currently are. Such a call is of great importance, especially considering that tattoos are becoming increasingly popular in the Western world, with approximately 10% of the German, Finnish, and French populations having a tattoo.
The EADV argues that current regulations do not go far enough to ensure satisfactory safety standards. Currently, the quality and sterility of tattoo inks is not controlled, which raises the potential for infection. Indeed, a Danish study that investigated 58 new tattoo inks showed that 10% were contaminated by bacteria, highlighting the risk of potential infection following tattooing. Additionally, the current regulations are not believed to be stringent enough to ensure that tattoo ink is not toxic and does not cause allergic reactions. Further to this, some of the pigments found in tattoo inks are not approved for use in cosmetic products because they have not been listed by the Scientific Committee for Consumer Products (SCCP).
Although the European Chemical Agency (ECHA) has prepared pathways for ensuring improved tattoo ink quality that are expected to be published by the end of 2018, the EADV does not believe these new proposals go far enough. Dr De Cuyper declared: “To eliminate carcinogenic substances and to limit long-term toxic effects, strict measures and well-defined safety limits are needed with appropriate analytical methods for controlling such use; the ECHA proposals do not provide adequate solutions to meet these requirements.” Dr De Cuyper went on to suggest that perhaps tattoo inks should be held to even higher standards than cosmetic products as they are injected under the skin and there is evidence that ingredients from tattoo inks are ingested into the body.
This call for better safety standards for tattoos will no doubt ensure that all those who choose to have a tattoo can be assured that they will be conducted in the safest way possible.
EADV Calls for Greater Information Sharing about HPV Vaccine
A vaccine currently exists that would prevent genital warts associated with HPV and HPV-associated cancers, so why are these conditions present today? In fact, in 2008, there were approximately 529,000 new cases of cervical cancer globally, which is the most common type of cancer associated with HPV. The World Health Organization (WHO) recommends that girls should be vaccinated as a matter of priority in order to help prevent and control cervical cancer. However, vaccination programme participation rates are still too low to impact the prevalence of cervical cancer in many countries. It was in this context at the EADV Congress that the EADV outlined recommendations for tackling this problem, as reported in a EADV press release dated 12th September 2018.
As already noted, nationwide participation in HPV vaccination programmes is low in many countries. For instance, in Germany only 40% of girls are vaccinated and only a very small percentage of boys. There is no need for this disparity in vaccination rates between the sexes, as men are infected just as frequently with HPV as women and HPV infection in men can lead to the development of penile and anal cancer. An additional reason to ensure men are also vaccinated against HPV is that this will make achieving herd immunity easier. It is estimated that 85% of boys need to receive the HPV vaccine in order to contribute to herd immunity.
The EADV attributed the low vaccination rate to a lack of dissemination of information within the population, both in regard to the general public and policymakers. Prof Mihael Skerlev, Chairman, EADV taskforce for HPV infection, commented: “The health authorities do not seem to have realised the cost savings that vaccination can produce for the health systems, even direct and immediate cost savings, over and beyond the prevention of cancer, simply as a result of a declining incidence of external genital warts.” Therefore, the EADV recommended a strategy for targeted information campaigns across platforms used by the desired audience, such as across social media to reach younger generations. It is believed that this policy will result in the successful breaking of the HPV infection chain.

Dupixent (dupilumab) Significantly Improves Disease Severity in Adolescents with Moderate-to-Severe Atopic Dermatitis
Dupixent® (dupilumab) (Sanofi, Bridgewater, New Jersey, USA and Regeneron Pharmaceuticals, Inc, Eastview, New York, USA), an IL-4 and IL-13 inhibitor, has been shown for the first time to significantly improve symptoms of atopic dermatitis (AD) along with quality of life measurements in adolescents with moderate-to-severe (MTS) AD, according to a late-breaking oral presentation at EADV on the 15th September 2018.
Dupixent is already approved for the treatment of MTS AD in adults, but this trial assessed Dupixent’s safety and efficacy in an adolescent population. This Phase III trial is also the first trial of a biologic in patients 12–17 years old with MTS AD that could not be controlled by topical therapies. A total of 251 patients were included in the 16-week long trial and were randomised to three treatment arms:
- Treatment with Dupixent at a dose of 200 mg or 300 mg (based on weight) every 2 weeks, with an initial dose of 400 mg or 600 mg, respectively.
- Treated with 300 mg Dupixent every 4 weeks with an initial dose of 600 mg.
- Treated with placebo every 2 weeks.
The coprimary endpoint outside of the USA was 75% improvement in Eczema Area and Severity Index (EASI-75) at 16 weeks; in the USA, the primary endpoint was the proportion of patients achieving Investigator’s Global Assessment (IGA) score of 0 (clear) or 1 (almost clear).
Results at 16 weeks showed that 41.5% and 38.0% of patients who received Dupixent every 2 weeks and every 4 weeks, respectively, achieved ≥75% EASI-75 compared to 8% in the placebo group (p<0.001). Clear or almost clear IGA scores were achieved by 24% of patients who received weight-based dosing and by 18% of those receiving fixed-dose Dupixent every 4 weeks, compared to 2% of the placebo group (p<0.001).
Results of the secondary endpoints were just as encouraging; 49% and 39% of patients who received Dupixent every 2 weeks and every 4 weeks, respectively, achieved a minimum of a 3-point improvement in the Peak Pruritus Numerical Scale compared to 9% of the placebo group (p<0.001). Significant improvements in quality of life as measured by the Children’s Dermatology Life Quality Index (CDLQI) and patient reported symptoms as measured by the Patient-Orientated Eczema Measure (POEM) compared with placebo (p<0.001) were also observed.
Adverse effects were reported in 72% of patients in the Dupixent every 2 weeks group, 64% of patients in the Dupixent every 4 weeks group, and 69% in the placebo group.
Dr Amy S. Paller, Director, Northwestern University Skin Disease Research Center, Northwestern University, Evanston, Illinois, USA, and principal investigator for the trial, commented on the importance of these results: “The results we are presenting today show the potential for Dupixent in adolescents to not only help clear the skin and reduce itching, but also improve certain aspects of quality of life in adolescents who may be dealing with these unbearable symptoms.”

A Historical Look at the Hôpital Saint-Louis
The arrival of the EADV Congress to Paris offers the perfect opportunity to dig beneath the surface and discover more of the city’s rich dermatological past.
Although today the Hôpital Saint-Louis is well-known for its specialism in dermatology, the road it took to achieve this accolade is an interesting one that started in 1606 when a new plague was spreading across France. Although King Henry IV had fled the city in an effort to ensure his own safety, he was petitioned by his advisors to establish a hospital for the effective treatment of the plague. In response, he ordered the construction of the Hôpital Saint-Louis, which was completed in 1610.
The next milestone in the history of the Hôpital Saint-Louis was at the time of the French Revolution. The French Revolution, which lasted from 1789–99, was transformative for hospitals: in 1801, the city’s hospitals were reorganised into general and specialised institutions. This saw the Hôpital Saint-Louis designated for the treatment of contagious diseases, such as scabies, and chronic conditions, such as cutaneous ulcers. During this time, Jean-Louis-Marc Alibert was appointed to the hospital, and it was under his influence that the hospital grew to become a focal point for dermatological teachings and learnings. This was further emphasised in 1889 when the hospital was the location for the first world congress of dermatology.
One of the most impressive collections in the hospital museum is the moulage collection, which comprises >4,800 moulages in various states of repair. It is believed that the beginning of this collection was commissioned by Charles Lailler, a French dermatologist, who wanted an artist to produce realistic depictions of skin diseases. Fortuitously, he walked past a small shop that sold papier-mâché fruit, and later found the artist, Jules Pierre Francois Baretta. Baretta was later tasked with creating dermatological moulages for Lailler. After initially working privately for Lailler, Baretta became the hospital’s modeller in 1870. He also sold models to other hospitals and to dermatologists from abroad. By the time Baretta retired in 1914, it is estimated he had cast 3,000 models for the Hôpital Saint-Louis. Barret’s successors went on to add to the collection, with the final model created in 1958.
The Creation of Baretta’s Moulages
- The making of moulages is a process shrouded in secrecy. Barretta remained tight-lipped about the techniques he used.
- This secrecy is probably one of the main reasons why Baretta’s moulages differ somewhat from those created by the moulages who succeeded him.
- Analysis conducted in the laboratory has shown that Baretta’s moulages were composed of a mixture of beeswax and a resin believed to be gutta-percha.
- Some of the colours may have been incorporated into the initial mixture.
- The mixture was heated to a temperature of roughly 200°C and then poured into a plaster cast.
- Following casting, Baretta would have most likely painted the finer details by hand.
Although in the present day moulages have long since been superseded by photographs in the teaching of dermatology, they represent a fascinating historical perspective, shedding light on historic teaching methods and the representation of illness that can still be studied today.
Quality of Life and Psychosocial Issue in Skin Disease
An Interview with Dr Francesca Sampogna
Awareness of the impact that skin diseases can have on a patient’s quality of life has improved markedly within the dermatology community in recent years. Yet the extent to which these symptomatic and psychosocial issues affect the daily lives of patients is still being uncovered in daily practice. During the recent EADV Congress in Paris, France, the EMJ took the opportunity to speak to Dr Francesca Sampogna, a leading researcher in this area from the Clinical Epidemiology Unit, Istituto Dermopatico dell’Immacolata IDI-IRCCS, Rome, Italy. In our interview, we discussed the study she presented during this event, entitled: ‘Sexual problems and quality of life in patients with skin diseases,’ before talking about trends in the field and new initiatives taking place to help clinicians assess the impact of the skin disease on a patient’s quality of life.
Growth in Understanding
Dr Sampogna described how coverage of quality of life has grown in recent times at major dermatological meetings, such as the annual EADV Congress, although she would still like to see sessions on this topic gain greater prominence than they currently do. This is something that she and colleagues who work in this area are continually emphasising. “Around 15 years ago there were almost no specific sessions on quality of life,” she explained. “Now, we always have specific sessions on quality of life and psychosocial impact of dermatological conditions.”
In general, there has been a vast improvement in the appreciation of the symptomatic and psychological aspects of skin diseases during the course of Dr Sampogna’s career, which has changed the way these conditions are looked at and treated. “If you read books 30 years ago, they say that psoriasis is an asymptomatic disease, but if you look at data it is not true at all because it causes a lot of itching, burning, and pain. And psoriasis patients also have a lot of psychosocial problems, especially in relationships and social life, which is its main impact,” she elucidated. “Atopic dermatitis also has a similar effect in terms of itch and social life. In our group, we studied vitiligo which is a chronic condition but has no symptoms, meaning it was previously considered as just a cosmetic problem with white spots being the only issue. But we observed that it has a huge impact from a psychosocial point of view. This shows that diseases that are not severe from a clinical point of view can have a major psychological impact.”
This increase in awareness has led to the stage where clinical trials will generally always include quality of life measurements, which is undoubtedly a big step forward in ensuring that doctors are more aware of the non-clinical impact of new treatments.
Bridging the Gap
Nevertheless, Dr Sampogna does believe there remains a separation between researchers and clinicians in dermatology, and this can prevent new discoveries being translated into clinical practice as much as they could be. Continuously finding scenarios in which professionals from the two areas can interact with each other is therefore crucial in bridging this gap. “The problem is the connection with clinical practice. Dermatologists who are also involved in research will of course change their clinical practice. But it is difficult for all the dermatologists in the world to have this information, so there is a gap, a disconnect. That is why it is so important to give information at congresses such as EADV,” she said.
Study at EADV
A study presented by Dr Sampogna at this year’s event primarily analysed the sexual problems faced by dermatology patients. Dr Sampogna’s particular analyses came from a large multicentre study of almost 3,500 dermatology patients covering 13 European countries regarding psychological problems they face. Here, data were collected from a single question from the Dermatology Life Quality Index (DLQI) questionnaire, which read: ‘Over the last week, how much has your skin caused any sexual difficulties?’ Overall, more than 11% of respondents reported problems in their sexual life, and the results also showed that this was especially prominent in certain conditions. Hidradenitis suppurativa was the highest of these, at 43%, and other skin diseases in which it was also a notable issue included pruritis and atopic dermatitis. In the view of Dr Sampogna, these findings demonstrate the benefits a simple questionnaire can have in informing a doctor about the quality of life issues their patient is facing. “One of our main conclusions is that a simple question such as this can help to deal with a sensitive issue because it is very difficult for a physician to ask; therefore, if you give a questionnaire an answer can be written,” she added.
Measuring Quality of Life
Developing tools such as questionnaires to measure quality of life in patients with skin diseases is something that Dr Sampogna and her colleagues are continuously seeking to develop further. “From a practical point of view, we are trying to create new, very easy questionnaires because we know in clinical practice it is always difficult to deal with these issues,” she explained. “The first questionnaire that was created was DLQI, which only has 10 items, and so we are creating new instruments that have no more than 10 items because it has to be something very quick.”
Dr Sampogna described an example of a visual measurement that was developed to measure quality of life in psoriasis: the Psodisk. The aim of this is to enable the patient to visualise the extent to which their quality of life has been impacted and then observe the difference when the results are recorded at a later date. It is hoped these kinds of initiatives can help physicians better understand the needs of their patients without taking much of their time. She additionally commented that there should be a greater emphasis on communication and the psychological aspect of diseases in the training of medical doctors.

Hidradenitis Suppurativa
As the study Dr Sampogna presented during the EADV Congress eluded to, the skin disease that can arguably have the greatest impact on a patient’s life is hidradenitis suppurativa. This is a condition that her group are now focussing on to a great extent in their studies as the awareness of it remains limited. “Hidradenitis suppurativa is not very frequent but is more common than people believe. And it has a big symptomatic and psychological impact.” She further outlined that this psychological impact is akin to severe depression, demonstrating the vitality of spreading greater awareness of it. One way the team is now doing this is to make comparative analyses of quality of life in hidradenitis suppurativa with more widespread dermatological conditions, such as psoriasis.







