Abstract
Background: The face is the most common site affected by skin cancer in the body and of the facial skin it is the nose that bears the brunt of the attack.1,2 Cancer resection results in the loss of a significant amount of tissue requiring replacement with either grafts or flaps in many cases. The expectation in nasal reconstruction, whether minor or major, is the restoration of symmetry, contour, colour match, and an overall pleasing result.
Objective: To review the various reconstructive options available for cutaneous defects of the nose following skin cancer resection and to describe outcomes associated with each.
Methods: A literature review was performed using PubMed, books, and websites. These were compiled to create a list of available options for the reconstruction of cutaneous defects on anatomical areas of the nose.
Results: Nasal reconstructive techniques have been evolving over centuries. With our advanced knowledge regarding blood supply and lessons learned from experiences, we have achieved a standard that offers excellent aesthetic results. The benefits and drawbacks of the common flaps are enunciated to provide a basis for decision making as to the best method to yield the optimum result in the reconstruction of cutaneous defects of the nose following resection of skin cancers.
INTRODUCTION
The incidences of non-melanoma skin cancer and melanoma have been increasing over the past decades. Globally each year, there are 2–3 million recorded cases of non-melanoma skin cancer and 132,000 melanomas (as stated by the World Health Organization [WHO]).3 A literature review compiling a list of available options for the reconstruction of cutaneous defects on anatomical areas of the nose was conducted using PubMed, books, and websites, in order to present the various reconstructive options available for cutaneous defects of the nose following skin cancer resection, and their outcomes.
BASAL CELL CARCINOMA
Basal cell carcinoma (BCC) is the most common type of skin cancer, with the sun-exposed areas of the head and neck the most frequently affected. This variety of cancer involves a slow growing tumour and metastasis is extremely rare. There are various effective topical and nonsurgical therapies available for low-risk BCCs. The factors influencing the prognosis of BCC are: tumour size, site, definition of clinical margins, histological subtype, features of aggression, recurrent lesions, and immunosuppression.4
Surgical Excision
Excision is widely used to treat both low and high-risk BCC, and is generally considered to have the lowest overall failure rate, based on the British Association of Dermatologists (BAD) guidelines. Surgical excision is a highly effective treatment for primary BCC with a recurrence rate of <2% reported 5 years following histologically complete excision in two different series.5
Mohs Micrographic Surgery
Pioneered by Frederic Mohs in the 1940s, this technique involves staged resection with immediate surgical margin examination.6 This has the best cure rates; a retrospective review of 720 lesions gave an estimated 5-year cure rate of 98.8% for primary, and 93.3% for recurrent disease.7
Curettage and Cautery
This technique is also known as electrodessication. Curettage is a common form of treatment and is suitable for low-risk lesions.8
Cryosurgery
This method uses liquid nitrogen to cause deep destruction of BCC. Cryosurgery is most useful in the treatment of low-risk BCC9 but also has a role in expert hands for high-risk lesions, especially following curettage.10
Topical Immunotherapy with Imiquimod
Topical imiquimod is approved by The European Medicines Agency (EMA) for the treatment of small BCC using the 5-times per week regimen for 6 weeks.5
Photodynamic Therapy
Topical photodynamic therapy using applied aminolevulinic acid or more recently methyl aminolevulinate, a more lipophilic methyl ester of aminolevulinic acid, is a good treatment for superficial BCC and a reasonable treatment for primary low-risk nodular BCC.
Radiotherapy
Radiotherapy (RT) is effective in the treatment of primary BCC11 and can also be used in cases of recurrent BCC without previous RT.12 In patients who are unwilling to have surgery or are unsuitable candidates for surgery, and have high-risk disease, RT is the treatment of choice.11 RT is avoided, or used only with caution, in patients with basal cell nevus syndrome as it may promote the growth of new BCC.13
SQUAMOUS CELL CARCINOMA
This is the second most common form of skin cancer. It is locally invasive and has metastatic potential. Non-surgical therapies used include: topical imiquimod, intralesional interferon-α, intralesional 5-fluorouracil, and photodynamic therapy.
Surgical Excision
The standard treatment for squamous cell carcinoma (SCC) is surgical excision with predetermined margins. Well-defined tumours <2 cm are excised with a minimum 4 mm margin around the tumour, and high-risk lesions >2 cm in diameter are removed with a wider margin of ≥6 mm.14 Surgery provides cure rates of 95%.15
Mohs Micrographic Surgery
This allows precise definition and excision of primary SCC but involves the long duration of the procedure, higher costs, and trained personnel, hence is considered only for areas where wide excision would result in significant functional impairment.
Curettage and Cautery
Small, slow-growing, well-differentiated SCC treated with this method show excellent cure rates in the hands of experienced physicians.16
Radiotherapy
RT can be considered as an alternative to surgery in inoperable SCC due to concomitant medical problems, a problematic location of SCC, or in the adjuvant setting.17
PRINCIPLES OF NASAL RECONSTRUCTION
The general principles for any reconstructive procedure apply to all nasal reconstruction procedures:
- Replace ‘like with like’
- Consider aesthetic subunits
- the nose consists of nine subunits: the dorsum, two lateral walls, two ala nasi, the tip, two soft triangles, and the columella
- If the defect comprises >50% of the subunit, excising the remaining tissue and reconstructing the whole subunit gives an aesthetically pleasing result
- Compare all measurements with the opposite side to achieve symmetry
- Restore lining and support
The reconstructive methods available for simple cutaneous defects following tumour resection are considered based on the anatomical location.
SKIN GRAFTS AND LOCAL FLAPS
As the nose is the most prominent feature on the face, surgical management of skin cancer on the nose very often necessitates the need for reconstruction using either a skin graft or flap. Primary closure is possible only in very small defects on the dorsum and sidewalls of the nose.
Full Thickness Skin Grafts
Full thickness skin grafts taken from the post-auricular region or supraclavicular area provide the best match but are not suitable when the cartilage or bone is exposed, as the graft requires perichondrium or periosteum to be intact for ‘take’ of the graft to occur. It also does not provide the bulk needed to avoid contour defects. This is used as a common option due to ease of harvest of the graft, a good colour match of the skin, and the simplicity of the procedure. This procedure allows the retention of more characteristics of normal skin including colour, texture, and thickness, and undergoes less contraction while healing compared with split thickness grafts. For defects of the nose where both flap and graft repair may be technically possible, a flap is more likely to result in a superior cosmetic outcome.18
Composite Skin Grafts
Composite skin grafts with superficial layers of subcutaneous tissue provide bulk for a better appearance. A composite graft from the helix including cartilage can be used for ala defect reconstruction. However, there are various simple flaps described in the literature that are as straightforward to do as a graft and provide a better appearance. Flaps are superior in terms of providing an accurate colour match and avoiding contour abnormalities.
The Local Flap
The various simple local flap options described in the literature for reconstruction of defects of the nose were reviewed. The earliest description of pedicled flaps for reconstruction of defects of the face and nose is by Sushruta in India in 600 BC.19 In this account Sushruta described how a template was used to plan a flap for a defect. This is the earliest plastic surgical procedure recorded and hence Sushruta is called ‘The Father of (Plastic) Surgery’.
The abundance of blood vessels on and around the nose provide the basis for the various flaps that can be used for reconstruction. The use of a flap follows the plastic surgical principle of replacing like with like. Local flaps are the most powerful reconstructive tools in the management of cutaneous nasal defects, providing a pleasing aesthetic outcome. In general, local flaps are used for reconstruction of nasal defects <1.5 cm in size. Park20 describes defects >1.5 cm as large defects that are unlikely to be closed by simple local flaps. The donor site can be the nose itself, cheek, glabella, or forehead. Major and complex defects of the nose are beyond the scope of this discussion.
THE ROOT OF THE NOSE AND THE MEDIAL CANTHUS
The Glabellar Flap
The glabella is the area between the eyebrows where there is an adequate quantity of redundant skin to raise a flap and close the donor site directly. Usage of this skin was first described by von Grafe in 1818. The classic glabellar flap is a modification of a V-Y flap which is transposed into the defect; various modifications and variations have later been described. It can be transferred as a rotation flap, a transposition or an island flap, or through a combination of rotation and transposition. The author has noted that a transposition flap from the midline called a finger flap is the simplest to perform (Figure 1A, 1B). An island flap from this area with a subcutaneous pedicle does not have an added advantage and is more difficult to perform. The advantages of performing glabellar flaps include their robust blood supply and reliability to provide a good colour match. However, the thickness of the glabellar skin is more than that of the reconstructed area, causing it to look bulky. Additionally, there will be medial movement of the eyebrows as a result of direct closure.
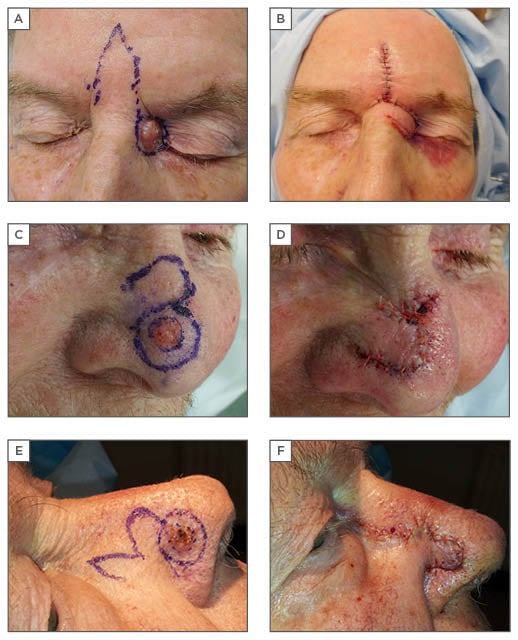
Figure 1: Glabella finger, bilobed, and banner flaps.
A, B) glabella finger flap; C, D) banner flap; E, F) bilobed flap.
A modification of the glabellar flap, termed the bipedicled flap, can be performed from this area based on either side and brought down to cover the defect and donor site closure by inferior advancement of the upper edge, described by Field.21 A recent modification named the ‘flap in flap technique’ by Turgut et al.22 involves an inverted V design with two flaps within; one transposed into the defect and the other advanced in a V-Y fashion.
LATERAL WALLS
The Note Flap
A note flap23 is a very simple flap, ideal for this area; this is a straightforward triangular transposition flap. For a circular defect, two tangents are drawn parallel to the relaxed skin tension line. This provides four options for raising the note flap and the surgeon chooses the best option.
The Rhomboid Flap
The rhomboid flap is a very versatile flap which can be used in many parts of the body. It is suitable for most areas based on adjacent skin laxity. Limberg24 first published the details of this flap and since then there have been various modifications published. Dufourmentel25 modified the design in such a way that the pedicle width is widened. In the original Limberg design, the defect is converted into a rhomboid and the flap is designed as a parallelogram with angles of 120o and 60o; it is possible to raise four flaps from a single rhomboid (Figure 2A, 2B). The choice is made based on the area of maximum skin laxity and orientation of the skin tension lines. The defect from skin cancer excisions are usually circular. The rhomboid flap can be modified to close circular defects by mentally superimposing the rhombus onto the circle.26 The main advantage of this technique is its versatility; the flap can be designed in various directions. However, it is a more complex design and therefore there is wastage of the normal skin in trying to convert the circular defect to a rhomboid.
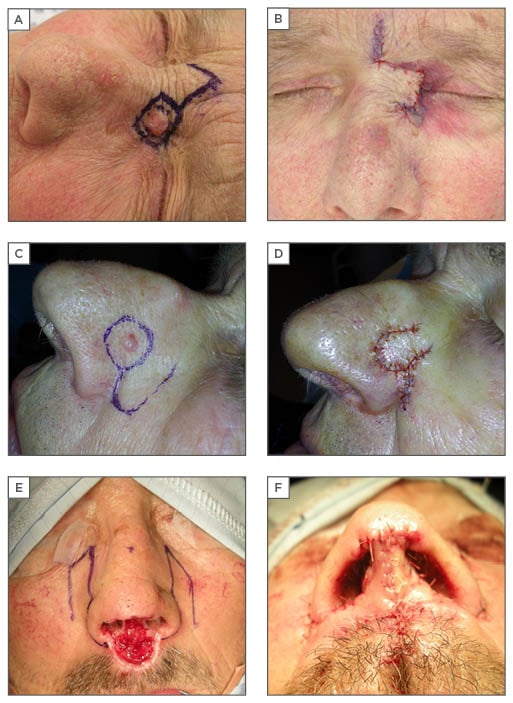
Figure 2: Rhomboid, nasolabial, and nasocheek flaps.
A, B) rhomboid flap; C, D) nasolabial flap; E, F) nasocheek flap.
The Banner Flap
The banner flap is a transposition flap which can be used for small defects. Described by Masson and Mendelson,27 the flap is designed by continuing the edge of the excision along a site of skin laxity on the nose (Figure 1C, 1D). According to the author, this is a very resourceful flap design for the nose and can be applied in different areas based on the direction of the skin laxity. It is extended slightly longer than needed and tapered down towards the end to facilitate closure. Elevation of the flap is carried out just above the nasal musculature, the flap trimmed to size, and inset. This is a simple flap that requires a simple technique however it is not suitable for the lower third of the nose as there is less tissue available. There is also a tendency for pin cushioning and dog ear formation.
The Bilobed Flap
This double transposition flap was first described by Esser in 1918.28 Modification of the bilobed flap by Zitelli29 made it an ingenuous technique for reconstruction of defects of the caudal aspect of the nose.29 He reduced the pivotal angle from 180o to 90o, thus minimising donor site distortions which gives a good result (Figure 1E, 1F). Its use however is restricted by the site and size of the defect. Ideally these flaps are suited for small defects <1.5 cm on the distal third of the nose. The first flap is designed to be the same size as the defect at 45o to the defect and the second flap smaller than the defect at 45o to the first flap. The design can be modified according to the site of the defect as a 180o flap with the two flaps at 90o to each other. Wide undermining of both the donor and defect sites helps to avoid pin cushioning. A detailed description with pictures on the execution of this flap is given by Chu and Byrne.30 This technique provides bulk in an area where skin and subcutaneous tissue is inherently thick and therefore its appropriate execution can give excellent results. It does carry several disadvantages including size limitation and distortion of the nasal tip, either elevation or notching, if used to reconstruct the extreme tip.
The Trilobed Flap
The trilobed flap31 allows application of the principle of the bilobed flap for the reconstruction of defects of a wider range of sizes and locations. This technique is different from the bilobed flap in that it uses a third lobe. This tertiary flap is at 45o to the second flap and smaller.
The Dorsonasal Flap
The dorsonasal flap by Rieger32 is a rotation advancement flap of dorsal and glabellar skin based superolaterally for defects of the middle and lower third of the nose (Figure 3A, 3B). It is elevated in a submuscular plane to protect the blood supply.
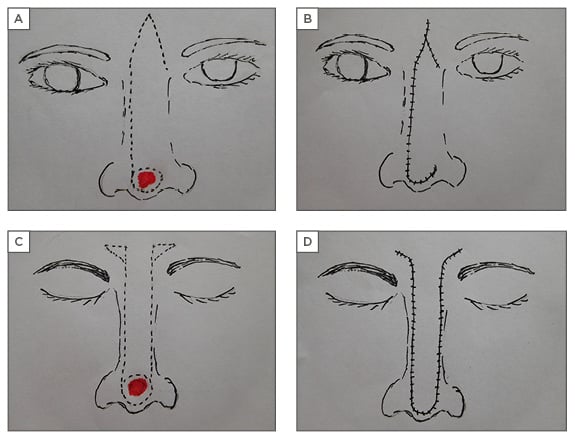
Figure 3: Dorsonasal and rintala flaps.
A, B) dorsonasal flap; C, D) rintala flap.
The Cheek Advancement Flap
These flaps are raised at the subdermal level and advanced to cover defects on a lateral aspect. This could cause a tenting effect on the medial cheek. The author uses a 5.0 polypropylene suture to anchor the dermis of the flap to the periosteum of the maxilla to maintain the contour of the nasocheek junction.
The Nasolabial Flap
This flap utilises the laxity of the nasolabial area to reconstruct defects of the side wall and lower third of the nose. The donor scar is easily hidden in the nasolabial fold. The colour match, proximity, and robust blood supply makes it a very appealing flap for reconstruction of nasal defects. Though it can be used for side wall, ala, and columella, it is best suited for the ala as the bulk recreates its natural shape. It can be designed as a transposition flap or as an island flap with subcutaneous pedicle. This is usually superiorly based (Figure 2C, 2D). When performed as a two-stage procedure, the pedicle division is usually done at 3 weeks.
The technique utilises the abundant tissue available adjacent to the nose where there is good vascularity. In addition, the donor site scar can be hidden in the nasolabial fold. However, it can cause distortion of the nasolabial sulcus and the bulk tissue can be excessive for side wall reconstruction. It has a tendency for trapdoor and pin cushioning and requires a staged procedure at times. Hair-bearing skin will be transferred to the nose if the flap is elevated low in male patients. The most common problem encountered by the author with the nasolabial flap initially has been the bulky appearance even for the ala; this has been solved by thinning the flap adequately at the time of harvest. It is safe to do so as this is a well vascularised flap.
THE ALA
The convexity and abundance of fibrofatty tissue in the ala nasi makes it a unique structure.
The Bilobed Flap
The bilobed flap can be used for reconstruction of small defects of the nasal ala.
The Nasolabial Flap
The ideal flap for ala reconstruction is the nasolabial flap as it can recreate the bulk and shape of the ala. Moreover, the tendency for pin cushioning delineates the ala subunit when used for whole subunit reconstruction. Though the ala has no cartilage, when reconstructing larger defects of the ala, a conchal cartilage graft is required as a framework to provide support and prevent collapse of the external nasal valve.
THE TIP AND SUPRATIP
The Banner and Bilobed Flaps
The banner flap and bilobed flap can be used for reconstruction of the tip. The bilobed flap is more suited for this region than the banner flap as the skin is thick and sebaceous, and transposition of a single flap can result in secondary distortion.
The Modified Nasalis Flap
The modified nasalis flap involves elevating bilateral transposition flaps from the lateral aspect of the defect on the tip.33 An incision is made along the superior alar sulcus extending to the nasojugal fold and a back cut is then made in the nasojugal fold, parallel to the nasolabial fold. The flap is transposed in an anterior and caudal direction. This technique is a single-stage procedure and donor site scars are concealed, however alteration of the contour of the tip does occur.
The Rintala Flap
The rintala flap is a long advancement flap based on the mid forehead skin. Burrow’s triangles (Figure 3C, 3D) are excised bilaterally lateral to the base of the flap.34 A modification places the triangular resections above the medial canthus. Using this technique, like is replaced with like and the nasal skin itself is advanced, however, distal ischaemia and necrosis occur occasionally and the procedure does result in a slight shortening of the nose.
THE COLUMELLA
This is a complex area to reconstruct due to its position and anatomy.
The Nasolabial Flap
This requires a two-stage procedure for columella reconstruction as the position of the columella is distant to the donor area. Alternatively, a subcutaneous pedicle flap from the nasolabial area can be used but adds bulk in the route of transfer.
The Extended Abbe Flap
The extended abbe flap consists of an extension of the distal portion of the abbe flap over the chin to create the neocolumella.35 This is a two-stage procedure that can be used if the upper lip also requires reconstruction.
The Nasocheek Flap
The nasocheek flap, as described by Akbaş et al.,36 utilises the skin of the nasojugal area to reconstruct the columella. This has the advantage that the thin and pliable skin of the nasojugal area allows good contouring. The addition of a strut of cartilage for columella support, as reported by the author (Figure 2E, 2F), gives an excellent result.37 This is a simple, single-stage procedure with no donor site morbidity, however there can be collapse of the columella without cartilage support.
Elbaz’ Flap
Tissue taken from the nostril edge based on the medial aspect; Elbaz’ flap is useful in people with a broad nostril rim.38
The Forehead Flap
This flap is the workhorse for nasal reconstruction. This is called the ‘Indian method’ as the technique was practised by the Kumhar caste in India for nasal reconstruction as far back as 1,000 BC.39,40 Even today, the forehead flap remains the gold standard for nasal reconstruction. A forehead flap is required when the defect is large, requires replacement of the support or lining, or is adversely located within the infratip or columella.41 As this review is not on complex defects or complex procedures, details on the forehead flap are beyond the scope of this article.
CONCLUSION
There are several local flaps described for reconstruction of partial cutaneous defects of the nose. This article provides a review of some of the very useful and common surgical techniques used in the reconstruction of such defects. The decision on which flap to use depends on the site and size of the defect, skin type, sex, age, tobacco use, and surgeon’s preference. Having a multitude of options in one’s armamentarium helps to overcome the limitations associated with one or the other. Each case should be considered unique, and reconstruction tailored to fit the defect and patient expectations. The ultimate outcome of the procedure depends on careful assessment, accurate planning, and meticulous technique.







