Abstract
Background: Pemphigus is a group of rare autoimmune blistering diseases affecting the skin and mucous membranes. Pemphigus foliaceus (PF) is known to be relatively benign than the other forms of pemphigus.
Methods: The authors carried out a single-centre retrospective study of 40 patients with PF and 125 patients with pemphigus vulgaris (PV) over a 30-year period. The aim was to compare the course of these two major variants.
Results: Both populations shared similar age, sex ratio, and treatment received. This investigation showed that relapses were more frequent in the group of PF, whereas the PV group needed a higher dose of corticosteroids to control the disease, a higher mortality rate, and complications were documented in this group. Severity, remissions, and mean duration of the disease were the same in both groups.
Conclusion: This investigation arises some doubts concerning the relative mildness of PF. Despite the improvement of the prognosis of pemphigus through the use of immunosuppressive therapy, few studies have been interested in comparing the clinical course of treated PF and PV. In the authors’ experience, PF should be treated as PV, as they may share a mutual evolutive profile. Further investigations are needed to define if the prognosis of PF depends on epidemiological, environmental, and genetic factors, including the optimal therapeutic management of this disease.
Key Points
1. While rare, both pemphigus vulgaris (PV) and pemphigus foliaceus (PF) are life-threatening autoimmune intraepidermal blistering diseases.2. In this comparative study, the authors compared PV and PF to determine the clinical course for treating both conditions and who is the most affected (in regard to age, sex, and geographical location).
3. The authors’ report indicated that patients with PV needed higher doses of corticosteroids to control their disease than patients with PF.
INTRODUCTION
Pemphigus encloses a group of autoimmune intraepidermal blistering diseases of the skin and mucous caused by the loss of intraepidermal adhesions. It is a rare and life-threatening dermatosis. Two major subtypes have been described: pemphigus vulgaris (PV) and pemphigus foliaceus (PF). The objective of this analysis is to compare pemphigus vulgaris and pemphigus foliaceus, concerning demographic data, clinical course, and prognosis. Thus, the authors are sharing their experience in the management of these two major variants.
PARTICIPANTS AND METHODS
The present study is a retrospective analysis of patients with pemphigus hospitalised in the University Hospital Ibn Sina in Rabat, Morocco, over 30 years (1991–2020). The authors included only PV and PF based on clinical, histological, direct immunofluorescence, and immunological features (indirect immunofluorescence). Following the consensus statement on pemphigus,1 all medical files have been analysed regarding age, gender, duration, the severity of the disease, pemphigus disease area index (PDAI) score, indirect immunofluorescence level, treatment modalities, complete remission rate off therapy, healing time, relapses, patients lost to follow-up, complications, and mortality rate. Data analysis was conducted using SPSS version 20.0 (IBM, New York City, New York, USA). Ethical approval for this study was granted by the Research Health Committee of Ibn Sina University Hospital at the Mohammed V University in Rabat, Morocco.
RESULTS
A total of 302 patients were investigated during the research period, and only the cases of PV (125) and PF (40) were considered. Table 1 includes the main features of the two groups. There were no major differences between PF and PV in terms of age (median age: 52 versus 53 years), gender (50% female versus 39% male), median illness duration before initiating therapy (13.0 versus 13.4 months). The PDAI score was severe in 36 cases in the PF group versus 102 cases in the PV group. The PV group showed more cases of positive indirect immunofluorescence in contrast to the PF group (76 versus 16 cases).
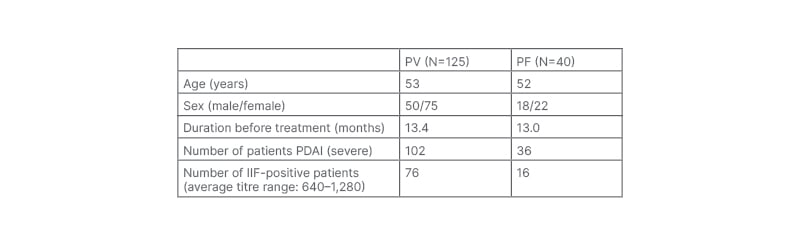
Table 1: Pemphigus demographic data and immunologic findings.
IIF: indirect immunofluorescence; PDAI: pemphigus disease area index; PF: pemphigus foliaceus; PV: pemphigus vulgarise.
All patients with pemphigus received oral prednisone at the dose of 1.5 mg/kg per day. The primary outcome of the initial treatment regimen showed that 95 cases of the PV group required a higher dose of prednisone (2 mg/kg/day) to control the disease. Adjuvant therapy was administered to the two groups (16 PF versus 84 PV cases). In the PF group, additional treatments used were azathioprine in 13 cases, dapsone in six cases, methotrexate in one case, and rituximab in one case. In the PV group, additional treatments used were azathioprine in 36 cases, rituximab in 10 cases, cyclophosphamide in one case, and dapsone in one case. In this study, no differences were noted in the two groups regarding maintenance treatment (the drug and its dosage), and no patient was required to stop the therapy.
Table 2 highlights the course and the follow-up of patients with PF and PV. The rate of complete remission off therapy was higher in patients with PF (52.5% versus 36%), and the healing time was similar between the groups (2.7 versus 3.2 months). However, the PF group showed a greater tendency to recurrence than the PV group (42.5% versus 29.6%), over a longer period (74 versus 47 months). Concerning death and complications, patients with PV were more concerned. The mortality rate was 17.6% versus 2.5%, and iatrogenic complications were 45.6% versus 35%, yet the PF group marked an increased level of complications. In this study, 17 cases in the PF group and 37 in the PV group were lost to follow-up (Figure 1).
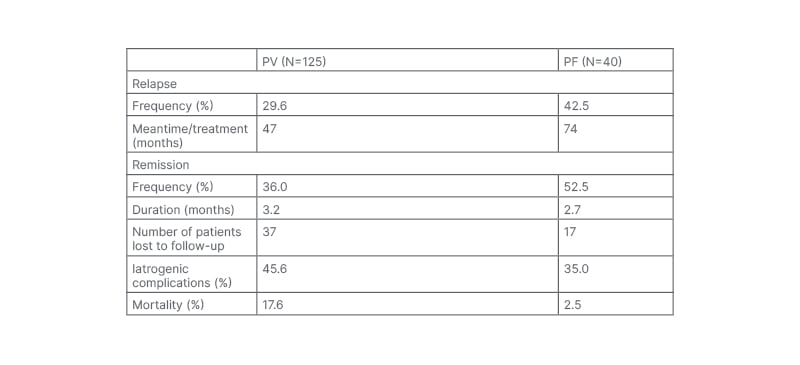
Table 2: Pemphigus clinical course.
PF: pemphigus foliaceus; PV: pemphigus vulgaris.
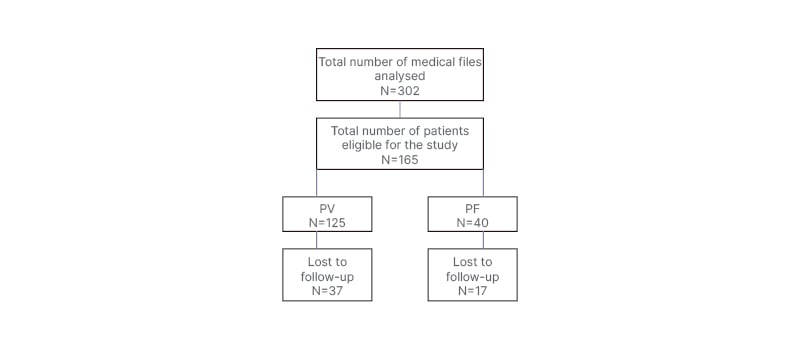
Figure 1: Patient analysis flow chart.
PF: pemphigus foliaceus; PV: pemphigus vulgaris.
DISCUSSION
PV and PF are intimately connected as autoimmune blistering diseases. Nevertheless, their dissimilarities are based on clinical and immunohistological features. In PV, IgG autoantibodies against the DSG3 and in some cases DSG1 cause a suprabasal cleft by the loss of keratinocyte cell adhesion (acantholysis). Lesions occur on the oral mucous membranes as erosions, and on the healthy-looking skin as flaccid blisters. PF is frequently described as fragile cutaneous blisters and erosions appearing primarily on seborrheic areas (e.g., scalp, face, and upper trunk) which might disseminate. It is characterised by the production of antibodies directed against DSG1, creating a cleavage within subcorneal cells.2
The geographical distribution of pemphigus is unequal. The annual incidence of PV ranges from 16.1 /million in Jerusalem to 0.76 /million in Finland.3 PF is less common than PV; the annual incidence in Western Europe varies between 0.5–1.0/million4 to 6.7/million in Tunisia.5 Two forms have been described in Brazil. The typical PF seen around the world sporadically, without evidence of geographical clustering, and the endemic occurring in certain regions of Brazil may be triggered by environmental factors, known as fogo selvagem. Fogo selvagem is endemic in Brazil, occurring mainly in middle age, neighbours, and family members as it follows the course of streams and creeks. PF is also endemic in other South American countries, and in Tunisia. In a recent Moroccan study,6 PV was the most reported form (50.3%), with fewer cases of PF (28.8%). In this analysis, PV was more prevalent than PF. These results are in line with existing literature. While few studies have been interested in comparing the two major variants of pemphigus, the authors’ work focused on analysing their clinical course. The most interesting findings were the absence of significant differences concerning demographic patterns, such as age and gender. In the northwest region of Africa, the disease affects those in the fifth decade6,7 and has a female predominance, as reported in the majority of epidemiological studies around the world; this supports the authors’ findings. However, in northern Colombia, endemic PF has been reported as more common in males (95%), which speculates that the epidemiology of PF may be attributed more to environmental triggers than to race and ethnicity.8
The mean duration of the disease before treatment was long: 13 months, as reported by the Tunisian study.7 In fact, it takes approximately 10 months and five doctors to make the diagnosis of PV.9 The delay in diagnosis is probably due to the lack of recognition of the disease among primary care physicians, especially in PV when mucosal lesions are predominant, or in the case of delayed skin manifestations. Patients tend to see specialist doctors such as dentists, otolaryngologists, gynaecologists, and urologists, who may evoke other differential diagnoses, leading to a late referral to dermatologists. In addition, in both PV and PF, intact blisters may not be seen, which may mislead even those who are familiar with these diseases.
Both groups had a severe PDAI score, which may be explained by area of skin involvement in PF, and mucosal lesions in PV. As for the time to heal, there were no statistical differences between the two groups. These findings are in line with the results reported by Zaraa et al.7 Azathioprine was the most used adjuvant therapy in the authors’ practice, either in the PV or in the PF group, while dapsone was used as second-line treatment in the study of Goon and Tan.10
The authors’ report showed that PV needed higher doses of corticosteroids to control the disease, and more cases of complications and mortality have been reported in this group as documented by Goon and Tan,10 and an Israeli study.8 Kridin et al.8 have found that the median overall survival among patients with PF was longer than patients with PV (14.0 versus 10.1 years; p=0.05), and the highest mortality rate was observed in the PV cohort. Even though these results sharpen the fact that PV is more life-threatening disease, and PF has a more favourable outcome, patients with PF presented a high tendency to relapse and a considerable rate of complications, suggesting that PF and PV may share the same course as reported by Zaraa et al.7 and Dehen et al.11 For instance, Jelti et al.12 have reported that the mortality rate in their research was mainly observed in elderly patients with a median age at death of 87.4 years for patients with PF versus 82.4 years for patients with PV. Interestingly, the highest mortality rate in their study concerned patients with PF (31.1% versus 19.4%), which was explained by the high proportion (32.8%) of patients older than 75 years among those with PF.12
This investigation, therefore, arises some uncertainty concerning the mildness of PF, as its prognosis may depend on geographic areas, genetic background, and environmental factors.
Untreated pemphigus had a mortality rate >70%; corticosteroid use and immunosuppressive therapy have narrowed the difference in morbidity and mortality.13 Today, mortality is mainly due to treatment-related complications, older age, cardiovascular comorbidities, and the level of autoantibodies.14
In this study, flaws and barriers concern the design of the research as a retrospective single-hospital study, and the absence of dosage of the anti-desmoglein antibodies, as ELISA testing is not available in the authors’ hospital, and is relatively expensive in private practices.
CONCLUSION
Pemphigus being the most common indication for hospitalisation in the authors’ department led them to conduct the first comparative study in Morocco of its two main variants. Their research advocates that PF and PV share similar evolutive profiles. However, prospective, multicentre trials based on demographic profile, genetic analysis, and prognostic factors are, therefore, needed to enhance the knowledge of this pathology in Morocco, to facilitate patient stratification, and to design personalised therapeutic plans in the hospital setting.






